Cardiac Contractility
advertisement

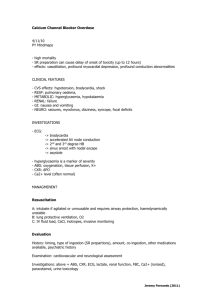
Cardiac Contractility Dapo Odujebe, MD Toxicology Fellow NYC Poison Control Center Overview Review & Cases Cardiac Electrophysiology Cardiac Contractility Cardiac Medications • Overdose Management Questions? Case #1 45-year old woman PMHx s/f depression presents to the ED after allegedly ingesting all of her anti-HTN medication. Prescription filled 3 days prior for 30 tablets of diltiazem CD 240 mg. Patient alert & oriented, mildly diaphoretic and complaining of generalized weakness. Case #1 Vital signs: • BP: 76/36, HR: 46, RR: 14, Temp: 98.6 • pOx: 100% RA, AccuChk: 154 Rest of physical examination is benign. Patient placed on a cardiac monitor, O2 via nasal cannular and IV access established. Case #1 What is the next step in her management? Case #3 An 86-year old woman presents with increased confusion and vomiting. Per family, she’s had increasing weakness, nausea & anorexia over the last 3 days. PMHx: • hypertension • congestive heart failure (CHF) • diabetes mellitus Medications: • • • • • hydrochlorothiazide digoxin furosemide enteric-coated aspirin metformin Case #3 In the hospital, she is alert, but oriented only to person. Vital signs are normal, except for a heart rate of 46 beats/minute. She weighs 143 lbs (65 kg). Her physical examination demonstrates: • bibasilar rales • irregular S1, S2 with a S3 gallop • bilateral LE 2+ pitting edema, up to her shins Case #3 ECG: • atrial flutter with variable block • ventricular rate of 40-50 beats/minute with occasional premature ventricular contractions (PVCs). Laboratory results were within limits except: • potassium - 3.2 mEq/L • creatinine - 1.6 mg/dL • glucose - 235 mg/dL Initial digoxin serum concentration (SDC): • 3.4 ng/mL (> 6 hours since last dose). Case #3 What is the next step in her management? Cardiac Electrophysiology Cardiac Electrophysiology Actions potentials • SA node • Cardiac muscle (atria, ventricles & Purkinje fibers) Channels • Ca2+ channel • β-adrenergic receptor • Na+/K+-ATPase Pacemaker Cell Cycle Phase 0 Phase 3 0 mV -50 mV -70 mV Phase 4 Ca2+ Phase 4 Action potential (SA Node) Pacemaker of the heart Unstable resting potential • Exhibits automaticity • AV node & His-Purkinje system are latent pacemakers Phase 1 & 2 are not present in pacemaker action potentials Cardiac Muscle Cell Cycle Phase 0 Phase 1 Phase 2 +30 mV 0 mV Ca2+ Phase 3 -70 mV -90 mV Phase 4 Resting Potential Na+ channel Voltage dependent L-type Ca2+ channel 2 Na+/K+ ATPase K+ 3 Na+ K+ channel(s) Ca2+ 3 Na+ β-adrenergic receptor Na+/Ca2+ exchanger SR (Mitochondria) Heart muscle Ryanodine receptor Na+/K+ ATPase Na+/Ca2+ Antiporter Representative Cardiac Cell Cardiac Contractility Contractility Intrinsic ability of cardiac muscle Also called ‘inotropism’ or ‘inotropy’ Related to the intracellular [Ca2+] Inotropic agents • positive: increase contractility • negative: decrease contractility Factors Increasing Contractility Increased intracellular [Ca2+] • increased heart rate • cardiac glycosides (e.g. digoxin) Stimulation of β1-adrenergic receptor • sympathomimetic agents • catecholamines Contractility - Other Factors Chronotropy • rate of contraction • also affected by intracellular [Ca2+] Dromotropy • rate of impulse conduction • noted particularly at AV node Cardiac Medications & Receptors Cardiac Medications Some examples: • Ca2+ channel antagonists/blockers • β-adrenergic antagonists/blockers • Cardiac glycosides (digoxin) 2+ Ca Channel Antagonists Calcium Channel Cardiac calcium channels • L-type calcium channel • ryanodine (RyR2) calcium channel located on the sarcoplasmic reticulum Critical for: • conduction