Revenue Cycle 101 - Central Ohio HFMA Chapter
advertisement

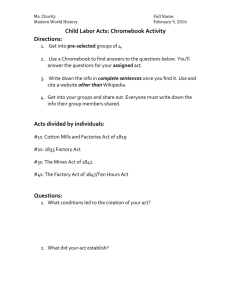
Revenue Cycle Management 3/17/2016 1 Here’s What You’ll Learn Introduction to Revenue Cycle Concept Zero to Zero Departments & Functions Process Key Definition & Metrics Market Conditions Impact to Revenue Cycle Modern Day Bounty Hunters Charity Care Future with Health Care Reform 3/17/2016 2 What is Revenue Cycle? All the administrative and clinical functions, processes, and software applications that contribute and manage the registration, charging, billing, payment and collections tasks associated with a patient encounter. Revenue Cycle is the process that begins when a patient comes into the system and includes all those activities that have occurred in order to have a zero balance In other words, think… 3/17/2016 Zero to Zero! 3 Importance of Revenue Cycle And You… “Hospitals exist in a very uncertain time. Reimbursement risk runs high, and receiving payments from patients is not guaranteed. The ability to capture lost revenue and improve the ability to forecast actual revenue received to the budget is necessary for hospitals' and other service providers' survival and vitality.” Source: Wall Street 2010 The Revenue “Cycle” SCHEDULING POST PAYMENT REVIEW REGISTRATION INSURANCE VERIFICATION CASH POSTING POINT OF SERVICE COLLECTIONS PROGRAM ADMINISTRATION SELF PAY COLLECTIONS CULTURE CUSTOMER SERVICE PROCESS PEOPLE FINANCIAL CLEARANCE TOOLS FINANCIAL COUNSELING DENIALS MANAGEMENT THIRD PARTY FOLLOW- UP CASE MGMT/QUR BILLING CDMP MEDICAL RECORDS CDM/CHARGE CAPTURE Process Flow by Department Patient Access Scheduling Hospital Care Delivery Documentation Of Services Charge Master Billing Claims Editor Receivables Management Payment Posting Case PreRegistration Management Transcription Bill Secondary Reconciliation Billing Utilization Eligibility & Verification Management Coding/ CDMP Claims Submission Financial Counseling Discharge Planning Charge Capture Appeals/ Contractual Denial Mgmt Adjustments Registration Patient Discharge Late Charges Patient Statements Follow-Up Bad Debt/ Write Offs Legal Collections Feedback Customer Service Customer Inquiries Issue Resolution Patient Access The “Front Door” to the hospital and the first step in the revenue cycle process for the majority of patients. The important functions and information gathered in Access include: 3/17/2016 Scheduling services (surgery not included) Verifying of Insurance Obtaining Authorizations and certifications Gathering patient demographics and insurance information Pre-Services/Point of Service collections Identifying the referring physician Informing the patient on instructions for the date of service, referral process, etc. Informing patient of referral process Financial Counseling Medicaid Eligibility/Charity Care Responsible for 50% of claims data 7 Health Information Management (HIM) Health information management (HIM) is the practice of maintenance and care of health records by traditional and electronic means in hospitals, physician's office clinics, health departments, health insurance companies, and other facilities that provide health care The important functions and information gathered in HIM include: Providing and Managing Transcription Services Coding services documented by Physicians CPT codes (procedures) ICD-9 (diagnosis) HCPC (supplies, drugs, etc.) ASC Codes Ensure Codes accurately reflect patient services Acts as a Liaison between all areas Serves as Subject Matter Experts in HIPAA, Documentation and Coding Educates, presents, and trains on opportunities to improve Case Mix Index (CMI) Oversees and responds to Defense Audits Manages storage and retrieval of medical records Implementation of Electronic Health Record System Building the Compliant Documentation Management Program (CDMP) 3/17/2016 8 Patient Financial Services (PFS) Patient Financial Services is the “cash machine” of the hospital. The important functions and information gathered in PFS include: Charge Master/Revenue Integrity Billing Overseeing Claims Edits to ensure “Clean Claim Submissions” Employing tools to ensure accuracy in charge capture Follow-Up with Insurance companies Customer Service Collections Cash Posting Subject Matter Experts Government Billing Commercial and Managed Care Billing Employs and Oversees systems and vendors to enhance 3/17/2016 Appeals Denials Un-paid Claims Services provided to patients Revenue Cost to Collect 9 Charge Master A comprehensive listing of hospital charges The Revenue Integrity team are a critical component to billing compliance and charge capture and is often considered the "life blood" to a Hospital's Revenue Cycle by touching almost every department within the facility. 