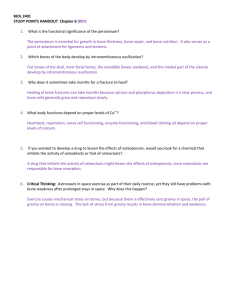
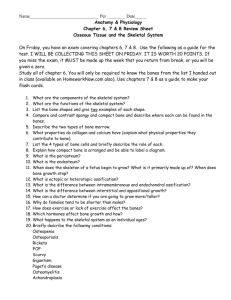
CARTILAGE and BONE
advertisement

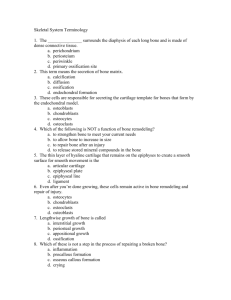
Kharkov National Medical University BONE Department of histology, cytology and embryology BONE: as a Tissue (single) as an Organ (many tissues) Types of Bone Tissue (Classification) According to its architecture: •Spongy (cancellous) and Compact (dense) According to its fine structure: •Primary (woven) and Secondary (lamellar) According to its histogenesis: •Intramembranous and Endochondral 1. • Compact bone is also called dense bone. 2. Compact bone is composed of closely packed osteons. An osteon is also called a Haversian system. • Spongy bone is also referred to as cancellous (trabecular) bone. The mineralized tissue is seen as plates and bars. Trabeculae are the bars seen in the spongy bone. Hollow marrow spaces are also present. • Immature bone is woven bone. It is non-lamellar bone or bundle bone. Functions of Bone: 3. • Supports soft tissues • Protects vital organs (cranium, thoracic cavity) • Contains bone marrow • Reservoir of Ca++, PO4 to maintain constant concentrations in body fluids • Allows body to move General structure 4. • Cells: - Osteoprogenitors (stem cells) – Osteoblasts – Osteocytes – Osteoclasts • Bone matrix: - Organic components- osteoid (50%): type I collagen fibers and ground substance - Inorganic components - Calcified material, lacunae, canaliculi, Calcium hydroxyapatite • Periosteum and Endosteum • Bone marrow Main Cells: 5. 1.Osteoblasts are bone-forming cells • Synthesize organic components of matrix (collagen fibers type I, proteoglycans, glycoproteins.) • Collagen forms osteoids: strands of spiral fibers that form matrix • Influence deposit of Ca++, PO4. • Active vs inactive osteoblasts • Estrogen, PTH stimulate activity Osteoblasts 2.Osteocytes 6. • Mature bone cells that sit in lacunae with filopodia in the canaliculi • Gap junctions between osteocytes provide nutrition (15 cells in a row) • Maintain bony matrix; long living cells • Stimulated by calcitonin; inhibited by PTH Osteocyte with cytoplasmic extensions (filopodia) Osteocytes with filopodia inside of the Canaliculae of Lacunae 3.Osteoclasts are bone-resorptive cells 7. • Derived from monocytes; engulf bony material • Active osteoblasts stimulate osteoclast activity • Large, branched, motile, multinucliated cells lying in Howship’s lacunae • Secrete enzymes that digest matrix Osteoclasts Histology of Compact Bone Osteon (Haversian system) 8. • The whole complex of concentric lamellae of the bone surrounding a canal containing blood vessels, nerves, and loose connective tissue is called a Haversian system, or osteon . • Lacunae containing osteocytes are found between , and occasionally within, the lamellae. In each lamella, collagen fibers are parallel to each other. • Haversian canals communicate with marrow cavity, periosteum, other canals through Volkmann’s canals Haversian system or 9. osteon is a Structural and functional unit of the Compact Bone OSTEONS 10. Periosteum. The outer surface of the bones is covered by a double-layered coat of connective tissue. The outer fibrous layer of periosteum is dense connective tissue. The inner or osteogenic layer is a loose CT containing osteoprogenitor cells. Endosteum lines the marrow cavity. It is condensed reticular tissue that contain bone and blood cell precursors. Bone Formation 11. • Ossification - the process by which bone is formed • Bone formation occurs in four situations: –Formation of bone in an embryo –Growth of bones until adulthood –Remodeling of bone –Repair of fractures Bone Development 12. • Bone may develop directly from mesenchyme or by the replacement of cartilage (indirectly). • The process of replacing other tissues with bone is called ossification OSSIFICATION 13. begins at the 6th week of embryo development and continues up to age of 25 Types: Intramembranous ossification flat bones of skull, mandible and clavicle Endochondral ossification most of the bones in the body formed in the place of hyaline cartilage Intramembranous (direct) Ossification • Intramembranous ossification -bone develops from mesenchyme. – Mesenchymal cells start to secrete the organic components (primary ossification center). Differentiate into osteoblasts. Further differentiation into osteocytes. – Spicule formation – Formation of spongy and compact bone. Intramembranous Ossification • Condensation of mesenchyme into trabeculae • Osteoblasts on trabeculae lay down osteoid tissue (uncalcified bone) • Calcium phosphate is deposited in the matrix forming bony trabeculae of spongy bone • Osteoclasts create marrow cavity • Osteoblasts form compact bone at the surface • Surface mesenchyme produces periosteum Remodeling is secondary bone formation Osteoclasts erode the primary bone matrix, blood vessels, nerves and lymphatics invade the cavity and osteogenic cells develop in osteoblasts and osteocytes, which create concentric lamellae and osteons. Remodeling helps reshape growing bones to adapt to changing loads. INTRAMEMBRANOUS OSSIFICATION 14. 