velocity (AV node) • duration of depolarization • cardiac muscle contraction Ca2+ Channel Antagonists Block the L-type calcium channel • negative inotropy in cardiac muscle decrease available intracellular Ca2+ • negative chronotropy in pacemaker cells • negative dromotropy at the AV node • relaxation of vascular smooth muscle decreased afterload decreased systemic blood pressure increased coronary vascular dilatation Ca2+ Channel Antagonists Phentylalkylamines • e.g. verapamil Benzothiazepines • e.g. diltiazem Dihydropyridines • e.g. nifedipine Diarylaminopropylethers • e.g. bepridil Tetralene Derivatives • e.g. mibefradil Ca2+ Channel Antagonists Overdose of CCB • extension of therapeutic effects Lose their selectivity (mostly) • Negative inotropy (bradycardia) • Negative chronotropy (hypotension) • Vasodilation (hypotension) • Negative dromotropy (AV blocks, brady) • +/- hyperglycemia (depressed insulin) CCB = calcium channel blocker β-Adrenergic Antagonists β-Adrenergic Receptors There are 3 known subtypes of βadrenergic receptors, namely β1, β2 & β3. The human heart has predominantly β1 receptors • β2 & β3 exist in ‘small’ quantities β-Adrenergic Receptors Stimulation on β1 receptors • increases • increases • increases • increases heart rate contractility conduction velocity automaticity The effect of adrenergic agents on the heart is mediated through a secondary messenger – cAMP β-Adrenergic Receptors Intracellular cAMP concentrations are regulated by 3 components: • adrenergic receptor on the cell surface • a “G-protein” complex • adenyl cyclase – enzyme synth. cAMP cAMP acts as a secondary messenger • interacts with protein kinase A to increase phosphorylating activity β-Adrenergic Receptors Protein kinases transfer a phosphate group from ATP to serine Thereby, phosphorylating various cellular proteins • phospholamban ( activity) • troponin ( activity) • L-type calcium channels ( activity) β-Adrenergic Receptors Bers DM. Cardiac excitation-contraction coupling. Nature 2002 415;198 - 205 β-Adrenergic Antagonists β-Adrenergic antagonists • effects similar to blockade of L-type calcium channel Clinical effects • decrease contraction (hypotension) • decrease chronotropy (bradycardia) • decrease dromotropy (AV blocks, brady) β-Adrenergic Antagonists Extra-cardiac signs of toxicity • neurological disturbances drowsiness, non-agitated coma • dilated pupils • respiratory depression Treatment of toxicity is based on: • stimulation of glucagon receptor • restoring intracellular Ca2+ stores Overdose Management Overdose Management Decontamination • Emesis not recommended • Activated charcoal should be considered • Gastric lavage with 36-40 Fr tube contraindicated in patients w/ bradycardia consider particularly in patients a/ SR preps • Whole bowel irrigation particularly a/ SR preps Overdose Management Atropine • Adult: 0.5 – 1.0 mg IVP (max 3 mg) • Children: 0.02 mg/kg IVP • given every 2 – 3 minutes Should be held in patients getting WBI because of anticholinergic effects Overdose Management Calcium salts • increases extracellular Ca2+ • calcium gluconate: 1 gm = 4.3 mEq • calcium chloride: 1 gm = 13.4 mEq Dose • 10 – 20 mL of 10% CaCl2 • 30 – 60 mL of 10% Ca gluconate Overdose Management Dose (cont’d) • effect is transient, redose q15 – 20 mins • in adults, can give 50 mL of 10% CaCl2 (5 gm) before having to check a Ca2+ serum concentration • (i.e. 150 mL of 10% Ca gluconate) • CaCl2 is causes sclerosis of peripheral veins and should be given centrally Overdose Management Glucagon • activates adenyl cyclase directly via glucagon receptor • adult dose: 2-5 mg slowly IV • can be repeated every 5-10 minutes • total dose should not exceed 10 