ethylene glycol
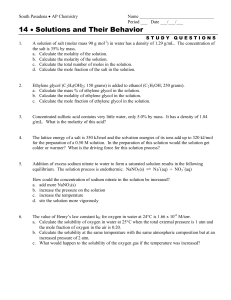
advertisement

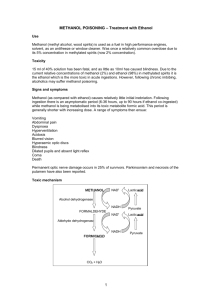
ALCOHOL OVERDOSE Kobra Naseri PharmD, PhD of Pharmacology ETHANOL POISONING Ethanol (ethyl alcohol,C2H5OH) - is derived from fermentation of sugars in fruits, cereals, and vegetables. Ethanol: the most frequently abused intoxicant INTRODUCTION PHARMACOLOGY OF ETHANOL CNS depressant: inhibits neuronal activity behavioral stimulation at low blood level Cross tolerance: BZD & barbiturates Absorption: proximal small bowel Excretion: 2% ~ 10% by lungs, in urine, in sweat PHARMACOKINETICS Ethanol is readily absorbed (peak30-120 min) (Vd=0.5-0.7L/kg). It is rapidly absorbed by diffusion across the lipid membranes of the stomach and small intestine. Coingestion of food or decreased GI motility produces a delay in absorption and increases the gastric metabolism of ethanol. Metabolism of ethanol 90% metabolized in the liver by one of the two pathways: 1. cytosol: – alcohol dehydrogenase – aldehyde dehydrogenase 2. microsomal alcohol oxidizing system Ethanol Alcohol dehydrogenase Acetaldehyde Aldehyde dehydrogenase Acetaldehyde Syndrome Acetic The mediator of liver toxicity acid Acetyl CoA CO2 + H 2O METABOLIC PATHWAY Adult : 6-10 mL/kg Children : 4 mL/kg SYMPTOMS OF INTOXICATION • Slurred speech • Disinhibited behavior • CNS depression • Decreased motor coordination & control • Hypotension: – decrease in total peripheral resistance • Reflex tachycardia HYPOTHERMIA Depresses central thermoregulatory mechanisms Decreases shivering Enhances heat loss through vasodilatation Sedative effects: lack of behavioral adjustment against exposure to the cold environment MANAGEMENT OF INTOXICATION Airway protection Adequate ventilation IVF replacement O2 supply EKG monitoring Thiamine (50 - 100 mg) IV Glucose supply (if hypoglycemic) Active charcoal (if co-ingestion is suspected) Re-warming (if hypothermic) Treatment is mainly supportive. Protect the airway to prevent aspiration. Glucose & thiamine administered. Glucagon is not effective for alcohol induced hypoglycemia. Correct hypothermia with gradual rewarming. Do not induced vomiting or activated charcoal and gastric lavage in pure ethanol intoxication. Consider gastric lavage only if the alcohol ingestion was massive and recent( within 30-45 min.). Hemodialysis efficiently removes ethanol but enhanced removal is rarely needed because supportive care is usually sufficient. Hemoperfusion and forced diuresis are not effective. BLOOD ALCOHOL CONC. • Legal definition of ethanol intoxication: BAC > 100 mg/dl • BAC correlates poorly with degree of intoxication (because of tolerance) BAC (mg/dl) Effects 20 - 50 fine motor function 50 - 100 judgment, coordination 100 - 150 Difficulty with walking & balance 150 - 250 Lethargy 300 400 - 500 Coma Respiratory depression, Hypotension, Hypothermia Convulsion, Death EFFECTS IN NON-ALCOHOLICS STAGE ONSET SYMTOMS I 6 - 8 hours Tremor, agitation, nausea, vomiting II 24 hours Hallucinations III 24- 48 hours Grand mal seizures IV 3 - 5 days Delirium tremens STAGING OF WITHDRAWAL Rx : ALCOHOL WITHDRAWAL • Hydration with D5NS (IV) • Cross-reacting drugs: – BZD or Phenobarbital • Thiamine (IV) • Magnesium sulfate (IV) • Admission: – fail to respond to 2 doses of sedative Methanol Physical Nature Wood alcohol CH3OH Colorless liquid Boiling point: 65°C Source Anti-freeze agents Solvents Cleaning agents Industrial alcohol Dye Poisoning Poisoning is common. Adulterated beverages (substituting methanol for ethanol) Mis-swallowing accidentally Suicide or homicide Ingestion of just 0.15 mL/kg of 100% methanol may cause