File
advertisement

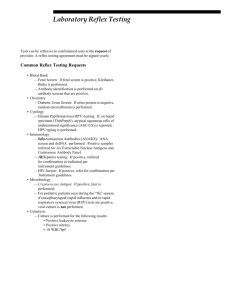
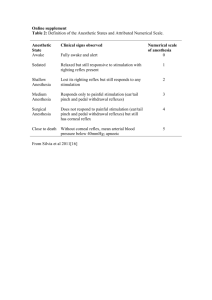
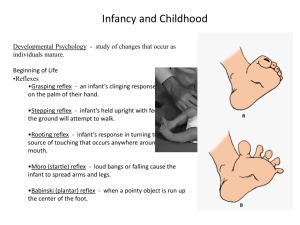
PTA 120 - Pathology Neurology Primitive Reflexes Primitive reflexes are reflex actions originating in the central nervous system that are exhibited by normal infants but not neurologically intact adults, in response to particular stimuli. These reflexes disappear or are inhibited by the frontal lobes as a child moves through normal child development. These primitive reflexes are also called infantile, infant or newborn reflexes. Older children and adults with atypical neurology (for instance, people with cerebral palsy) may retain these reflexes and primitive reflexes may re-appear in adults because of certain neurological conditions including, but not limited to, dementia, traumatic lesions, and strokes. An individual with cerebral palsy and typical intelligence can learn to suppress these reflexes, but the reflex might resurface under certain conditions such as during an extreme startle reaction. Reflexes may also be limited to those areas affected by the atypical neurology, such as individuals whose cerebral palsy affects only their legs retaining the Babinski reflex but having normal speech; in individuals with hemiplegia, the reflex might be seen in the foot on the affected side only. Primitive reflexes are primarily tested with suspected brain injury to test the functioning of the frontal lobe. If they are not being suppressed properly they are called frontal release signs. Atypical primitive reflexes are also being researched as potential early warning signs of autistic spectrum disorders. Adaptive value of reflexes Reflexes vary in utility. Some have a survival value. An example is the rooting reflex, which helps a breastfed infant find the mother's nipple. Babies display it only when hungry and touched by another person, not when they touch themselves. There are a few reflexes that probably helped babies survive during human evolutionary past like the Moro reflex. Other reflexes such as sucking and grabbing help establish gratifying interaction between parents and infants. They can encourage a parent to respond lovingly and feed more competently. They can also help parents comfort their infant because they allow the baby to control distress and the amount of stimulation they receive. PTA 120 - Pathology Neurology Moro reflex – Postural Reaction The Moro reflex in a four-day-old infant: 1) the reflex is initiated by pulling the infant up from the floor and then releasing him; 2) he spreads his arms 3) he pulls his arms in ; 4) he cries (10 seconds) This is sometimes referred to as the startle reaction. It is an automatic response to a sudden change in sensory stimuli. A sudden change of any kind (bright light, change in body position, temperature, loud noise, intense touch etc.) can trigger the Moro Reflex. The Moro reflex is present at birth, peaks in the first month of life, and begins to disappear around 2 months of age. It is likely to occur if the infant's head suddenly shifts position, the temperature changes abruptly, or he is startled by a sudden noise. The legs and head extend while the arms jerk up and out with the palms up and thumbs flexed. Shortly afterward the arms are brought together and the hands clench into fists, and the infant cries loudly. The reflex normally disappears by three to four months of age, though it may last up to six months. Bilateral absence of the reflex may mean damage to the infant's central nervous system while a unilateral absence could mean an injury due to birth trauma such as a fractured clavicle or injury to the brachial plexus. Erb's palsy or some other form of paralysis is also sometimes present in such cases. In human evolutionary history, the Moro reflex may have helped the infant cling to his mother while she carried him around all day. If the infant lost its balance, the reflex caused the infant to embrace its mother and regain its hold on the mother’s body. Some possible long term effects of an unintegrated Moro are: Easily triggered, reacts in anger or emotional outburst Poor balance and coordination Poor stamina Poor digestion, tendency towards hypoglycemia Weak immune system, asthma, allergies and infections Hypersensitivity to light, movement, sound, touch & smell Vision/reading/writing difficulties Difficulty adapting to change Cycles of hyperactivity and extreme fatigue PTA 120 - Pathology Neurology Walking/stepping reflex The walking or stepping reflex is present at birth; though infants this young can not support their own weight, when the soles of their feet touch a flat surface they will attempt to 'walk' by placing one foot in front of the other. This reflex disappears at 6 weeks due to an increased ratio of leg weight to strength. It reappears as a voluntary behavior at around eight months to a year old. Asymmetric Tonic neck reflex (ATNR) The tonic neck reflex, also known as asymmetric tonic neck reflex or 'fencing posture' is present at one month of age and disappears at around four months. When the child's head is turned to the side, the arm on that side will straighten and the opposite arm will bend (sometimes the motion will be very subtle or slight). If the infant is unable to move out of this position or the reflex continues to be triggered past six months of age, the child may have a disorder of the upper motor neurons. According to researchers, the tonic neck reflex is a precursor to the