3/17/2016 Standardization of charge master Department level review of all processes and charges with management staff to ensure all billable charges are represented on the CDM CDM reviews and updates to ensure compliance for all payors Market pricing, transparency and defensibility strategies Revenue cycle system mapping to ensure charge capture and compliant billing Acuity-based charging methodology development and implementation Maintenance strategies, controls and tools for maintaining an accurate and compliant CDM Educational and training tools 10 The Importance of Charge Capture A key part of the Revenue Cycle but does not report to Revenue Cycle “Bill what you do” – the process where services provided are entered into the system; charges and expected reimbursements are calculated The important functions and information gathered in Charge Processing include: Keyers and coders enter data automatically from a charge master or manually input Claims Manager software scrubs entries for correctness Problems sent to department work file for processing or corrections Reconciliation performed to insure all entries received and entered into the system Accuracy of service and charge Appropriate edits to scrub data Charge entered timely for prompt payment Daily Charge Logs Reviewed 3/17/2016 11 Process Flow: For Real? Process Flow Overview Revenue Cycle – Where Does the Information Come From? Required Billing Elements - Where do they come from? Required Elements: 50% - Patient Access, Registration 15% - Medical Records 15% - Charge Entry Areas 20% - Billing Patient Demographic Data Patients last name, first name, and middle initial Patient address Birth date Male (M) or Female (F) Marital Status Admission date or start of care date Encounter Specific Hour patient was admitted for inpatient or outpatient care Occurrence Codes Code indicating the priority of admission--1 indicates emergency; 2 urgent; 3 elective; 4 newborn; and 9 information not available. Code indicating the source of admission or outpatient service Provider has patient signature on file permitting release of data (Y or N) Principal Diagnostic Coding (ICD-9-CM code) Admitting Diagnostic Coding (ICD-9-CM code) Insurance Information The name and number identifying each payer that payment is expected Assignment of benefits (Y) yes; (N) no The name of the patient or insured individual Relationship of the insured (person having insurance) to the patient Insured’s identification number assigned by the payer organization The group name/plan through which the insurance coverage is provided The insurance group number Employment status code Employer’s name and address Access: Metrics Registration accuracy rate Denials No Authorization Not Eligible Telephone Statistics Hold Times Abandonment Rates Other Point of Service Collections “Red Flags” – Incorrect Claim Demographics 3/17/2016 15 HIM: Metrics Discharges Not Final Billed (DNFB) Turnaround Times Dictation/Transcription Record Requests & TAT CDMP Queries Rate Response Rate Agreement Rate RAC Audits & Timeliness Responses 3/17/2016 16 PFS: Metrics Cash Expected Reports Days in A/R Aging Analysis by Payer Unbilled Accounts Receivable Late Charge Postings by Service Area Claim Denial Volumes / Amounts / Types Bad Debt / Bad Debt Recovery Levels Cost to Collect 3/17/2016 17 Top Issues Influencing Health Care Industry Record spending on health information technology Significant changes in benefit plan design, plan pricing and the health plan landscape New risks and opportunities may emerge as payment models shift from fee-for-service to new models that focus on performance, health outcomes and shared cost savings Health organizations may feel the trickle down effect of decreased utilization by price sensitive consumers. A further uptick in merger and acquisition activity to share administrative burdens and IT investments, gain market share and fill strategic gaps. Pharmaceutical companies see an opportunity to increase their visibility with consumers, influence health outcomes and reduce healthcare costs while increasing revenue using digital strategies and technology. The use of mobile health and wireless technologies by all health organizations is expected to continue to surge. Source: PwC 2010 18 Revenue Stream Where the Money Comes from... Source: OHA 2010 19 Insurance by Percentage Enrolled Source: Kaiser Family Foundation 2010 20 Average Health Insurance Premiums and Worker Contributions for Family Coverage, 1999-2009 $13,375 131% Premium Increase $9,860 $5,791 $4,247 128% Worker Contribution Increase $1,543 1999 $3,515 2009 Employer Contribution Worker Contribution Note: The average worker contribution and the average employer contribution may not add to the average total premium due to rounding. Source: Kaiser/HRET Survey of Employer-Sponsored Health Benefits, 1999-2009. 