toxicity. Fatal dose : 60-240 mL Pediatric cases are usually accidental. Adult cases usually involve suicidal ingestion or ingestion of methanol as an alcohol substitute. Toxic effects are typically severe, if untreated. Death may occur in untreated patients. Inhalation or dermal absorption can produce toxicity. Absorption Gastrointestinal Tract Skin Respiratory Tract Metabolic Pathway Methanol Alcohol dehydrogenase Formaldehyde Aldehydedehydrogenase Formic acid Tetrahydrofolate CO2+ H2O Methanol Metabolism Enzyme Involved: –Alcohol Dehydrogenase(Rate-Limiting) –AldehydeDehydrogenase Toxic Products: –Formaldehyde –Formic acid Formic Acid Toxicity Inhibition of mitochondrial cytochrome oxidase: –Histotoxic Hypoxia –Metabolic Acidosis Elimination Liver (predominates) Lung Kidney Elimination half life: 3 hours Clinical feature Incubation Time 12-72 hours Factors influencing time to symptoms: –Amount Ingested –Concomitant Ethanol Intoxication –The individual’s Folate Status Premortal Vital Signs Hyperpnea usually develops to compensate metabolic acidosis(Kussmaul’s Respirations) Sudden Respiratory Arrest Tachycardia Blood pressure is stable until death Hypotension may develop late in severe cases. Neurologic Toxicity Neurologic Symptoms: –Headache –Dizziness –Amnesia –Restlessness –Acute Mania –Lethargy –Confusion –Coma –Convulsions –Parkinsonism may develop as a sequelae of severe intoxication. Ophthalmologic Toxicity Occur when serum pH drops below 7.2 Low pH → intracellular concentration of formate↑ Improvement of vision with correction of acidosis, because formate moves out of the cell Formate is an inhibitor of cytochrome oxidase, which could inhibit ATP formation in the optic nerve leading to a stasis of axoplasmic flow, axonal swelling, optic disc edema and finally loss of visual function Ophthalmologic Toxicity Symptoms: Blurred Vision Photophobia Eye Pain Partial or complete loss of vision Visual hallucinations (bright lights, snowstorm, dancing spots, flashes) Ophthalmologic Toxicity Signs: Optic discs hyperemia Retinal edema Retinal vessels engorgement Papilledema Papillary dilation Loss of papillary reflex Gastrointestinal Toxicity Hemorrhagic Gastritis Acute Pancreatitis Symptoms: •Abdominal Pain •Nausea •Vomiting •Diarrhea •Liver Function Impairment Laboratory Tests Essential Tests: 1.Serum Electrolytes (Hyperkalemia) 2.Leukocytosis 3.Amylase elevations 4.BUN and Creatinine 5.Glucose (Hyperglycemia) 6.Arterial Blood Gases Elevated anion gap acidosis supports the diagnosis. 7.Osmolar gap 8.Elevated lactate levels 9.Serum Methanol Level (greater than 20 mg/dL) Early diagnosis History-taking Increased osmolar gap Blood methanol detection Late diagnosis Visual symptoms Metabolic acidosis with increased anion gap History of alcohol consumption and methanol contact Treatment Supportive Care Antidotes Hemodialysis Sodium Bicarbonate Folic acid Supportive Treatment Airway management in comatose patient Intravenous Fluids Cardiac Monitoring Oxygen Supply Ipecac is contraindicated (CNS depression) Activated charcoal is not effective Sodium bicarbonate Antidotes Fomepizole Ethanol Fomepizole Fomepizole(Antizol) Fomepizoleis the preferred agent 4-methylpyrazole (4-MP) “Fomepizole”:a more potent inhibitor of alcohol dehyrogenase No side effect of CNS depression as in ethanol therapy Fomepizole Indications: A history of ingestion when a serum level is not immediately available A Serum methanol level greater than 20 mg/dL Unexplained metabolic acidosis with elevated anion and osmolar gaps Fomepizole Metabolic acidosis with elevated anion gap accompanied by visual signs and symptoms Unexplained coma