Medical Diagnostic in Microbiology

Lecture Week 14
Reference for
Vaccines and Immunisations
• Schaechter chapters 45 and 55
• Schaechter chapter 32 for Polio vaccines. There is a table that compares live and killed vaccines .
• Brooks chapter 30 for viral vaccines (page
407-410)
• Brooks. Selected chapters with subheading
“Prevention and control by vaccines”: chapters
15, 16, 19,24,27,33,34,35,36, 37,39,40 and 42.
Medical Diagnostic in
Microbiology
Medical Microbiology SBM 2044
Diagnosing pathogens
• Why is this important?
• To guide the selection of appropriate therapy for the cause of an infection.
• Valuable information can be generated in four ways:
– Microscopic examination of patient samples
– Cultivation and identification of microorganisms from patient samples
– Measurement of a pathogen-specific immune response in the patient.
– Detection of pathogen-specific macromolecules in patient samples.
Assessing performance of laboratory tests
• No lab test is perfect
• Require skills to perform diagnostic techniques, as well as analysing and interpreting the results
• To describe the performance of value of all diagnostic tests:
– Sensitivity : the likelihood that it will be positive when the pathogen is present
– Specificity : the likelihood that it will be negative if the pathogen is not present
Diagnosing Infections by
Microscopy
• Based on:
– morphologic features
– staining properties
– movement
• Helminthic and protozoal infections are routinely diagnosed by microscopy.
• Fungal characteristic morphologic features
– e.g. Cryptococcus neoformans is an encapsulated yeast. Staining CSF with India ink, transparent capsule is visualised
FIGURE 48-4 India ink preparation of cerebrospinal fluid that shows many encapsulated yeast cells, some of which are budding, that are diagnostic of Cryptococcus neoformans meningitis.
Diagnosing Infections by
Microscopy
• Based on:
– morphologic features
– staining properties
– movement
• Helminthic and protozoal infections are routinely diagnosed by microscopy.
• Fungal characteristic morphologic features
– e.g. Cryptococcus neoformans is an encapsulated yeast. Staining CSF with India ink, transparent capsule is visualised
• Viruses – indirectly by the virus-induced changes in host cell morphology
A
Laboratory findings of
Cytomegalovirus
B. Immunohistochemical staining of infected cells
(arrow) in a renal biopsy specimen from a transplanted kidney in a patient with CMV infection.
A. Nuclear inclusions and cytoplasmic inclusions (arrows) in infected alveolar epithelium of an infant with congenital
CMV infection.
B
Stains
• When to stain culture for diagnosing?
• Provide info of presence of bacteria in a normally sterile body fluid
• Provide suggestive identification which allows for the empirical selection of antibiotics
• Confirmative diagnosis for certain clinical specimens
– G- diplococci inside the leukocytes of urethral pus
(always) gonococci
– Acid-fast bacteria in coughed sputum M. tuberculosis
• Stains:
– Gram stain, acid-fast, Giemsa, iodine and silver stains
Giemsa-stained blood smears from
Trypanosoma sp.
Antibody-based identification
FIGURE 58-2 The crossreactivity of three types of immunoglobulin preparations.
Cross-reactive
Common antibody-binding sites
(epitopes)
Specificity is enhanced by monoclonal antibody against an epitope on the antigen
Diagnosing infections by Culture
• The most specific way – identification of a particular pathogen in a patient sample
• However, is culturing practical for all microbes?
• Culturing media: agar and broth, in aerobic or anaerobic conditions
• Assumption: any organisms present in the specimen are causative and that the chemotherapy directed against them will be beneficial
• Open-ended vs. a specific pathogen
– Selective Thayer-Martin medium for gonococci, in nonsterile sites
• What factors might result in false positive cultures?
Blood culture
• Blood sample is inoculated into a nutrient broth turbidity
• Then subcultured on agar plates for species identification
• Lysis-centrifugation method lyse blood cells and pellets are removed and inoculated directly onto agar-based medium
More on culture techniques
• To determine phenotypic properties
– Motility, utilisation of various nutrient substrates, enzymes and toxin productions, byproducts of metabolism
– This would take days
• Antimicrobial sensitivity testing
– For therapeutic information
Antibody-based Techniques
• More rapid method
• Serological tests measure the patient’s humoral immune response to an infection, those directed at specific microbial antigens
• Other serology of infectious diseases are agglutination, complement fixation, and neutralization
• Solid-phase assays, where either the pathogen or antigens from the pathogen fixed to a solid support, and then the patient serum is added to the system.
