Paracetamol and Aspirin Poisoning
advertisement

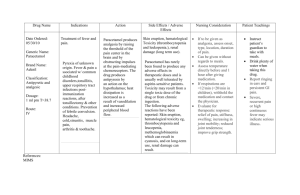
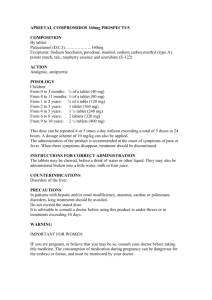
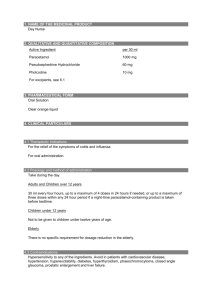
Paracetamol and Aspirin Poisoning Dr. SH Tsui 23 March 2005 Paracetamol • Very Common – 1054 registered pharmaceuticals contain paracetamol in HK • Perceived to be benign – But it can be lethal • Treatable – Early antidote Poisoning Data • Local – UCH database – About 1000 cases – Paracetamol 16% • US - TESS 2002 – 2.3 million exposure – Analgesics 10.8% – Paracetamol 4.9% – Salicylates 0.8% QMH data • • • • • May to October 1998 Total cases of DO: 205 Paracetamol involved: 33 (16%) Mortality: nil Paracetamol found without a history of intake: 4 • With potentially toxic level: 1 out of 4 Who will manage this case in A&E/Observation ward? • Young lady taken 12 tabs of panadol 3 hours ago? • Young man taken 20 tabs of panadol half an hour ago? • Paracetamol level at 4hr came back to be 896mol/L, LFT normal Who will continue to manage? Who will start NAC? • Who will give full course of NAC in their O ward? Pharmacokinetics • Potential toxic dose – >150mg/kg • Rapid absorption – Peak within 1-2 hour • Vd – 1L/kg • T1/2 – 2-3 hours, – Increased in overdose Metabolism • Non toxic metabolites APAP – Sulfate conjugate – Glucuronide conjugate • Toxic metabolites – NAPQI Urine (unchanged) • Determinants – Dose – P450 activity – 2E1 – polymorphism results in different susceptibility – Glutathione >90% Sulfate Glucuronide cytochrome P450 (IIE1, IA2, IIIA4) NAPQI Glutathione Glutathione depleted Mercapturic acid conjugates Cell Damage Liver toxicity • Central zone – Highest concentration of P450 – Lowest oxygen content • Massive centrilobular necrosis Risk factors for liver toxicity • Enzyme induction: smoking, barbituates, phentoin, isoniazids, ethanol • Decreased glutathione store: malnutritionalcoholism, HIV, chronic illness Renal toxicity – Consistent with acute tubular necrosis – P 450 in kidney – NAPQI formation – Not hepato-renal initially In massive overdose • CNS – Coma – P450 in brain, ? Mechanism • Metabolic – Metabolic acidosis, mitochondria dysfunction • Coagulopathy – Directly interfere with coagulation factors – Later 2o to liver failure Clinical Presentation I 0.5-24 Hours Nausea, vomiting, anorexia, pallor, or entirely normal appearance II 18-72 Hours Progressive laboratory and clinical signs of hepatic injury III 72-96 Hours Hepatic failure Multi-organ failure IV 4 to 14 Days Recovery or death Liver is entirely normal after recovery Must Screen Level • Paracetamol level – Approximately 1/500 poisoned cases where there is no history of paracetamol overdose has a level requiring therapy – Cost effective Ashbourne: Ann Emerg Med 1989:18:1035 Kulig: Ann Emerg Med 1985;14:562 Sporer KA, Am J Emerg Med.1996;14:443-6 Treatment • GI decontamination • Antidote • Liver failure – Supportive – Transplant GI decontamination • Early (< 4 hours) – Activated charcoal – GL for co-ingestion only • Late – No indication for decontamination in pure overdose – Activated charcoal consideration in mixed overdose Natural History of Untreated Overdose Mortality < 5% Hepatic failure 5-10% Clinical hepatitis 20-40% Chemical hepatitis 50-70% Renal failure 10% Efficacy of NAC – <8 hours - no morbidity and mortality – 8- 24 hours, 10-30% had AST>1000 Smilkstein: N Engl J Med 1988;319:1557 – 10-36 hours, reduce mortality in fulminant hepatic failure (58% Vs 37%) Harrison: Lancet. 