hand/eye coordination of the infant. It also prepares the infant for voluntary reaching. The ATNR is important for developing unilateral (one-sided) movements. When the infant turns his head to one side, the arm and leg of that side automatically extend. In utero the ATNR provides the necessary stimulation for developing muscle tone and the vestibular system. It assists with the birth process, providing one of the means for the baby to “corkscrew” down the birth passage. ATNR also provides training in the hand-eye coordination. By six months of age, this reflex should evolve into more complex movement patterns. If the TNR remains active it plays a significant contribution to academic problems at school. Some possible long term effects of an unintegrated ATNR are: Dyslexia Reading, listening, handwriting and spelling difficulties Difficulty with math Confused handedness PTA 120 - Pathology Neurology Tonic Labyrinthine Reflex (TNR) The tonic labyrinthine reflex (TLR) is a primitive reflex found in newborn humans. With this reflex, tilting the head back while lying on the back causes the back to stiffen and even arch backwards, the legs to straighten, stiffen, and push together, the toes to point, the arms to bend at the elbows and wrists, and the hands to become fisted or the fingers to curl. The presence of this reflex beyond the newborn stage is also referred to as abnormal extension pattern or extensor tone. The presence of the TLR as well as other primitive reflexes such as the asymmetrical tonic neck reflex (ATNR) beyond the first months of life may indicate that the child has developmental delays and/or neurological abnormalities. For example, in people with cerebral palsy, the reflexes may persist and even be more pronounced. As abnormal reflexes, both the tonic labyrinthine reflex and the asymmetrical tonic neck reflex can cause problems for the growing child. The TLR and ATNR both hinder functional activities such as rolling, bringing the hands together, or even bringing the hands to the mouth. Over time, both the TLR and ATNR can cause serious damage to the growing child's joints and bones, causing the head of the thighbone to partially slip out of the hip socket (subluxation) or completely move out of the hip socket (dislocation). TLR provides the baby with a means of learning about gravity and mastering neck and head control outside the womb. This reflex is important for giving the baby the opportunity to practice balance; increase muscle tone; and develop the proprioceptive and balance senses. The TLR interacts with other reflexes to help the infant to start developing coordination, posture and correct head alignment. It is vital for the TLR to do its job because correct alignment of the head with the rest of the body is necessary for balance, eye tracking, auditory processing, muscle tone and organized movements - all of which are essential to the development of our ability to focus and pay attention. The Tonic Labyrinthine Reflex has two forms, forward and backward: Forward: As the head bends forward, the whole body: arms, legs, and torso curl inward in characteristic fetal position. Backward: As the head is bent backward, the whole body, arms, legs and torso straighten and extend. PTA 120 - Pathology Neurology TLR provides the baby with a means of learning about gravity and mastering neck and head control outside the womb. This reflex gives the baby opportunities to practice balance, increase muscle tone and develop the proprioceptive and vestibular senses. Eventually the TLR interacts with other reflexes and bodily processes to help the child develop coordination, posture and correct head alignment from infancy through toddlerhood. It is critical for the TLR to do its “job” because correct alignment of the head with the rest of the body is necessary for balance, visual tracking, auditory processing and organized muscle tone, all of which are vital to the ability to focus and pay attention. Some Possible Long Term Effects of an unitegrated TLR are: Balance and coordination problems Shrunken posture Fatigues easily May have a fear of heights Muscle tone usually weak or too tight Motion sickness Difficulty judging distance, depth, space and speed Toe walking “W” leg position when floor sitting Tendency to be cross-eyed Visual, speech, auditory difficulties Stiff jerky movement Difficulty following directional or movement instructions Difficulty walking up/down stairs Palmar grasp reflex The palmar grasp reflex appears at birth and persists until five or six months of age. When an object is placed in the infant's hand and strokes their palm, the fingers will involuntarily close and they will grasp it. The grip is strong but unpredictable; though it may be able to support the child's weight, they may also release their grip suddenly and without warning. The reverse motion can be induced by stroking the back or side of the hand. Clenching of the fingers or toes on stimulation of the palm or sole is normal only in infancy and associated with frontal lobe brain lesions. Plantar reflex – Babinski Sign A plantar reflex is a normal reflex that involves plantar flexion of the foot (toes move away from the shin, and curl down. An abnormal plantar reflex (aka Babinski Sign) occurs when upper motor neuron control over the flexion reflex circuit is interrupted which results in a dorsiflexion of the foot (foot angles towards the shin, big toe curls up). This also occurs in babies under ~1 year, because of low