Serology test
FIGURE 58-3 Direct ELISA serology for the detection of specific antibodies in patient serum.
Western blot
• Most specific serologic methods available
• Antigenic molecules from a pathogen are first separated according to their size using electrophoresis
• Immunoblotting (“ Western blot ”) whereby defined antigens are placed on strips of nitrocellulose paper.
• Following incubation, the strip is treated with an enzyme-labeled Ab. Addition of the substrate for the enzyme allows detection of Ag-specific bound Ab by colorimetric reaction.
• Useful for Abs in HIV infection and Lyme disease.
Antigens are then blotted
The blot is then incubated with the patient’s serum
•Antigenic molecules from a pathogen are first separated according to their size using electrophoresis
gp160 gp120 p55 gp41 p31 p24
Interpreting Western Blot
HIV proteins
Gp160 viral envelope precursor
( env ) gp120 viral envelope protein ( env ) binds to CD4 p24 viral core protein ( gag ) p31 Reverse transcriptase ( pol )
Band pattern Interpretation
Lane 1, HIV+ serum (positive control)
Lane 2, HIV- serum (negative control)
Lane A, Patient A
Lane B, Patient B
Lane C, Patient C
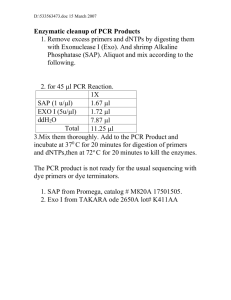
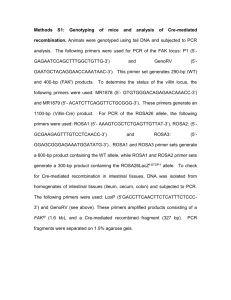
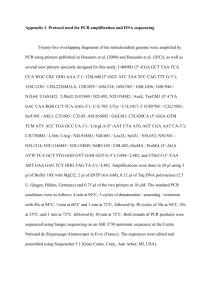
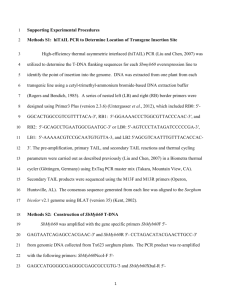
Diagnosing Infection by Detecting
Microbial Nucleic Acid
• To design a PCR, a specific sequence of microbial nuc acid must be known designing primers
• The PCR recipe:
• two primers
• deoxyribonucleotides dNTPs
• heat-stable DNA polymerase
• Temperature shifts between heating
(denaturation of DNA) and cooling (hybridization of the primers)
• The chain reaction results in a massive production of target DNA
PCR
Real-time PCR
•Amplicons (DNA amplified sequence) are quantified as they are generated using fluorescence label probe
•Intensity of fluorescence increases as the amplicons generated
•Useful in measuring viruses in human fluid samples
•e.g. HIV, CMV, EBV
Microarrays
• Bacterial culture allows microbiologist to detect a variety of pathogenic organisms in a single method.
• That is also the beauty of microchip…
• A microchip can be printed to contain hundreds of oligonucleotide probes
• Because bacteria have many conserved sequences, the design PCR primers will amplify a product (cDNA) from any bacterial species, but with different amplified sequences between the primers.
• Watch animation http://www.bio.davidson.edu/Courses/genomics/chip/chip
.html
• Play the Video game: http://learn.genetics.utah.edu/units/biotech/microarray/
1
Microarrays
2
3
4
1. PCR will amplify intervening sequences that are different in each species
2. During the amplification, the amplicons (cDNA) are labeled with a fluorescent dyeconjugated primer
3. Microarray has bound oligonucleotides (ssDNA) representing the intervening sequences from hundreds of bacterial species
Reference
• Schaechter chapter 58 or
• Brooks chapter 47