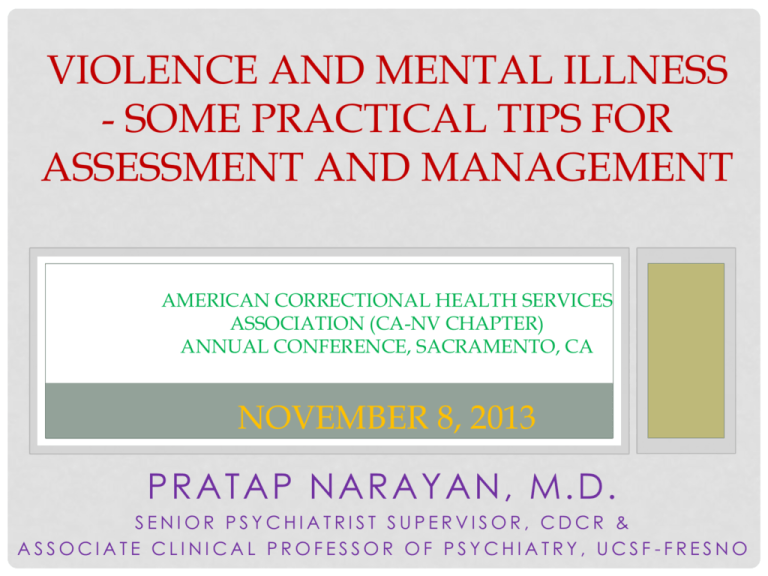
VIOLENCE AND MENTAL ILLNESS
- SOME PRACTICAL TIPS FOR
ASSESSMENT AND MANAGEMENT
AMERICAN CORRECTIONAL HEALTH SERVICES
ASSOCIATION (CA-NV CHAPTER)
ANNUAL CONFERENCE, SACRAMENTO, CA
NOVEMBER 8, 2013
PRATAP NARAYAN, M.D.
SENIOR PSYCHIATRIST SUPERVISOR, CDCR &
ASSOCIATE CLINICAL PROFESSOR OF PSYCHIATRY, UCSF -FRESNO
The contents of this presentation are the
opinions solely of the author and do not
represent the endorsements or opinions of
the CCHCS, CDCR, CA State Govt. or any
other organization(s).
Any republication, retransmission, and/or
reproduction of all or any part of the
materials contained herein is expressly
prohibited, unless the copyright owner of
the material has expressly granted prior
written consent to so republish, retransmit,
or reproduce the material.
All other rights are reserved.
2
VIOLENCE AND MENTAL HEALTH
• Association between dangerousness and mental
illness – facts and myths
• Risk assessment – Historical data, Clinical
assessment, Collateral Info, Differential diagnoses
• Management/Treatment: Medications; Other
interventions - Acute, Sub-acute and Chronic
settings
• Legal implications and Risk Management issues
SEUNG-HUI CHO - 2007
Shooting spree in Blacksburg, VA – 4/16/07
Killed 32 people, injured 17 others
Committed suicide before he could be arrested
“Soc. anxiety d/o” - middle school – recd therapy
Placed in sp ed (ED) – recd speech therapy
Dx w/ MDD in 2005 (age 21) – Rx Prozac (?noncompliant)
• Teased and bullied in school for “shyness”
•
•
•
•
•
•
PUBLIC PERCEPTION
• Link et al, 1999 - 75% believed that mentally ill are
dangerous; 60% believed people w/ schizophrenia
were likely to commit violent acts
• Judges, lawyers, the media and physicians share
this viewpoint
• So do many mental health professionals
• But, this is not supported by the
research!
SOME RELEVANT RESEARCH - 1
• Elbogen and Johnson (2009):
• Large scale survey (n=34,653)
• Incidence of violence was higher with SMI, but ONLY w/ cooccurring substance use
• Mental illness alone did NOT predict future violence
• Similar results - MacArthur Violence Risk Assessment Study
(2000)
• SMI w/o substance abuse and h/o violence – same risk of
violence in next 3 yrs as gen pop.
