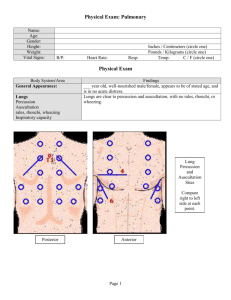
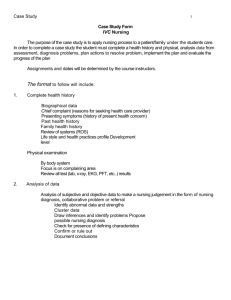
Assessment techniques
advertisement

Health History and Physical Assessment Lecture 1 HISTORY and PHYSICAL ASSESSMENT OBJECTIVES • Discuss different methods and the sequencing used for basic physical assessment for each body system • Describe the components of the complete health history • Identify significant findings of a health history and physical assessment of a patient • Discuss the normal assessment and common abnormal findings for each body system • Successfully complete a physical assessment practicum Health History Physical Assessment • Subjective database • Objective database • Obtained through interview • Obtained by observation and physical assessment techniques • Use of effective communications skills • Completes the client’s health picture Historical information often comes from a variety of sources, including • The patient • The family • Friends • Other observers Complete Health History • Biographical data • Chief complain • History of Present Illness • Past Health history • Family History • Functional Assessment ( Activities of Daily Living): Diet, sleeping, exercise, coffee, alcohol, drugs, tobacco Biographical Data • Name: • Age: • Gender: • Marital status: • Occupation: Complete Health History-Cont. • Chief complain: What brought you here today? (symptom/s & duration) • History of Present Illness – Arranges symptoms in chronological order from the time of onset to the present time. – Includes an Analysis of the Symptom Analysis of the Symptom • What What makes symptoms better/worse? • Describe What does pain feel like? • Where Where & where does pain go? • How On Scale of 1-10 (other scales) • When When, How often, How long? Past Health history • Major childhood & adult illnesses • Accidents and Injuries • Hospitalizations and Operations • Immunizations & dates: reactions to immunizations • Surgery: Dates, Complications • Medications: Current, past • Allergies: Medications, environmental, food. • Transfusions: Reactions, date & # of units if known • Emotional status: Mood disorders, psychiatric attention Family History • Any family members with illness • Age of parents: Age & cause of death if deceased • Age & number of siblings: Health Status • History of chronic diseases (ex: Hx of heart disease, hypertension, cancer, TB, diabetes, asthma, STD's, kidney, thyroid disease) • Major genetic disorders & health problems Father died at age 43 in train accident. Mother died at age 67 of stroke; had varicose veins, headaches One sister, died in infancy of unknown cause. Husband died at age 54 of heart attack Daughter, 33, with migraine headaches, otherwise well; son, 31, with Headaches Review of Systems • Inquires about signs and symptoms as well as diseases related to each body system Physical assessment Physical Assessment • Usually performed after the health history • Examiner must wash hands • Make the patient comfortable • Assessment must be systematic and organized • Head – to - Toe Assessment Assessment techniques • Inspection • Palpation • Percussion • Auscultation Assessment techniques - Cont. Inspection • Close and careful visualization of the person as a whole and of each body system • Ensure good lighting • Perform at every encounter with your client Assessment techniques - Cont. Palpation • Temperature, Texture, Moisture • Organ size and location • Rigidity or spasticity • Crepitation & Vibration • Position & Size • Presence of lumps or masses • Tenderness, or pain Assessment techniques Cont. Palpation Temperature, Texture, Moisture Organ size and location Rigidity or spasticity Crepitation & Vibration Position & Size Presence of lumps or masses Tenderness, or pain Palpation Techniques – Light – Deep Assessment techniques - Cont. Percussion • Technique that translates the application of physical force into sound • Assess underlying structures for location, size, density of underlying tissue. Percussion Technique Percussion Sounds Assessment techniques - Cont. Auscultation • Listening to sounds produced by the body • Instrument: stethoscope (to skin) • Diaphragm –high pitched sounds Heart Lungs Abdomen • Bell – low pitched sounds Blood vessels Nutritional Assessment • BMI • Dietary data – Food record – 24-hour recall – Diet diary • Conducting the Dietary Interview • Cultural and religious considerations Clinical Assessment Indicators of Nutritional Status • General appearance • Skin, hair, and nails • Mouth; includes teeth and gums • Neck; includes thyroid • Musculoskeletal • Abdomen • Nervous system • Height and weight