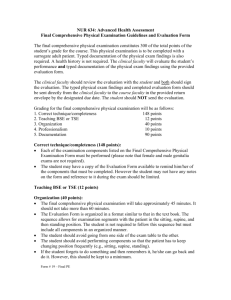
Health Assessment: Performing A Physical Examination
advertisement
An Overview Part of a general health assessment Used to gather data about the client Focuses on functional abilities and responses to illness/stressor The nurse performs a physical examination to: Establish baseline data Identify nursing diagnoses, collaborative problems, or wellness diagnoses Monitor the status of an identified problem Screen for health problems Comprehensive: Interview plus complete head-to-toe examination Focused: “Focused” on presenting problem Ongoing: Performed as needed to assess status Evaluates client outcomes Head-to-toe ◦ Starts at the head ◦ Progresses “down” the body ◦ System-related data found throughout: • Heart sounds - chest • Pulses - periphery Body systems ◦ Gathers system-related data all at once ◦ May be done in a predetermined order that mimics head-to-toe: • Neurological • Cardiovascular • Respiratory • Gastrointestinal Theoretical knowledge • A and P, techniques Self-knowledge • Skill and comfort level • Willingness to seek help Knowledge about client situation • Purpose of examination • Client diagnosis Privacy is key • Draping • Use of curtains Noise control • TV/radio off Enable visualization • Adequate lighting • Flashlight if needed Promote client comfort: Develop rapport Explain the procedure Respect cultural differences Use proper positioning Four major skills used: Inspection Palpation Percussion Auscultation Use of sight to gather data Used throughout physical examination Tools to enhance inspection • Otoscope • Ophthalmoscope • Penlight Examples: Skin color, gait, general appearance, behavior Use of touch to gather data Begin with light pressure, moving to deep palpation Use caution with deep palpation Parts of the hands used: • Fingertips: Tactile discrimination • Dorsum: Temperature determination • Palm: General area of pulsation • Grasping (fingers and thumb): Mass evaluation Examples: Edema, moisture, anatomical landmarks, masses Tapping on skin to elicit sound • Direct • Indirect Useful for assessing abdomen, lungs, underlying structures Examples: Distended bladder Use of hearing to gather assessment data Direct auscultation: • Listening without an instrument Indirect auscultation: • Use of a stethoscope to listen Diaphragm - high-pitched sounds Bell – low-pitched sounds Examples: Heart sounds, lung sounds Infants: Parents hold Attend to safety Toddlers: Allow to explore and/or sit on parent’s lap Invasive procedure last Offer choices Use praise Preschoolers: Use doll for demonstration Still may want parental contact Allow child to help with examination School-Aged Children: Show approval and develop rapport Allow independence Teach about workings of the body Adolescents: Provide privacy Concerned that they are “normal” Use examination to teach healthy lifestyle Screen for suicide risk Young/ Middle Adults: Modify in presence of acute or chronic illness Older Adults: May need special positioning related to mobility Adapt examination to vision and hearing changes Assess for change in physical ability Assess for ability to perform activities of daily living Provide periods of rest as needed Begins at first contact Overall impression of client Deviations lead to focused assessments • Appearance/behavior • Grooming/hygiene • Body type/posture • Mental state • Speech • Vital signs • Height/weight Integumentary: Skin characteristics • Color • Temperature • Moisture Lesions Hair Nails • Texture • Turgor Head: Skull and Face • Size • Shape • Facial features Eyes • External eye • Sclera • Pupils • Visual acuity • Vision examinations Acuity, distance, near, color, visual fields • Internal structures Head: Ears/hearing • External ear • Inner ear Tympanic membrane • Hearing Weber’s test Rinne’s test • Balance Romberg’s test Nose • Smell Mouth • Lips • Buccal mucosa • Teeth • Hard and soft palates Neck: Musculature Trachea Thyroid gland Cervical lymph nodes Breasts: Size Shape Nipple characteristics Tissue Include axillae Chest and Lungs: Describe size and shape of chest Relate findings to landmarks Breath Sounds: Bronchial Bronchovesicular Vesicular Adventitious Diminished or misplaced Abnormal vocal sounds Cardiovascular– Heart: Inspection • PMI • Heaves/Lifts Palpation • Thrill Heart sounds Location: • Aortic, Pulmonic, Tricuspid, Mitral Components: • S1, S2, S3, S4 Murmurs Cardiovascular– Vessels: Central vessels • Carotid arteries Palpate pulsation * Special precautions Auscultate for bruit • Jugular veins Peripheral vessels • Blood pressure • Peripheral pulses • Signs of inadequate oxygenation • Varicosities Different order for assessment skills • Inspect • Auscultate • Percuss • Palpate Body shape/symmetry: Joint mobility: Posture Gait Spinal curvature Balance: Romberg’s test Coordination: Finger-thumb opposition Movement Color change Deformity Crepitus Muscle strength: Range of motion Resistance Staff RN Uses Focused Neuro Assessment: Cerebral Functioning: Level of consciousness • Arousal - response to stimuli • Orientation - time, place, person Mental status/cognitive function • Behavior, appearance, response to stimuli, speech, memory, communication, judgment Reflexes: Automatic responses Responses on a graded scale • 0 = No response • 4 = Clonus Example: deep tendon reflexes Motor/Cerebellar Function: Movement/coordination Tone Posture Equilibrium Proprioception Sensory Function: Light touch Light pain Temperature Vibration Position Sense Stereognosis Graphesthesia Two-point discrimination Point localization Extinction Male: Includes reproductive information External genitalia: penis, urethral opening, scrotum, lymph nodes, pubic hair Examine for the presence of a hernia Female: Female external genitalia: labia, clitoris, urethral opening, vaginal orifice, pubic hair, lymph nodes Other: Kidneys (CVA tenderness) Bladder (palpation of the abdomen) NP/MD responsible for anus, rectum, prostate examination NP/MD responsible for pelvic examination