with a high osmolar gap Clinical evidence of toxicity Fomepizole Contraindication Disulfiram Allergic reaction to fomepizole Relative contraindication Metronidazole GI Ulceration Child < 5 years Severe Hepatic Disease Fomepizole L.D: 15mg/kg (IV) M.D: 10mg/kg/12h for 4 doses then 15mg/kg/12h Each dose is diluted in 100 mL normal saline or D5W and infused over 30 minutes. Ethanol Ethanol is a preferential substrate for alcohol dehydrogenase. Once alcohol dehydrogenase metabolism is blocked, methanol is eliminated slowly via pulmonary and renal excretion. Ethanol Indications: A history of ingestion when a serum level is not immediately available A Serum methanol level greater than 20 mg/dL Unexplained metabolic acidosis with elevated anion and osmolar gaps Ethanol Metabolic acidosis with elevated anion gap accompanied by visual signs and symptoms Unexplained coma with a high osmolar gap Clinical evidence of toxicity It may be used if fomepizole is not available Ethanol Loading Dose Gram/kg of Ethanol 10% (Oral) Non-Drinker/Child 0.88 Average Drinker 1.4 Chronic Drinker 2 Maintenance Dose 100 mg/kg/hour of Ethanol 10% (Oral) Increase M.D. 2-3 times during hemodialysis Ethanol Conc. to 100 -150 mg% Enhanced Elimination Hemodialysis effectively removes methanol and its toxic metabolites Elimination rates: -142 ~ 286 ml/min (methanol) -148 ~ 203 ml/min (formate) Peritoneal dialysis also removes methanol but not as effectively Adjunctive Treatment Folate or tetrahydrofolate(Leucovorin) to hasten elimination of formic acid. Leucovorin1mg/kg Max 50 mg/dose/IV/4-6 hours until methanol becomes undetectable. Folate 1mg/kg Max 50 mg/dose/P.O/4-6 hours until methanol becomes undetectable. Metabolic Pathway Methanol Alcohol dehydrogenase Formaldehyde Aldehydedehydrogenase Formic acid Tetrahydrofolate CO2+ H2O Overdose ETHYLENE GLYCOL Ethylene glycol is a sweet, odorless and colorless liquid. Overdose ETHYLENE GLYCOL Introduction It is a common component of antifreeze used in: Heating and cooling systems Brake Fluid Inks It is used as an industrial solvent in: Paints Plastics It is used in synthesis of: Resins Synthetic Fibers Waxes Epidemiology Poisoning is uncommon. Death occurs in patients who do not receive medical care. Poisoning most commonly occurs: Accidental ingestion Suicidal Attempt Pathophysiology E.G ADH Glycoaldehyde ADH Glyoxalate Pyridoxine Oxalate Glycine Itself is non-toxic Toxicity being to… Ethylene glycol Fatal dose in adult : 100 mL Clinical feature The first phase: 3 min –12 hours Resemble ethanol intoxication without alcohol smell Nausea, Vomiting & hematemesis The major effects are on the CNS Coma Seizure Nystagmus The second Phase: 12 –14 hours Tachycardia Mild Hypertension Pulmonary edema CHF Due to deposition of calcium oxalate within the vascular tree, myocardium and lung parenchyma The third phase: 24 –72 hours Flank pain CVA Tenderness (costovertebral angle) Acute tubular necrosis Treatment Focus treatment: Supportive care Treatment with fomepizole Treatment with ethanol Hemodialysis as indicated. Adjunctive Therapy Pyridoxine and thiamine to hasten elimination of toxic ethylene glycol metabolites. Pyridoxine Dose 1 to 2 mg/kg administered intravenously every 6 hours until ethylene glycol level is undetectable. Thiamine Dose Adult dose is 100 mg/I.V. over 5 minutes every 6 hours until ethylene glycol level is undetectable. Pediatric dose is 50 mg/I.V. over 5 minutes every 6 hours until ethylene glycol level is undetectable. Sodium Bicarbonate Sodium bicarbonate should not be used routinely but may be used as a temporarily for life-threatening acidosis prior to hemodialysis.