21 On the Rise… Group Health Plan premiums up 9% with expectations of 6% in 2012 High Deductible Health Plans continue to rise Deductibles and Out of Pockets Increasing 22% Charity Care, Government Payors Increasing 1.3 Million Uninsured equivalent to the population of Columbus 22 Adults Living in Poverty 3/17/2016 23 Market Conditions State budget issues continue Traditional Medicaid/Medicaid Managed Care wanting relief More Ohio residents live below the poverty level High Penetration of Self-Insured Employers Shifts of health care costs to Consumers Increases in Deductibles Increases in Co-Pays But, still coverage offered from employers Most markets are dominated by few payors Smaller Payors being closed out of the Market Aggressive Managed Care payors Movements to more complicated contracts 3/17/2016 24 Market Conditions Reimbursement Variances Commercial Payors Continue to Subsidize Government Payors High Deductible Health Plans Increase Deductibles increasing too Quality Scores tied to Contract Increases/Consumerism Hospitals Physicians Multi-Year Contracts with Payors Transparency Growing 3/17/2016 25 Charges, Payments, and Cost Charges are the amount the hospital lists as the price for services. Very few pay this “sticker price.” Payment or Reimbursement is the amount the hospital actually receives in cash for its services. Private insurers, public insurers, Self Pay and the uninsured all pay different amounts for the same services. Payment can be either more or less than what it costs the hospital to provide a given service. Cost is what it actually costs the hospital to provide the services. 3/17/2016 26 Reimbursement Methodologies Hospitals Percent of Charge Per Diems Case Rate Payment Ambulatory Patient Groupings (APGs) Ambulatory Payment Classifications (APCs) Other 3/17/2016 Diagnosis Related Groups (DRGs) Medical Severity (MS) DRGs Globals Professional Services Fee For Service discounts Fee Schedules Payment based on Resource Based Relative Value Based System (RBRVS) Capitation Withholds Pools Case Rates Carve-Outs 27 Subsidies and Payor Mix Cost Government Reimbursement Commercial Reimbursement Charge Note: Solid lines are status quo; dashes represent future state with costs, reimbursement, and charges shifting. 3/17/2016 29 3/17/2016 30 Contracted Fee Schedule Match Source: AMA 2011 National Insurer Report Card 31 Administrative Costs Pre-Authorizations Complex Benefit Designs Limitations of Network Denials Coordination of Benefits Audits 3/17/2016 32 Importance of POS Collections Recent Studies on the “Tipping Point” – Financial Hardship Limit – found that when the total amount billed to the patient reached 3.5% of the family's gross income, the likelihood of paying the bill dropped dramatically. 33 3/17/2016 Source: TransUnion/NorthShore LIJ Study Modern-Day Bounty Hunters RAC: Recovery Audit Contractors Medicare MAC: Medicare Administrative Contractors The new Fiscal Intermediary MIC: Medicaid Integrity Contractors Medicaid Managed Care Audits 3/17/2016 34 RACs Findings 4% 2% 6% 4% 35% 40% 8% 17% 85% Outpatient SNF Rehab 3/17/2016 Inpatient Other Incorrectly Coded Other No/Insufficient Doc Medically Unnecessary 35 Charity 9 8 An IRS study found that 9 percent of revenue was spent on community benefit. 7 3-7 percent of revenue on a variety of community benefit and charity care activities is likely adequate. 6 5 Nearly 60 percent of the hospitals surveyed provided less than or equal to 5 percent of revenue on uncompensated care 4 3 2 1 Twenty percent of hospitals surveyed reported total community benefit spending of less than 2 percent of revenue. Source: Kaiser Daily Health Policy Report Feb 2009 Revenue Cycle Management Strategies A CFO’s Focus on Revenue Cycle Vendor Management Denials Management Technology Optimization Point of Service Collections Strategic Pricing Contract Management Compliance Documentation/Coding. Source: Interview with: Vince Schmitz, Senior Vice President & CFO, MultiCare Health System. 3/17/2016 37 Revenue Cycle & Health Care Reform Revenue Cycle improvements Positioning for the Future Expanded Coverage Payment Cuts New Coverage Requirements New Economic Incentives Eligibility Processes Denials Prevention Charity Care Policies & Processes ICD-10 C2C Rational Pricing Documentation & Coding Physician Integration ACO/Bundled Payments QUESTIONS