Assessment of fluid accumulation - Dietitians in Nutrition Support
advertisement

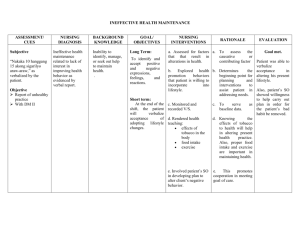
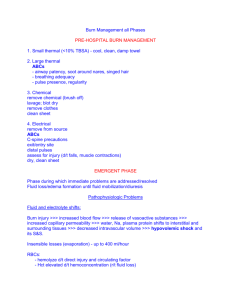
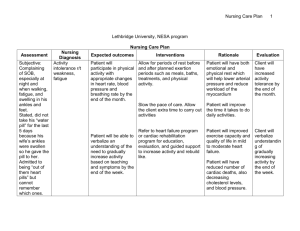
ABDOMINAL EXAMINATION AND THE ASSESSMENT OF FLUID ACCUMULATION Susan Roberts, MS, RD, CNSC Andrea JeVenn, RD, LD, CNSC THE ABDOMINAL EXAMINATION ANATOMY AND TERMINOLOGY RUQ Right lobe of liver, gallbladder, pylorus, first 3 parts of duodenum, head of pancreas, right suprarenal (adrenal) gland, right kidney, right colic (hepatic) flexure, sup. part of ascending colon, right half of transverse colon RLQ Cecum, appendix, most of ileum, inferior part of ascending colon, right ovary, right uterine tube, right ureter LUQ Left lobe of liver, spleen, most of stomach, jejunum & proximal ileum, body & tail of pancreas, left suprarenal (adrenal) gland, left kidney, left colic (splenic) flexure, sup part of descending colon, left half of transverse colon LLQ Sigmoid colon, inf part of descending colon, left ovary, left uterine tube, left ureter COMPONENTS OF EXAM Inspection • Visual review • Assess symmetry and contour Auscultation • Assess bowel and vascular sounds • Done prior to palpation Percussion • assess location & density of underlying body masses/organs, gas/fluid patterns AUSCULTATION Use diaphragm of stethoscope Begin in RLQ (ileo-cecal valve) Listen in each quadrant • What are bowel sounds? • Gas and fluid movement • Active • Hypoactive • Absent BOWEL SOUNDS Hyperactive Hypoactive • Increased motility • Decreased motility • Stenosis • Inflammation • Early SBO • Paralytic ileus • Resolving ileus • Peritonitis • Gastroenteritis • Surgical manipulation • Late SBO • Lower lobe pneumonia PERCUSSION Light tapping on abdomen • Assess size and position of solid organs • Differentiate gas versus liquid vs solids Tympany Dullness ILEUS Absence of peristalsis or function • Lack of mechanical issue Causes • Peritonitis • Sepsis • Medications, especially narcotics • Metabolic disturbances • Hyperglycemia and hypokalemia Absent or hypoactive BS Abdominal distention ILEUS MILD ILEUS ILEUS ILEUS IN NEONATE BOWEL OBSTRUCTION Defined as a partial or complete blockage Causes • Extrinsic • Adhesions, volvulus, or hernias • Intrinsic • Tumor, stricture, stenosis • Intraluminal • Bezoars, fecal material, gallstones BOWEL OBSTRUCTION General signs & symptoms Tests • Abdominal film • Distention • CT • Hyperactive or high pitched BS • UGI and/or small bowel series • Minimum rebound • Crampy pain SITE OF OBSTRUCTION Proximal Distal • Acute onset • Less vomiting • Greater vomiting • Greater explosive diarrhea • Bilious emesis • Less distention • Greater distention POSSIBLE OBSTRUCTIONS IMAGING STUDY OF OBSTRUCTION Barium was instilled through a nasogastric tube Picture shows loops of bowel >4cm in diameter Green arrow shows transition point ILEUS VS OBSTRUCTION Ileus • No source of obstruction • Gas in colon/rectum • Distention but without pain • May have bowel sounds ASSESSING FLUID ACCUMULATION WHAT IS FLUID RETENTION? Abnormal retention of fluid in interstitial spaces and cavities (e.g., peritoneal/abdominal cavity) • may not clinically manifest until it accounts for at least 10% of body weight or fluid volume is increased by 2.5-3 liters • fluid accumulation around the heart, in the lungs, small pockets of ascites, or hematomas may only be seen on imaging studies Braunwald, Loscalzo. Ch 36: Edema. In: Longo DL, Kasper DL, et al. Harrisons Principles of Internal Medicine; 2012 Epocrates: Evaluation of Peripheral Edema; accessed 11/26/14 Sterns RH. Clinical manifestations and diagnosis of edema in adults; UpToDate 1/30/14 Ch 15: I have a patient with edema. How do I determine the Cause? In: Symptom to Diagnosis: An Evidence-Based Guide; 2009 Causes Conditions Associated with Fluid Accumulation Increased capillary hydrostatic