• Any type of SMI – NOT at increased risk of serious/violent
acts
SOME RELEVANT RESEARCH - 2
• Steadman (1998):
• Substance use: 73% more likely to be aggressive (w/ or w/o
MI)
• Holcomb and Ahr (1988):
• ETOH/drugs – more lifetime arrests than SMI
• Teplin (1994): (n=627 random male arrestees)
• 3x higher prevalence of MI (but most commonly PDO and
substance use d/o)
• Did not support stereotyped notion of mentally ill criminals
invariable re-offending after release
FAZEL, ET AL - 2009
• Large group of subjects (n=8003 schizophrenia,
n=80025 GP)
• Schizophrenia w/o substance abuse – slightly higher
rate (1.2:1) of violent crime compared to GP
• Schizophrenia w/ substance abuse – More than 4x
likely (4.4:1) as GP to have a violent-crime
conviction
• In latter group, when compared to unaffected
siblings, risk of violence was less pronounced
FAZEL, ET AL - 2010
• Bipolar D/os and Violent Crime: Pts no more likely to
commit violent crime than GP unless used
ETOH/drugs
• Higher risk of violent crime in unaffected siblings of
people w/ Bipolar D/O
• Highlights contribution of genetic or early
environmental factors rather than MI
JARED LEE LOUGHNER - 2011
• Perpetrated shooting in Tucson, AZ – 1/8/11
• Killed 6 people, injured 13 others (including US
Rep Giffords)
• Dx as “Paranoid Schizophrenia” by 2 MH
professionals
• Initially found IST – forcibly medicated, and later
found CST
• Abused alcohol and drugs in the years before
• Pleaded guilty – sentenced to life w/o parole
(seven consecutive life-terms + 140 years w/o
parole
FUTURE VIOLENCE – RISK FACTORS
• Historical:
• Past violence, juvenile detention, physical abuse, parental
arrest
• Dispositional:
• Age, Sex, income
• Clinical:
• Substance Abuse, perceived threats
• Contextual:
• Recent events: divorce, unemployment, victimization
RISK ASSESSMENT - HISTORICAL
•
•
•
•
•
•
Past violence – risk increases with # of past episodes
Juvenile detention hx
Physical Abuse
Parental arrest record
H/o military service
H/o weapons training
RISK ASSESSMENT - DISPOSITIONAL
•
•
•
•
•
Age – younger age
Sex – male
Income – lower SES
Marital status – Single
Employment status - unemployed
RISK ASSESSMENT - CLINICAL
•
•
•
•
•
•
•
•
•
Substance use
Lower IQ, h/o head trauma
Perceived threats
Low self-esteem, hopelessness, depression
Acute psychosis, Threat/control Override sx.