1990 Jun 30;335(8705):1572-3 – 36-80 hours, reduce mortality (48% Vs 20%) Keays: Brit Med J 1991;303:1026 Smilkstein: N Engl J Med 1988;319:1557 Antidote : N-acetylcystecine • Mechanism of action in early phase – Major • Increases non-toxic sulfation • Precursor for glutathione – Minor • Directly conjugates NAPQI • Directly reduces NAPQI back to Paracetamol Antidote : N-acetylcystecine • Mechanism of action in late phase – Non-specific antioxidant – Impairs WBC migration to injury – Improves hepatic oxygen extraction Harrison: N Engl J Med 1991;324:1852 – Improves cardiac output Harrison: N Engl J Med 1991;324:1852 Indications for NAC Therapy – Level available < 8 hours • • – Level not available < 8 hours post ingestion • • – Treat first Make decision to continue or stop therapy based on level Late Presentation (>24 hrs post-ingestion) • • – Wait for level Treat if above nomogram Detectable paracetamol level Elevated AST Fulminant liver failure Nomogram • Paracetamol (g/ml) = 0.15 x Paracetamol (mol/L) Drawbacks of Normogram • Refers to single acute ingestion • Applicability to young children never been proved • Time of ingestion not always accurate in real life situation • Does not predict life or death IV NAC dose • 150mg/kg in 200ml D5 over 1 hour then • 50mg/kg in 500ml D5 over 4 hours then • 100mg/kg in 1000ml D5 over 16 hours • Total dose 300mg/kg in 21 hours • Rate-related side effect Anaphylactoid reaction Rash, utricaria, bronchospasm, hypotension Treatment of liver failure • Supportive treatment – NAC • 150mg/kg every 24 hours till death or recovery – Plasmapheresis – Bioartificial Liver (BAL) • Liver transplants – 50% survival in 10 years – Clinical Predictors Predictors of death in Paracetamol liver failure • Kings College’s criteria • Newer Predictors – Lactate • pH < 7.30 after volume – Phosphate resuscitation OR • Combination of 3 parameters – Stage III or IV encephthalopathy – PT > 100 seconds – Creatinine above 300µmol/L O’Grady: Gastroenterology 1989:97:439 Extended Release Preparations • First marketed in 1994 • Bilayered preparation contains ~650mg of paracetamol • Delayed dissolution and release of half of the drug Observations from case reports • 13 patients with overdose of ER formulation • Elimination phase was delayed in 8 patients • 3 patients had non-toxic levels at 4hr subsequently had levels in toxic range Cetaruk: Ann Emerg Med 1997; 30: 104-8 Recommendations • Check levels at 4 hour and then 4-6hrs later • NAC if either value is above treatment line • If 2nd level> 1st level, or lies close to toxic range, start NAC and obtain additional measurements Temple: N Eng J Med. 1995; 333: 1058-9 How about Fast Acting Paracetamol? • Paracetamol & sodium bicarbonate • Doubles the absorption rates • Syrup panadol overdose (Also fast absorption) Repeated Supra-therapeutic intake • • • • • >4gm for 24hr or more >90mg/kg/day for 24hr or more GI decontamination not a priority Normogram not applicable NAC if detectable paracetamol level or elevated liver enzyme • Continue NAC until 24hrs after last dose or improvement of patient Summary – Paracetamol • • • • • • Common overdose No clear early toxidrome Must screen with level Early therapy very effective Late therapy still efficacious Identify high risk patients for transfer to liver transplant unit Salicylates • Common anti-inflammatory, analgesic, antipyretics, and anti-platelet agent – 57 and 132 registered pharmaceuticals in HK contain aspirin and salicylate • Different preparations – Aspirin (acetyl salicylic acid) tablets – Enteric coated – Topical Preparations (methyl salicylate) • Dangerous -7gm of salicylate in 5 ml Pharmacokinetics • Absorption – Tablets