mg • follow bolus with an infusion of the dose that produced an effect Overdose Management Catecholeamines • attempt to competitively antagonize βadrenergic antagonist at the receptor • no convincing evidence • chance of stimulating other receptors in the required dose to produce competive displacement • if one is used – norepinephrine is probably the best choice Overdose Management Insulin & Glucose • growing evidence that used correctly, this increases inotropy and chronotropy • theory: improved Ca2+ entry & improved myocardial carbohydrate use • Dose: 0.5 – 1 Unit/kg/hr regular insulin • give 0.5 gm/kg/hr dextrose (glu > 100) • check glucose every 30 mins initially Overdose Management Amrinone • inhibits breakdown of cAMP by phosphodiasterase III • thereby increasing intracellular [] of cAMP • this increases inotropy and chronotropy • BUT, causes vasodilation & hypotension • should be used with a vasopressor Cardiac glycosides (digoxin) Therapeutic Digoxin inhibits Na+/ K+-ATPase This increases cytosolic Ca2+ which increases inotropy. Therapeutically: • digoxin increases automaticity • shortens the repolarization intervals of the atria and ventricles Therapeutic Decreases depolarization & conduction through the SA and AV nodes. These changes are reflected on ECG by: • • • • decrease in ventricular response rate PR interval prolongation QT interval shortening ST segment & T-wave opposite major QRS forces scooped ST segment Both these effects result in the characteristic “digitalis effect” Therapeutic Digitalis effect Atrial flutter with PVC Some characteristic signs of digoxin therapy and toxicity. Clinical Toxicity Toxicologic Effects mirror its therapeutic actions. • Bradydysrhythmias (from increased VAGAL TONE) • Ventricular tachydysrhythmias (from myocardial “irritability”) • Rapid atrial rhythms with slow ventricular response (slowed AV conduction) 2 K+ Phase 2 3 Na+ Ca2+ Ca2+ 3 Na+ Ca2+ Ca2+ Ca2+ SR (Mitochondria) Ca2+ Ca2+ Ca2+ Ca2+ Cell Electrophysiology = DigoxinDigoxin K+ 2 [K+] Phase 2 3 [Na+] Ca2+ Ca2+ 2+ Ca 2+ Ca2+2+ Ca 2+ Ca 2+ Ca 2+ 2+ 2+ Ca Ca CaCa 2+ 2+ Ca2+ Ca2+2+ CaCa 2+ Ca 2+ 2+Ca2+ 2+ 2+ Ca Ca Ca CaCa 2+ 2+ Ca Ca 2+ 2+ Ca Ca 2+ Ca 2+ Ca 2+ 2+ Ca Na+ SR (Mitochondria) Ca Therapeutic & Toxic MoA Signs of Toxicity Metabolic • Acute: Hyperkalemia is a marker for severe poisoning Due to blockade of Na+/K+ ATPase Increases AV blockade and worsens bradydysrhythmias • Chronic: Hypokalemia predisposes the patient to dysrhythmias at lower digoxin levels Higher resting potential increases automaticity Signs of Toxicity Cardiac • Acute or chronic Increased automaticity with high-degree AV block Any dysrhythmia possible….. … EXCEPT a rapidly conducted supraventricular rhythm. Electrocardiogram PVCs (most common dysrhythmia) Classic ECG findings: • Bidirectional ventricular tachycardia • Atrial tachycardia with variable or slow ventricular response • Accelerated junctional rhythms Overdose Management Management of Toxicity The main goal of treatment is to correct cardiac toxicity. Treatment of cardiac toxicity usually leads to resolution of CNS and GI symptoms. Treatment Decontamination • Activated charcoal (AC) Adsorbs digoxin well Decrease absorption ‘Gut dialysis’ [Boldy DA. et al. 1985, de Silva HA. et al. 2003, Ibanez C. et al. 1995] • Multi-dose AC Renal failure Yellow oleander poisoning Treatment Dysrhythmias • Tachy Replace K+ or Mg++ Consider Class IB & III antidysrhythmics • amiodarone, lidocaine or phenytoin for ventricular dysrhythmias AVOID Class IA, IC, II and IV antidysrhythmics • particularly procainamide and quinidine AVOID cardioversion in TOXICITY • Brady Atropine AVOID transvenous/internal pacing Management