Poor compliance w/ tx
Personality disorder, impulsivity, anger dyscontrol
Suicidality – homicidality
Low GAF score
RISK ASSESSMENT - CONTEXTUAL
•
•
•
•
•
•
•
•
Recent divorce
Unemployment
Recent victimization
Environmental violence
Position of vulnerability/ powerlessness
Recent move of weapon out of storage
Access to weapon
Access to potential victim(s)
OTHER FACTORS INCREASING RISK
•
•
•
•
•
•
•
•
Risk indicators denied/minimized
Info not shared between professionals
Clinical responsibility not clearly defined/transferred
Poor community support
Caregivers unaware of availability of svcs
Inadequate provision of resources
Poor admin focus on education/training
Systematic risk assessment not done
CLINICAL CONSIDERATIONS
• Clinical settings: Managing aggression/violence top
priority
• Proper assessment and attention to red flags is
crucial
• All aggression is not psychiatric or mental-health
related
• A medical or surgical cause may need to be ruled
out
CLINICAL ASSESSMENT
• Frontline assessment:
•
•
•
•
•
•
•
Environment – threatening, uncomfortable, hostile
Sensorium – clouding, misperception
Emotions – anger, depression, fear, powerlessness
Personality aspects – impulse control, manipulation
ETOH/drug use – intoxication, withdrawal, seeking
Medications causing agitation or disinhibition
Psychiatric conditions – acute psychosis, agitation
CLINICAL ASSESSMENT - 2
Body language – restlessness, rapid breathing
Verbal communication – hostile content, tone
Eye contact – intense, prolonged
Muscle tension – Clenching fists, jaws,
Suspiciousness – hypervigilance, statements
Frustration – long wait-time, denial of wants
Abrupt changes - posture, mood, tone of voice,
psychomotor activity
• Most important – Trust Your Gut instincts
•
•
•
•
•
•
•
DIFFERENTIAL DIAGNOSES
•
•
•
•
•
•
•
Substance Use Disorders
Personality Disorders
Psychotic and Mood Disorders
Delirium
Dementia
Other medical or neurological conditions
Mental Retardation
JAMES EAGAN HOLMES - 2012
Alleged perpetrator of CO mass shooting (7/20/12)
Killed 12 and injured 58 others
Several suicide attempts in jail in Nov 2012
Reportedly h/o past contact w/ MH professionals
Unusual behavior – orange hair, claimed he was
“Joker”, etc.
• No previous criminal history known
• After NG plea in March, pled NGRI in June 2013 –
awaiting trial
•
•
•
•
•
ACUTE MANAGEMENT STRATEGIES
• Non-threatening approach – calm manner
• De-escalation – empathize, meet pt halfway, quiet
environment, isolation from disruptive influences
• Minimize risk to staff/family – get LE involved
• Physical Restraints/Seclusion – if lesser restrictive
measures fail
• Medications:
•
•
•
•
Anxiolytics, antipsychotics
Oral route preferable – more autonomy and dignity
Parenteral – if necessary
Pain management, if indicated
COLLATERAL INFORMATION
• Interview others – obtain relevant info (e.g. family,
friends, neighbors, custodians, attorneys, parole
agents, probation officers)
• Tap diverse sources, if possible
• Review past medical records – IP and OP
• Obtain legal records, if indicated – previous parole
or probation reports, diversion reports from court,
correctional classification files, etc.
SHORT-TERM
• Assess antecedents – address env. stress
• Remove access to weapons
• Ensure safety of potential victims – referral to
shelters, notification of law enforcement, etc.
• Optimize medication management of treatable
conditions
• Engage pt in abstinence from drugs/ETOH
• Long-term substance abuse treatment placement
LONG-TERM
Long-term abstinence – random drug testing
Involvement in NA, AA
1:1 and/or group therapy
Monitor long-term tx compliance
Psychosocial aspects – employment, housing,
financial assistance, medical care
• Do not hesitate to involve the law – pursue
prosecution if violence persists
• Sometimes, incarceration may be necessary
• Avoid “medicalizing” violence
•
•
•
•
•
PREVENTIVE
•
•
•
•
•
•
•
Be vigilant
Use alarms/safety equipment
Undergo personal safety training
Regular education and training – possible drills
Become familiar with pt’s hx as early as possible
In high-risk cases, strength in numbers
Show-of-strength sometimes helps
ADAM PETER LANZA - 2012
Responsible for Sandy Hook shooting (12/14/12)
Killed 27 and injured 2 others
Committed suicide when police entered bldg
Past dx: Autism, “personality disorder”, “Asperger’s
syndrome” and “sensory-integration disorder”
• Had no previous criminal history
• Pt advocates defined autism as a “brain” disorder
and not mental illness
•
•
•
•
RISK ASSESSMENT TOOLS
• Many actuarial tools, involving static and dynamic
factors
• Actuarial measures better than unstructured clinical
judgment; which is better than chance!
• Accuracy can be improved when context can be
factored into the equation
• However, some doubt re: the value of actuarial
tools for positive predictive value.