dissolution is the rate determining step – Formation of concretion – Pyloric spasm – Significant dermal absorption, especially in diseased skin Brubacher JR: J tox clin tox 1996; 34(4):431-6 • Distribution – High protein-bound • saturated in overdose – Vd -0.15 → 0.35 L/kg – pH effect • Weak acid. pKa 3 pH effect • Alkalemia • pH of serum higher than that of CSF • HA Can cross membrane pH ↓ pH ↑ • Acidemia • H+ A- Cannot cross membrane • pH in serum lower than that of CSF Metabolism & Excretion • Therapeutic – Hepatic conjugation with glucuronic acid or glycine – Renal elimination insignificant • Overdose – Hepatic conjugation saturated – Renal elimination become important Pathophysiology • Uncouple the oxidative phosphorylation – Short circuit the mitochondria membrane potential – Generate heat instead • Inhibits dehydrogenase in Kreb’s cycle HA X H+A- Clinical Manifestation CNS – Tinnitus or hearing impairment – Confusion, lethargy, coma, seizure – Cerebral edema – Death Clinical Manifestation • Acid/Base – Early respiratory alkalosis • Hyperventilation by ↑RR or/and ↑TV – Mixed metabolic acidosis and respiratory alkalosis • Lactates, ketones and salicylates – Acidemia – decompensate and dying • pH < 7.4 – poor prognostic maker pH PCO2 HCOmmHG mmol/L Early 7.5 30 24 Later 7.4 30 20 Dying 7.3 45 20 Dying 7.3 30 16 Clinical Manifestation • • • • • • • GI - Vomiting Pulmonary – ALI CVS – Tachycardia Hyperthermia Sweating Hypokalemia Glucose Diagnosis & Severity assessment • History – >150mg/kg • Clinical manifestation - most important ! – Subtle in chronic poisoning (30% misdiagnosis) • FeCl3 test • ABG, electrolytes, urinalysis • Drug level – Therapeutic 15-30mg/dl – Serum Salicylates (mg/dL)=13.8x serum salicylates (mmol/L) – Serial trend Done Nomogram • Limitation – Assume all cases had a same pH – Clinically NOT useful Management • • • • GI decontamination ABC Alkalinization Extracorporeal removal GI decontamination • Gastric lavage – Acute large overdose – Spontaneous vomiting is common • Multiple dose activated charcoal – Reduce delayed absorption • Whole Bowel Irrigation for enteric coated tablets ABC • DO NOT allow respiratory acidosis during and following intubation • Kill the patient quickly • DO give aggressive volume resuscitation • Hypovolemia – – – – Vomiting Sweating Fever Hyperpnea ABC • Monitor blood glucose and correct hypoglycaemia • Maintain a high normal blood glucose • Maintenance IV Fluid: 1L D5 40 mmol KCL 3 amp of NaHCO3 • Adjust infusion rate and concentration • Monitor urine output, serum/urine pH and serum K level Alkalinization • Aim for both serum & urine alkalinization • Indications – Clinical Salicylism – Level > 40mg/dl • NaHCO3 – Bolus 1-2mEq/kg – Maintenance • Goal – Urine pH 7.5-8 – Serum pH 7.45-7.55 • K+ is important for success Extracorporeal removal • Indications – Vital end-organs toxicity – Failure of excretion – Failure of conservative management – Level • Acute > 100mg/dl • Chronic >60mg/dl • Methods – Hemodialysis – Charcoal hemoperfusion – Hemodialysis in series with hemoperfusion – Exchange transfusion in infants Are you going to manage this case? • F20, Ingested 1 pack of Cortal® 3 hours ago • C/O Nausea, otherwise asymptomatic • Amount of ingestion (Assume 50kg): 200mg/kg • Range of mild to moderate toxicity Summary - Aspirin • Another common overdose • Understand the pharmacokinetic • Recognize the clinical manifestation and how to assess the severity • Nomogram NOT useful clinically • Don’t allow acidemia • Treatment options available and their indications Thank you ! Dinner time