myelination of the corticospinal tracts. As these tracts develop to adult form, the flexion-reflex circuit is inhibited by the descending corticospinal inputs, and the normal plantar reflex develops. Also known as the Babinski reflex, this is a sign of neurological abnormality, e.g. upper motor neurone lesion, in adults. PTA 120 - Pathology Neurology Neck Righting Reflex The trunk is rotated in the direction in which the head of the supine infant is turned; this reflex is absent or decreased in infants with spasticity. Neck reflexes make adjustments in trunk posture and limb position caused by stimulation of proprioceptors in the neck joints and muscles when the head is turned, tending to maintain a constant orientation between the head and body. Galant reflex The Galant reflex is present at birth and fades between the ages of four to six months. When the skin along the side of an infant's back is stroked, the infant will swing towards the side that was stroked. If the reflex persists past six months of age, it is a sign of pathology. The Galant reflex works in conjunction with the ATNR to help the baby's journey down the birth canal. It is also thought to help babies balance and coordinate the body for belly crawling and creeping. It is thought to be connected to bladder function because a high percentage of children who are bedwetting past age 5 have an active Galant reflex. Some possible long term effects of an unintegrated Spinal Galant Reflex are: Bedwetting Poor endurance Attention difficulties Hip rotation to one side/scoliosis Poor concentration Poor coordination Poor posture Poor short-term memory Fidgeting/hyperactivity PTA 120 - Pathology Neurology Landau Reflex The Landau reflex is a postural reflex that the infant needs to develop to sit and walk independently. It allows the child to strengthen muscle tone and refine motor skills. To test for the reflex, the doctor will hold the infant face down horizontally. The baby's head will raise up, while her trunk will be straight and her legs extended. When the doctor pushes the baby's head downward, her legs should drop as well. When the doctor releases the baby's head, both her head and legs should return to their original positions. The reflex can appear any time between 3 months to 10 months and disappears as the child matures, usually by the time he is 3 years old. Assessing the Landau reflex is part of the routine physical examination for babies who are 6 months old. If an infant lacks the Landau reflex, he may need to be evaluated for a motor development issue. Children with cerebral palsy can lack the Landau reflex. Parachute reaction Protective abduction of arms, extension of elbows and wrists and spreading of fingers, a normal defence reflex, elicited when an infant is held in ventral suspension and is tilted abruptly forward toward the floor, seen in the 7th–12th month of age, a response that is asymmetrical in infants with hemiparesis and is an early sign of cerebral palsy. PTA 120 - Pathology Neurology Extensor Thrust a spinal-level reflex present in a human in the first 2 months of life. It is an exaggeration of the positive support reflex and consists of an uncontrolled extension of a flexed leg when the sole of the foot is stimulated. Examples of reflexes that last into adulthood are: Blinking reflex -- blinking the eyes when touched or when a sudden bright light appears. Cough reflex -- coughing when the airway is stimulated. Gag reflex -- gagging when the throat or back of the mouth is stimulated. Sneeze reflex -- sneezing when the nasal passages are irritated. Yawn reflex - yawning when the body needs more oxygen. Knee jerk/Patellar reflex Flexor Withdrawal reflex - a nociceptive reflex in which a body part is quickly moved away from a painful stimulus. It is a widespread contraction of physiologic flexor muscles and relaxation of physiologic extensor muscles and characterized by abrupt withdrawal of a body part in response to painful or injurious stimuli. Righting reflex - the ability to assume an optimal position when there has been a departure from it. PTA 120 - Pathology Neurology Crossed Extension Reflex - occurs with a withdrawal reflex.When the reflex occurs the flexors in the withdrawing limb contract and the extensors relax, while in the other limb, the opposite occurs. An example of this is when a person steps on a nail, the leg that is stepping on the nail pulls away, while the other leg takes the weight of the whole body. The crossed extensor reflex is contralateral, meaning the reflex occurs on the opposite side of the body from the stimulus. To produce this reflex, branches of the afferent nerve fibers cross from the stimulated side of the body to the contralateral side of the spinal cord. There, they synapse with interneurons , which, in turn, excite or inhibit alpha motor neurons to the muscles of the contralateral limb. In the ipsilateral leg (the one which steps on the nail), the flexors contract and the extensors relax to lift the leg from the ground. On the contralateral side, the flexors relax and the extensors contract to stiffen the leg since it must suddenly support the entire weight of the body. At the same time, signals travel up the spinal cord and cause contraction of the contralateral muscles of the hip and abdomen to shift the body’s center of gravity over the extended leg. To a large extent, the coordination of all these muscles and maintenance of equilibrium is mediated by the cerebellum and cerebral cortex.