SOME TOOLS
•
•
•
•
•
•
•
•
Dangerous Behavior Rating Scale (DBRS)
Violence Risk Appraisal Guide (VRAG)
Psychopathy Checklist – Revised (PCL-R)
Historical/Clinical/Risk Management 20-item scale
(HCR-20)
Sex Offender Risk Appraisal Guide (SORAG)
Static-99
Sexual Violence Risk-20 (SVR-20)
Spousal Assault Risk Assessment (SARA)
LINK BETWEEN VIOLENCE AND MENTAL
DISORDER
• Even in mentally ill w/ h/o violence –
violence is not always result of mental illness.
E.g.: A psychotic patient may continue to be
violent even after psychosis is controlled
• Mental illness and violent tendency can
coexist.
• Although mental illness may be treated,
future violence may not necessarily be
prevented (Huber et al. 1982).
• Some mentally ill people do commit
violence; but, it is unfair to generalize that all
mentally disordered people are potentially
more violent than the G.P.
ACUTE SX VS DIAGNOSIS
• Research – some acute sx may be
more specifically linked to violence
than dx.
• Many major mental disorders show
episodic exacerbation and remission
(McNiel and Binder 1994).
• Thus, just dx of mental disorder not
enough to determine culpability (or
lack)
• Violence being grossly underreported by MH professionals
MYTHS INVOLVING UNDERREPORTING
• Assaults are “inevitable” in MH practice
• Reporting ends the therapeutic alliance
• It is ethically wrong to be in dual role of tx.provider and accuser
• ‘Pt. not responsible for violence because of
mental status; reporting is not appropriate’
• Victim: “It’s my fault – I should’ve been more
vigilant”
• Reporting will breach confidentiality
• “No use reporting” – chance of legal action
very small
DEFENSIVE MANEUVERS
• Denial and rationalization: Potent factors in
handling and disposition of assaultive pts
(Dubin et al, 1988)
• 3800 OP psychiatrists in PA, NJ and DE: 59%
contd to tx pt after being assaulted.
• 55% felt they could have anticipated assault
(Madden et al, 1976)
• “Most insidious form of denial”: Failure to
obtain unflattering and anxiety-producing
data from pt’s hx (Lion and Pasternak)
• Incident result of therapist’s negative countertransference
OTHER FACTORS
• Therapist’s behavior might be seductive;
project unconscious expectation that assault
will take place; or attempt to cover underlying
hostility with kindness; (Madden, et al. 1976).
• High-cost of forensic evals vs. low level of
punishment
• Judicial system believes that psych pts belong
in hospital, not in jail; individuals who choose
MH work must accept associated risks
UNDER-REPORTING: OTHER
FACTORS
• Institution - No reporting requirements or
discourages reporting (? admin burden)
• Staff – ‘Employer not supportive’; fear of
being criticized by supervisors
• Institution fears negative publicity; deals w/
incidents w/o involving judicial system
(Seclusion, meds, etc.)
• Colleagues may be unsupportive and
dissuade reporting
• Institutional belief: violence due to lack of
proper tx
RECENT VIEWPOINTS
• If pts’ crimes are ignored, then those pts may learn
that their conduct is acceptable, tolerated, and
immune from adverse consequences (Leeuwen
and Harte, 2011; Miller and Maier, 1987; Quanbeck,
2006; Coyne, 2002)
• Pt population characteristics in mental hospitals
changing:
•
•
•
•
More people with personality disorders and h/o violence
Dangerousness is required criterion for civil commitment
Deinstitutionalization: Less severely ill pts out of hospitals
Therapist’s potential liability when pt injures 3rd party;
hospitalization of assaultive pts for preventive detention
(Appelbaum, 1988).
SOME OBSERVATIONS
• Sometimes, hospitalization is for confinement,
not treatability
• In acute setting, causal relationship of MI to
violence difficult to establish; so, hospital
admission more likely than arrest
• Both legal professionals and clinicians lack
(and therefore need) specific training to
recognize differences between behavior due
to pt’s illness (and lack of control), and
impulsive or deliberate behavior (due to
character pathology) that can be addressed
by criminal sanctions (Miller and Maier, 1987).
