Reducing Catheter Associated Blood Stream Infections in Pediatric ICUs
advertisement

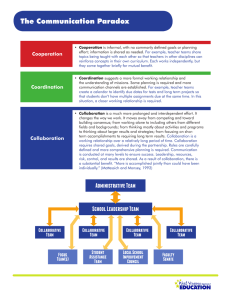
Reducing Catheter Associated Blood Stream Infections in Pediatric ICUs The Collaborative Model – key to success? Richard J. Brilli, MD Academy of Health Chief Medical Officer 2009 Annual Research Congress Nationwide Children’s Hospital Professor, Pediatrics The Ohio State University College of Medicine Outline • Why CA-BSI? • What is CA-BSI and Why is it hard to eradicate? • Brief Summary of Outcome Data • Why has this Network (Collaborative) been successful Every system is perfectly designed to produce the results it gets. If you do not change the system you will continue to get the same results Don Berwick, Institute for Healthcare Improvement and many others • CA-BSI is high morbidity, high mortality, high cost 250,000 cases per year in US 80,000 cases per year in ICU’s Attributable mortality: 9-25% Attributable cost: $25,000-$45,000 • Regulatory - Oct08: CMS no longer pays hospital for CA-BSI event • To date, 19 States mandate at least hospital reporting CA-BSI data to CDC • CA-BSI – Catheter-associated Blood Stream Infection • Bacteremia (bugs in the blood) in the presence of a centrally located venous catheter, in the absence of another source of the bacteremia besides the catheter Eliminating CA-BSI a function of Pathophysiology Skin contamination (insertion & during maintenance) Bacterial migration through subcutaneous tissue down catheter track Full Sterile Barrier - Operator Full Sterile Barrier at Insertion How to Fix relates to CA-BSI Pathophysiology External catheter colonization from within the bloodstream Eliminating CA-BSI a function of Pathophysiology Intraluminal & Extraluminal catheter contamination / colonization Maintenance Care Focus Outcome Data Collaborative GOALS and AIMS Outcomes Measures 50% decrease in CA-BSI rate per 1,000 line days for 2 consecutive quarters within 6 months of reliably implementing infection reducing strategies (ACHIEVED) Eliminate CA-BSI across 30 PICU’s (FAILED) Process Measures 100% of units adherent with insertion and maintenance practice changes – not done before (ACHIEVED) Measure compliance with bundle elements - Practices followed 95% of the time (ACHIEVED at 90%) •Building Block / Culture Goals – Improvement in Mean Safety Climate Score (IN PROCESS) – Every clinician involved in line care receives education (ACHIEVED) CHARTER GOALS and SPECIFIC AIMS Spread - Critical Care Engage more than 100 pediatric critical care physicians in network activities within the first year (ACHIEVED) Disseminate to the ~330 PICUs in the US by the end of the third year of the project (FAILED – up to 60, working on another 20 units) Program Model to Assist Recertifying Subspecialists Part IV Maintenance of Certification for Pediatric Subspecialists (ACHIEVED) Project approved by ABP (ACHIEVED) Control Chart: Monthly BSI Rates - Baseline to Present Phase I Apr09 NHSH pooled mean = 2.9 AJIC Nov 2008 & dropping 254,872 line days - 29 PICUs over 2.7 yrs Baseline rate – 5.4; current – 1.6 70% decrease in BSI rate Monthly BSI Rates: Oct 06 – Apr 09 Phase I – Apr09 Apr09 = 1.6 rate Catheter Care Bundle - Insertion • Hand Washing • Chlorhexidine Scrub at insertion site • No Iodine use at insertion site • Insertion Checklist • Prepackaged or Filled Insertion cart • Polyurethane or teflon catheters only • Insertion training for all operators Make it Easy to follow all steps and do the Right Thing Insertion Cart Kosair Children’s Hospital Catheter Care Bundle - Maintenance • Daily Assessment of Line necessity & Integrity • Hand Hygiene before Line Care • Catheter Site Care – dressing changes; prepackaged dressing change kits • Catheter Cap/Hub/Tubing care NACHRI CA-BSI Elimination Collaborative Dressing Change Kit Kit Contents NACHRI CA-BSI Elimination Collaborative NACHRI CA-BSI Elimination Collaborative Cap Change Kit Cap Change Kit Contents Aggregate Monthly Bundle Compliance Data Oct 06 – Feb 09 Phase I – Feb09 Sustained Reliable Performance 29 PICUs CA-BSI Rates, Insertion and Maintenance Compliance - Pre-and PostCollaborative Intervention Periods 100,000 Central Line Days Insertion Compliance Rate