of Toxicity GI decontamination • Decrease absorption • ‘Gut dialysis’ • [Boldy DA. et al. 1985, de Silva HA. et al. 2003, Ibanez C. et al. 1995] Atropine Correct electrolyte abnormalities Consider lidocaine or phenytoin • for control of dysrhythmias (if definitive therapy unavailable) Indications for digoxin-Fab Symptomatic bradydysrhythmias Ventricular dysrhythmias Acute digoxin toxicity & [K+] >5 mEq/L Ingestion >4 mg - child (or 0.1 mg/kg) Ingestion >10 mg - healthy adult SDC of ≥10 ng/mL steady state • 4-6 hours after ingestion SDC of ≥15 ng/mL at any time Chronic Digoxin Toxicity More common and more controversial No absolute indication based on serum concentration Administer digoxin-Fab if • ECG evidence of digoxin toxicity • Unable to tolerate symptoms of toxicity • Unable to clear digoxin (BUN/Creat) Management Empiric Therapy Acute toxicity: • Adults: 10 – 20 vials • Children: 10 – 20 vials Chronic toxicity: • Adults: 3 – 6 vials • Children: 1 – 2 vials **Should be administered IV over 30 minutes • via a 0.22-micron membrane filter. ** Can be given as an IV bolus in a critically ill patient • (per manufacturer). Management Ingested Dose Known amt ingested (mg) x 0.8 # of vials = 0.5 Serum Drug Concentration (SDC) Known SDC (ng/mL) x pt wgt (kg) # of vials = 100 Things Not To Do!! Calcium • “stone heart” in animal models Transvenous pacing • Taboulet et al. 1993 • failure rate of 23% and a 17% mortality • increased risk of dysrhythmic death Case Review Case #1 45-year old woman PMHx s/f depression presents to the ED after allegedly ingesting all of her anti-HTN medication. Prescription filled 3 days prior for 30 tablets of diltiazem CD 240 mg. Patient alert & oriented, mildly diaphoretic and complaining of generalized weakness. Case #1 Vital signs: • BP: 76/36, HR: 46, RR: 14, Temp: 98.6 • pOx: 100% RA, AccuChk: 154 Rest of physical examination is benign. Patient placed on a cardiac monitor, O2 via nasal cannular and IV access established. Case #1 What is the next step in her management? Case #3 An 86-year old woman presents with increased confusion and vomiting. Per family, she complained of increasing weakness, nausea and decreased appetite over the last 3 days. She has barely kept any of her medications down, and has not been eating. Case #3 PMHx: • hypertension • congestive heart failure (CHF) • diabetes mellitus Medications: • • • • • hydrochlorothiazide digoxin furosemide enteric-coated aspirin metformin Case #3 In the hospital, she is alert, but oriented only to person. Vital signs are normal, except for a heart rate of 46 beats/minute. She weighs 143 lbs (65 kg). Her physical examination demonstrates: • bibasilar rales, irregular S1, S2 with an S3 gallop • bilateral lower extremity 2+ pitting edema up to her shins Case #3 ECG: • atrial flutter with variable block • ventricular rate of 40-50 beats/minute with occasional premature ventricular contractions (PVCs). Laboratory results were within limits except: • potassium - 3.2 mEq/L • creatinine - 1.6 mg/dL • glucose - 235 mg/dL Initial digoxin serum concentration (SDC): • 3.4 ng/mL (> 6 hours since last dose). Case #3 What is the next step in her management? Digoxin-Fab Dose Serum Drug Concentration (SDC) Known SDC (ng/mL) x pt wgt (kg) # of vials = 100 3.4 ng/mL x 65 kg 100 = 2.21 vials ≈ 3 vials Always round UP whatever answer you get. Case #3 The patient is given 3-vials of digoxin specific antibody fragments (digoxin-Fab). About 60 minutes after therapy: • her heart rate improved to 85 beats/minute • blood pressure remained stable • her ECG demonstrated rate-controlled atrial fibrillation with no ectopy • Her serum potassium concentration had also improved Questions?