1.Mesenchyme cells differentiate into osteoblasts. Osteogenic islands. 2.Osteoblasts secrete osteoid matrix. Osteoblasts surround themselves with bone matrix, forming osteocytes. It is osteoid stage. 3.Osteoid becomes mineralized through crystallization of Ca++ salts using enzyme alkaline phosphatase and is called primary ossification center(OC). It is ossification stage and formation of spicules. 4.Blood vessels begin to grow spicules that meet and fuse together. Woven Bone (primary spongy bone). 5. Osteoclasts erode the primary bone matrix. It is remodeling or Secondary bone formation. Endochondral (indirect) Ossification 1 • Bone develops from pre-existing model – perichondrium and hyaline cartilage • Formation of primary ossification center (OC) and marrow cavity in shaft of model – – – – bony collar developed by osteoblasts chondrocytes swell and die stem cells give rise to osteoblasts and clasts bone laid down and marrow cavity created Endochondral Ossification 2 • Secondary ossification centers and marrow cavities are formed in the ends of the bone – same process • Cartilage remains as articular cartilage and epiphyseal (growth) plates – growth plates provide for increase in length of bone during childhood and adolescence – by early twenties, growth plates are gone and primary and secondary marrow cavities united Endochondral bone formation 15. 1.Cartilage model 2.The periosteal bone collar (perichondral ossification) 3.Proliferation,hypertrophy,calcification of the cartilage. Formation of primary marrow cavity and Periosteal bud- small cluster of blood vessels 4. Primary ossification center 5.Secondary ossification center 7.Secondary bone formation and remodeling 8.Bone growth in length and girth Structure of the epiphyseal plate: 16. 1. Zone of reserve cells (resting cartilage): A thin layer (3-6 cells wide) of small, randomly oriented chondrocytes adjacent to the bony trabeculae on the articular side of the growth plate. 2. Zone of proliferation: Chrondrocytes are stacked in prominent rows, mitotic figures and the cartilage matrix becomes more basophilic 3. Zone of maturation: No mitoses; gradual cellular enlargement. 4. Zone of hypertrophy: Chrondrocytes and their lacunae increase in size. 5. Zone of calcification: Deposition of minerals in the matrix surrounding the enlarged lacunae causing cell death. 6. Zone of ossification: Osteoblasts deposit bone matrix on the exposed plates of calcified cartilage. 7. Zone of resorption: Osteoclasts absorb the oldest bone spicules. Bone Growth and Remodeling • Bones increase in length – interstitial growth of epiphyseal plate – epiphyseal line is left behind when cartilage gone • Bones increase in width = appositional growth – osteoblasts lay down matrix in layers on outer surface and osteoclasts dissolve bone on inner surface • Bones remodeled throughout life – Wolff’s law of bone = architecture of bone determined by mechanical stresses • action of osteoblasts and osteoclasts – greater density and mass of bone in athletes or manual worker is an adaptation to stress BONE GROWTH in LENGTH • on epiphyseal side chondrocytes continually reproduce by epiphyseal plate • on diaphyseal side chondrocytes swell and become surrounded by calcified matrix, chondrocytes die, bone replaces chondrocytes bone is eroded away by osteoclasts, marrow cavity forms • epiphyseal plate remains constant until 18 years in females,20 years in males • epiphyseal plate becomes ossified after 25 years • It is stop growth of the bone. BONE GROWTH in girth (DIAMETER) Compact bone grows in thickness by proliferation and differentiation of osteoprogenitor cells in the inner layer of the periosteum and due to deposition of new ossified tissue on the outer surface of the bone. Marrow cavity increases in diameter Balance between osteoblasts and osteoclasts depends from Hormonal regulation.