pressure Hypervolemia; kidney disease, pregnancy, CHF Loss of plasma proteins Kidney disease, liver disease, burn victims, malabsorption, malnutrition Obstruction of lymphatic Obstructing tumor, infection, damages to the lymph nodes or lymph node removal (cancers) circulation Increased capillary permeability Usually from inflammatory response or response to infections ACADEMY / ASPEN CLINICAL CHARACTERISTICS – EDEMA / FLUID ACCUMULATION Context Malnutrition Chronic Illness or Social / Environmental Acute Illness or Injury Circumstances Moderate Severe Moderate Severe Edema Mild Moderate to severe Mild Severe White et al, Characteristics for identification/documentation of adult malnutrition; JPEN 2012 ACADEMY / ASPEN CLINICAL CHARACTERISTICS – EDEMA / FLUID ACCUMULATION • Weight loss is frequently masked by fluid retention and weight gain may be present • If severe, can also mask evaluation of muscle/fat loss • Usually SUPPORTIVE evidence - RARELY ever directly related to malnutrition White et al, Characteristics for identification/documentation of adult malnutrition; JPEN 2012 ASSESSING FLUID RETENTION • Primarily found in dependent areas such as the sacrum, ankles, feet, calves, scrotum, vulva • The clinician may evaluate generalized or localized fluid accumulation during a physical exam • Localized: • extremities, abdomen (ascites), vulva/scrotal area • Generalized: • if severe, is referred to as anasarca DEPENDENT EDEMA – AMBULATORY PATIENTS: LEGS, ANKLES, FEET DEPENDENT EDEMA – BED BOUND PATIENTS: SCROTUM, VULVA, SACRUM Additional fluid OTHER AREAS: EDEMA AND ASCITES ASSESSMENT STRATEGY • Perform general survey, then head-to-toe • Use inspection and palpation • gloves optional • Determine if onset is acute vs chronic • Acute: < 72 hours • Chronic: better? worse? same? • Correlate physical findings of fluid accumulation with other evidence • vital signs, input/output records, labs, weight, history, imaging studies PALPATION TECHNIQUE Severity of edema is rated on a scale from +1 to +4 Press firmly but gently with your thumb for at least 5 seconds over • the dorsum of the foot • behind each malleolus • over the shins 0 Depth Description none No impression or distortion observed, bone structure easily identified mild 1+ 2+ 3+ 2 mm or less moderate 2 – 4 mm 4 – 6 mm severe 4+ 6 – 8 mm Slight pitting without distortion, rapidly disappears Somewhat deeper pit, distortion not easily apparent, disappears 10-25 seconds later Noticeably deep pitting, entire extremity looks full, swollen; indentation can last longer than 1 minute Very deep pitting, extremity is grossly misshapen, indentation lasts 2-5 minutes Table adapted from: Grading: Pitting Edema - http://www.med-health.net/EdemaGrading.html Grade FEASIBILITY OF ACCESSING DATA IN HOSPITALIZED PATIENTS… • Cross-sectional survey at 4 different hospitals: 2 tertiary teaching,1 urban, 1 rural; included 262 adults • Determined availability of data to support the proposed Academy/ASPEN malnutrition characteristics • Data on edema available at time of nutrition assessment • All patients – 84.4%, Non-ICU – 85.9%, ICU – 82.7% • Edema used as one of the characteristics to define malnutrition • All patients – 26.6%, Non-ICU – 16.2%, ICU – 39.1% Nicolo et al. JPEN 2013 SUMMARY • Nutritional and medical history, & current medical picture must be considered before determining whether fluid accumulation is a relevant characteristic to use in identifying malnutrition • Many patients have fluid accumulation but not all are malnourished • RARELY a direct result of malnutrition • Fluid accumulation may not always be readily visible • Fluid accumulation will falsely increase weight / mask weight loss and can prevent muscle mass / SQ fat assessment • Continue to partner with nurses, physicians and other health care team members to enhance assessment of fluid status