Hyperinflation Therapy
advertisement

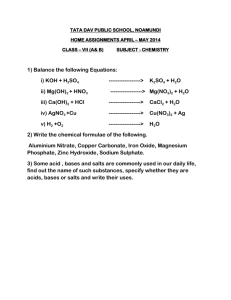
Hyperinflation Therapy IPPB Classification Flow Air-Mix Expiratory Time Pressure Sensitivity IPPB - Troubleshooting Loss of pressure Excessive pressure Failure to trigger inspiration Failure to cycle off Pressure does not rise normally A patient is receiving chest percussion, lung expansion therapy, and directed cough to treat obstructive atelectasis. Which of the following diagnostic procedures should be recommended to evaluate the patient's response to respiratory care? A. chest radiograph B. computed tomography (CT scanning) C. peak expiratory flow measurement D. body plethysmography A physician has ordered lung expansion therapy for a patient with atelectasis. The patient had a recent right lower lobectomy. Upon examination, the patient is alert, oriented, and has a nonproductive cough. Which of the following should the respiratory therapist recommend? A. chest physiotherapy and postural drainage B. IPPB C. incentive spirometry D. vibratory PEP While administering an IPPB treatment at 20 cmH2O to a patient with pulmonary emphysema, the respiratory therapist notes the patient has suddenly become very short of breath and cyanotic. The therapist's most appropriate action would be to A. suction the patient. B. discontinue the treatment. C. decrease the peak pressure to 10 cmH2O. D. stop the treatment for 10 to 20 minutes. The respiratory therapist is administering an IPPB treatment by mask to a patient who is unconscious. The machine cycles to expiration before the patient receives an adequate volume. Which of the following adjustments should the respiratory therapist make? A. Increase the cycling pressure. B. Increase the flow. C. Decrease the sensitivity. D. Decrease expiratory time. Which of the following patient categories are at high risk for developing atelectasis? I. Those who are heavily sedated II. Those with abdominal or thoracic pain III. Those with neuromuscular disorders A. I and II B. II and III C. I and III D. I, II, and III How do all modes of lung expansion therapy aid lung expansion? A.Increasing the transpulmonary pressure gradient B. Decreasing the transthoracic pressure gradient C.Increasing the pressure in the pleural space D.Decreasing the pressure in the alveoli How can the transpulmonary pressure gradient be increased? I. Increasing alveolar pressure II. Decreasing pleural pressure III.Decreasing transthoracic pressure A.I and II B.II and III C. I and III D. I, II, and III Which of the following is not a potential hazard or complication of IS? A. Pulmonary barotrauma B. Decreased cardiac output C. Respiratory alkalosis D. Fatigue A postop patient using IS complains of dizziness and numbness around the mouth after therapy sessions. What is the most likely cause of these symptoms? A. Gastric insufflation B. Hyperventilation C. Pulmonary barotrauma D. Respiratory acidosis Which of the following outcomes would indicate improvement in a patient previously diagnosed with atelectasis who has been receiving IS? I. Improved PaO2 II. Decreased respiratory rate III. Improved chest x-ray IV. Decreased forced vital capacity (FVC) V. Tachycardia A. I, II, and III B. I, III, and IV C. I, II, III, IV, and V D. III, IV, and V Ideally, when should high-risk surgical patients be oriented to IS? A.Postoperatively, after full recovery from the anesthesia B.Preoperatively, before undergoing the surgical procedure C.Postoperatively, while they are still in the recovery room D.Postoperatively, but no sooner than 24 hours after surgery In performing the SMI maneuver during incentive spirometry, the patient should be instructed to sustain the breath for at least how long? A. 10 to 15 seconds B. 5 to 10 seconds C. 3 to 5 seconds D. 1 to 2 seconds Which of the following is an absolute contraindication for using IPPB? A. Hemodynamic instability B. Active untreated tuberculosis C. Tension pneumothorax D. Recent esophageal surgery What is the minimum airway pressure at which the esophagus opens, allowing gas to pass directly into the stomach? A. 25 to 30 cm H2O B. 20 to 25 cm H2O C. 15 to 20 cm H2O D. 10 to 15 cm H2O Which of the following are potential desirable outcomes of IPPB therapy? I. Improved oxygenation II. Increased cough and secretion clearance III. Improved breath sounds IV.Reduced dyspnea A. II and IV B. I, II, and III C. III and IV D. I, II, III, and IV When checking a patient's IPPB breathing circuit before use, you notice that the device will not cycle off, even when you occlude the mouthpiece. What would be the most appropriate action in this case? A. Secure a new IPPB ventilator. B. Check the circuit for leaks. C. Decrease the flow setting. D. Increase the pressure setting Which of the following are appropriate initial settings for IPPB given to a new patient? A.Sensitivity –2 cm H2O; pressure 25 cm H2O; high flow B.Sensitivity –3 cm H2O; pressure 5 cm H2O; moderate flow C.Sensitivity –1 cm H2O; pressure 15 cm H2O; moderate flow D.Sensitivity –8 cm H2O; pressure 15 cm H2O; moderate flow The End I. II. III. IV. During IPPB therapy, a patient complains of dizziness and tingling sensations in her fingers. Which of the following should the respiratory therapist record in the patient's chart? medication administered during the treatment the patient's vital signs before and after the treatment the patient's symptoms the family's reaction to the patient's complaint A. I, II, and III only B. I, II, and IV only C. I, III, and IV only D. II, III, and IV only Persistent breathing at small tidal volumes (VTs) can result in which of the following? A. Reabsorption atelectasis B. Spontaneous pneumothorax C. Passive atelectasis D. Respiratory alkalosis Which of the following patient groups should be considered for lung expansion therapy using IPPB? I. Patients with clinically diagnosed atelectasis who are not responsive to other therapies II. Patients at high risk for atelectasis who cannot cooperate with other methods III. All obese patients who have undergone abdominal surgery A. I and II B. II and III C. I and III D. I, II, and III Which of the following is not a potential hazard of IPPB? A. Increased cardiac output B. Respiratory alkalosis C. Pulmonary barotrauma D. Gastric distension During administration of a CPAP flow mask to a patient with atelectasis, you find it difficult to maintain the prescribed airway pressure. Which of the following are most likely the problems? I. System or mask leaks II. Outflow obstruction III. Inadequate system flow A. I and III B. I and II C. II and III D. I Which of the following initial flow settings would you select when setting up a CPAP flow-mask system for a patient with atelectasis? A. 2 times the patient's minute ventilation B. At least 6 to 10 liters per minute C. 4 times the patient's minute ventilation D. 10 times the patient's VT Which of the following mechanisms probably contribute to the beneficial effects of CPAP in treating atelectasis? I. Recruitment of collapsed alveoli II. Decreased work of breathing III. Improved distribution of ventilation IV. Increased efficiency of secretion removal A. I, II, and IV B. II and III C. I and IV D. I, II, III, and IV An alert and cooperative 28-year-old woman with no prior history of lung disease underwent cesarean section 16 hours ago. Her x-ray currently is clear. Which of the following approaches to preventing atelectasis would you recommend for this patient? A. IS B. PEEP therapy C. Deep breathing exercises D. IPPB therapy