SHOULD WE PROSECUTE VIOLENT
OFFENDERS?
• “Prosecution is not in line with the principle of
patient beneficence”.
• However, successful prosecution has been reported
to have a beneficial effect, with a significant
reduction in frequency and severity of aggressive
behavior in some patients (Kumar, 2006).
DISADVANTAGES OF LEGAL ACTION
• If prosecution pursued inconsistently, pts may
feel victimized.
• Prosecution and punishment have no direct
therapeutic value; can cause guilt among MH
professionals
• Prosecution may be ploy to expel unpopular
pts
• Imprisonment may be anti-therapeutic
• Possibility of scapegoating by other pts and
staff
CASE EXAMPLE: POSITIVE
OUTCOME OF PROSECUTION
• 40 yo MR female – h/o striking out when frustrated, esp. when
limits set by staff:
• During an admission, pt impulsively slapped or hit several
nurses and mental health workers.
• Staff concluded that clinical methods employed restrictions, medications, and consistent limits - were
ineffective and that pt was capable of self-control. Pt was
informed.
• Pt hit nurse again and charges were filed.
• She was found competent and criminally responsible for her
actions and was sentenced to 2 weeks in prison.
• Afterwards, transferred to another facility; no assaults
• Staff felt they had made successful intervention
(Hoge and Gutheil, 1987)
DISADVANTAGES OF LEGAL ACTION
• Adverse publicity for institution
• Can be time-consuming and impractical
• Pts have option of counter-suit or other forms of
retaliation (e.g. reporting to Medical Board)
• Will involve breach of pt confidentiality
PROSECUTION: POSITIVE EFFECTS
• Positive effect on staff morale – more willingness to
work with potentially assaultive patients (Miller and
Maier, 1987)
• Lets staff know that they also have rights
• May help increase patient’s capacity to accept
responsibility for their crime (Eastman and Mullins,
1999)
• Can have positive impact on health and
performance at work
• Prosecution may uncover malingering
• Reduces stigma: the mentally ill are not “globally and
totally impaired” – they can be held responsible for
criminal behavior
• May deter future aggression (Miller and Maier, 1987)
PROPONENTS OF PROSECUTION
• Miller and Maier (1987) suggest use of
prosecution within framework of tx (or tx failure)
in repeatedly aggressive pts
• Pts with PDOs, who are unmotivated for tx,
should not be protected from legal
consequences of their behavior
• Legal professionals should be trained to
recognize that pts w/ mental d/os can be
responsible for their actions; and MH
professionals deserve as much protection as
other citizens (Miller and Maier, 1987).
A DIFFERENT VIEWPOINT
• Appelbaum and Appelbaum (1991) wrote policy at MA
state hospital that allowed “filing of criminal charges
under only extreme circumstances involving serious
criminal acts”.
• They excluded any therapeutic intent; “only retribution
or protection of others is acceptable ground for
prosecution in such a setting” (i.e. holding patients to
the same expectations society holds for all citizens).
• Prosecution therefore may be appropriate:
• therapeutically (to help set limits for patients, particularly those
with character disorders)
• legally (to bring to the public’s attention an individual who is
assaultive - a social, not a clinical, matter)
• morally (otherwise an injurious act may proceed without just
consequence) (Mills and et al. 1985)
SUMMARY
• Violence and dangerousness have become more
commonplace in society – we will all encounter this at
some point
• The association between mental disorders and violence
is tenuous; other factors appear to be much more
significant than mental illness in increasing risk of
violence
• Legal and healthcare professionals and the media need
to be educated about the association (or lack)
between mental illness and violence
• We can improve the accuracy of assessments with
education and diligence
• Sometimes, there is no recourse other than prosecution
THE END
• QUESTIONS ?????
• COMMENTS