Hypertension Guide: Diagnosis, Management, and Secondary Causes
advertisement

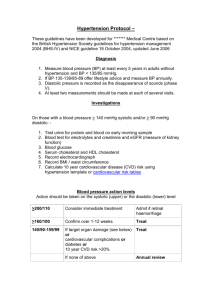
Cardiovascular [HYPERTENSION] Introduction Hypertension is defined by a systolic BP > 140 or a diastolic > 90. HTN is often an asymptomatic, chronic, age-related condition that worsens and contributes to atherosclerotic disease. In essential hypertension (primary hypertension) the cause is idiopathic and independent of any one given risk factor. This must be differentiated from secondary hypertension - hypertension attributable to some hormonal, structural, or metabolic condition. Essential is by far the most common but other causes must be investigated. Diagnosis In order to diagnose hypertension there must be two blood pressures taken at separate office visits that are greater than 140/90. Normal is 120/80. Pay attention to the severity/stage of hypertension. Remember the “20, 10, symptom rule”. Start at 120/80, then add 20 to the systolic and 10 to the diastolic to reach the next stage. Once at 180/120, the presence of end organ damage pushes from urgency to emergency. It’s important at the time of diagnosis to evaluate for acute end organ damage, which’d thrust the patient into the emergent category. Management Treatment is dependent on the stage of hypertension. For prehypertension the renoprotective benefits of ACE/ARB doesn’t decrease the number of events but does prevent progression of hypertension. For stage I, diuresis is the name of the game. If drugs are to be added, diuretics > ACE/ARBs > CCB. When it comes to Stage II, many permutations exist with the expectation that 2-4 medications will be required. If using β-Blockers combined vasodilators (Carvedilol) are better than nonvasoactive (Propranolol). When using CCB be aware that addition or increasing dose may take several days to see effect. α-blockers (like clonidine) should be avoided until no other options exist. Secondary Hypertension This is refractory hypertension caused by something. If the kidneys are nor perfused (renovascular, CHF, cirrhosis) then the kidney responds with an increased RAS (which means ANGII = HTN). A primary aldosterone secreting tumor produces aldosterone without renin. Pheochromocytoma causes the release of catecholamines. Hyperthyroid causes an increase in T3 metabolism. Even an isolated hypercalcemia can cause hypertension by accelerating plaque formation. Each are discussed in detail in other sections. Goals In general, the minimum goal is <140/<90. Every 20 point systolic increase OR 10 point diastolic DOUBLES the risk of a cardiovascular event. More stringent blood pressure control is required for diabetics (<135/<85, some would even say <130/<80). Hypertension Cavitation Alarm Symptoms 180/120? PO / IV BP Control Urgent / Emergent HTN Age >20, Age <70 Refractory, ↑↑HTN Secondary HTN Aldo:Renin Renal Art U/S CrCl TSH Ca CXR CBC Essential Stage Normal Pre-HTN Stage I Stage II Urgency Emergency SYS DIA 120 80 130 90 140 100 160 110 180 120 Alarm Sxs Initial Tx ?ARB? ARB Thiazide > ACE > CCB Comorbid Specific PO Meds (Hydralazine) IV Meds (Labetalol) Alarm Sx = Stroke, MI, Papilledema, Proteinuria, ARF, eclampsia, aortic dissection Condition CAD (pre-MI) Angina Post MI CVA PPX DM CKD Option CCB + ACE > β-Blocker + Diuretic β-Blocker β-Blocker + ACE ACE ACE ACE + Others CCB = Calcium Channel Blocker = Amlodipine β-Blockers = Propranolol, Labetalol, Carvedilol ACE/ARB = Lisinopril, Captopril, Losartan, Candesartan Type Renovascular History DM or glomerulonephritis ARF induced by ACE/ARB Renal Bruit, Hypo K Pheochromocytoma Hyperaldo Pallor, Palpitations, Pain, Perspiration, Pressure Refractory HTN or HTN and HypoK Weight Loss, Sweating, Heat intolerance, Palpitation, Polyuria, AMS, “moans, groans, bones, kidney stones” Hyperthyroid Hypercalcemia Workup CrCl BMP Aldo:Renin < 10 U/S Renal Artery 24-Hr Urinary metanephrines, CT Aldo:Renin > 20 CT Pelvis TSH, Free T4 Free Ca © OnlineMedEd. http://www.onlinemeded.org