Maintenance Compliance Rate Pre-Collaborative Interventions CA-BSI Rate Post-Interventions Infection Rate vs. Insertion Compliance Insertion compliance ↑es, infection rate ↓es; but not statistically significant association Infection Rate vs. Maintenance Compliance As Maintenance compliance ↑es, infection rate ↓es sharply Highly statistically significant association (p<0.008) TAKE HOME MESSAGE RE: Outcomes PICU CA-BSI Collaborative impact: >741 CA-BSIs prevented >$25 million dollars saved > 89 deaths prevented Reliable implementation of Maintenance care practices New Knowledge for children’s healthcare Measure compliance with care practices Model is sustainable and can create new pediatric evidence Why Has this Network been Effective? • The Collaborative – Just Getting Together Absent “Perserveration with Perfection” Absent “Paralysis of Analysis” • Transparency of Data Rapid Exchange of new ideas or best practice; Key to moving quickly • Standard Method for Improvement Reliable Implementation - measured Data Driven but not Data Paralyzed – planned experimentation Collaborative Model – Organization Sponsors and Contributors Key Sponsors of Collaborative – – – – – NACHRI American Board of Pediatrics CHCQ: Center for Health Care Quality Johns Hopkins Bloomberg School of Public Health Johns Hopkins Quality and Safety Research Group Involved Parties – CDC: Centers for Disease Control – NOC: National Outcomes Center – VPS: Virtual PICU Performance System Collaborative Leadership from Diverse Institutions and Disciplines – Content experts AND Process improvement experts Improvement Collaborative Model Select Topic Participating PICU’s Prework Printed Reports P P Changes Strategies A D A S Design Meeting Planning April 19, 06 LS 1 Sept 06 D S LS 2 Jan 07 Spread LS 3 Phase II Oct 07 Jul 08 Decision to focus on Maintenance Care What Do We Think has Made this work • The Collaborative – getting together Absent “Perserveration with Perfection” Absent “Paralysis of Analysis” • Transparency of Data Rapid Exchange of new ideas or best practice; Key to moving quickly • Standard Method for Improvement Reliable Implementation - measured Data Driven but not Data Paralyzed – planned experimentation One Bundle – Two Parts Insertion & Maintenance • Where did the bundles come from? Pediatric literature (sparse) Extrapolated from adult literature (esp. for “insertion”) Pathophysiology-driven (esp. for “maintenance”) Consensus opinions of experts and thought-leaders • Uncertain if these bundles were “best practice” But if these bundled practices were standardized & reliably implemented, then… • Initial PICUs could assess impact on BSI rates • Additional Maintenance practices could be “tested” What Do We Think has Made this work • The Collaborative – getting together Absent “Perserveration with Perfection” Absent “Paralysis of Analysis” • Transparency of Data Rapid Exchange of new ideas or best practice; Key to moving quickly • Standard Method for Improvement Reliable Implementation - measured Data Driven but not Data Paralyzed – planned experimentation 29 Collaborating PICUs PICU CA-BSI Phase II Members Levine Children’s Hospital (NC) Texas Children’s Hospital – PICU (TX) Methodist Children’s Hospital of South Texas (TX) Texas Children’s Hospital – CVICU (TX) Children’s Hospital of Philadelphia – PICU/PCU (PA) CHRISTUS Santa Rosa Children's Hospital (TX) Children’s Hospital of Philadelphia – CICU (PA) Children’s Medical Center at Presbyterian Hospital (NM) Medical City Children’s Hospital (TX) Children’s Hospital (Denver) – PICU and CICU (CO) Children’s Hospital of Michigan (MI) Cabell Huntington Hospital (WV) Maria Fareri Children’s Hospital (NY) Arnold Palmer Hospital for Children – CICU (FL) Yale-New Haven Children’s Hospital (CT) Arnold Palmer Hospital for Children – PICU (FL) Children’s Hospital, Cleveland Clinic (OH) CS Mott Children’s Hospital University of Michigan – CICU (MI) Children’s Hospital of Central California (CA) Children’s Hospital of Alabama (AL) Schneider Children’s Hospital (NY) SSM Cardinal Glennon Children’s Medical Center (MO) Riley Hospital for Children (IN) Children’s Medical Center Dallas - PICUs (TX) Univ of Virginia Children’s Medical Ctr (VA) Children’s Medical Center Dallas – CICU (TX) Deaconess Hospital (IN) Nationwide Children’s Hospital – PICU (OH) Mary Bridge Children’s Hospital (WA) Nationwide Children’s Hospital – CICU (OH) Transparency Barriers & Excuses • Typical excuses I have used and have heard used: The data is wrong – inconsistent definitions Our patients are sicker (old severity of illness argument) Our hospital is busier than yours Our patient population is different than yours Your data makes our unit look bad ! My CEO, CFO, hospital attorney say I can’t share data It can’t be true I am in a world famous center • Probably all relevant and maybe even true • What if I could go to your website and learn from you because you are doing it better? Some systems really are better than others We can learn from the best As a result – all will improve more quickly 35 01/04 n=13 02/04 n=12 03/04 n=12 04/04 n=14 05/04 n=14 06/04 n=14 07/04 n=14 08/04 n=14 09/04 n=15 10/04 n=17 11/04 n=17 12/04 n=17 01/05 n=19 02/05 n=20 03/05 n=20 04/05 n=18 05/05 n=19 06/05 n=18 07/05 n=19 08/05 n=19 09/05 n=19 10/05 n=18 11/05 n=18 12/05 n=18 01/06 n=21 02/06 n=21 03/06 n=21 04/06 n=20 05/06 n=20 06/06 n=21 07/06 n=19 08/06 n=19 09/06 n=19 10/06 n=22 11/06 n=22 12/06 n=21 01/07 n=25 02/07 n=24 03/07 n=25 04/07 n=25 05/07 n=25 06/07 n=24 07/07 n=25 08/07 n=26 09/07 n=26 10/07 n=27 11/07 n=27 12/07 n=27 01/08 n=27 02/08 n=27 03/08 n=27 04/08 n=15 BSI Rate NACHRI Collaborative Variation BSI Rates by Unit BSI Rate By Month 40 Systems are perfectly designed to get the results they get and by the way some systems are better designed than others, for example ….. Max 75th Percentile Median 25th Percentile Min 30 25 20 15 10 5 0 Data entered as of 1/16/2007 (updated October and November) December 2006 CA-BSI Rate per 1000 Line Days - Ordered by Rate Note: October was the first month of data submission; November the first month of full verification of number of events 25.0 20.0 What would you do if this was your hospital? Rate 15.0 10.0 OctAgg (n=25) 5.0 0.0 Nov Agg (n=25) NovAgg (n=29) DecAgg (n=29) Wis Cin Ark Oct Nov Nov Dec Unit Unit Unit Unit May Unit Unit Kos Unit Unit Unit Sea Unit Unit Unit Hop Unit Unit Unit Unit Unit Unit Unit Unit Unit Unit con cinn ans Agg Agg Agg Agg 18 3 27 15 o 11 20 air 16 4 23 ttle 9 2 6 kins 10 13 17 19 22 25 26 30 31 5 sin ati as (n= (n= (n= (n= 23.3 18.0 10.8 8.7 8.1 5.8 5.3 4.2 3.8 3.6 3.4 2.6 2.4 2.3 2.0 0.0 0.0 0.0 0.0 0.0 0.00 0.0 0.0 0.0 0.0 0.0 0.0 0.0 5.1 3.5 3.4 3.0 Line Days 86 222 185 231 123 172 375 236 264 563 292 389 425 429 498 368 192 302 259 265 367 93 102 202 329 313 236 252 6,44 6,30 7,35 7,79 Rate Infections 2 4 2 2 1 1 2 1 1 2 1 1 1 1 1 0 0 0 0 0 0 0 0 0 0 0 0 0 33 22 25 23 What Do We Think has Made this work • The Collaborative – getting together Absent “Perserveration with Perfection” Absent “Paralysis of Analysis” • Transparency of Data Rapid Exchange of new ideas or best practice; Key to moving quickly • Standard Method for Improvement Focus on Reliable Implementation measured Data Driven but not Data Paralyzed – planned experimentation Model for Improvement What are we trying to accomplish? How will we know that a change is an improvement? Significant time devoted to Teaching improvement science – very important. What change can we make that will result in improvement? Act Plan Study Do Key Driver Diagram - Analysis Outcomes Key Drivers Intervention/Change Concepts What Do We Think has Made this work • Collaborative Model • Data Transparency • Standard Method for Improvement Collaborative Faculty Co-Chairs: Richard J. Brilli, MD; Marlene Miller, MD Faculty: Debra Campbell, RN; Charlie Huskins, MD; Michelle Moss, MD; Matthew Niedner, MD; Tom Rice, MD; Debra Ridling, RN QI – Informatics: Mitch Harris, PhD; Peter Margolis, MD; Steve Muething, MD; Jayne Stuart, RN NACHRI Staff: Mary Kelly, Gloria Lukasiewicz, RN CA-BSI Collaborative Structure NACHRI Project Staff Clinical, Statistics Improvement and Data Science and Operational Mitch Jayne Gloria Mary K JHU SOPH JHU-SAQ CHCQ STEERING COMMITTEE Chairs: Brilli, Miller Members: Huskins; Rice; Campbell; Ridling; Moss; Niedner; others from Phase II Phase I 29 units Began 9/2006 Phase II 33 units Began 5/2008