Suture Techniques in Primary Care
advertisement

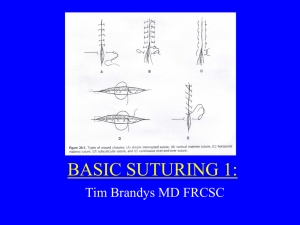
Suture Techniques in Primary Care Shawn A. Sutterlin, PA-C Watauga Orthopaedics Objectives • Review wound types and classification • Understand the principles of wound healing • Describe the 3 types of wound closure • Overview of Suture materials • Wound closure techniques Wound Classification • Four Classes • Clean • Clean-contaminated • Contaminated • Dirty/infected Clean Wounds • Most common is elective surgical incision • Primary closure • 1-5% rate of infection Clean Contaminated • Wounds contaminated by local flora despite aseptic technique • Cholecystectomy, appendectomy and hysterectomy • 3-11% infection rate Contaminated • Open traumatic wounds in nonsterile environment • Open fractures • Surgical procedures in which there is a gross deviation from sterile technique (emergent open cardiac massage) • 10-17% infection rate Dirty or Infected • Gross/heavy contamination or active infection • Perforated viscera, abscess and traumatic wounds • >27% infection rate Wound Healing • Four Stages • Hemostasis • Inflammatory • Proliferative • Remodeling Phase I: Hemostasis • Vasoconstriction stimulated by endothelial injury • Platelet aggregation • Coagulation cascade is activated and fibrin clot formed • Platelets release pro inflammatory mediators and PDGF in preparation for subsequent phases Hemostasis Phase II: Inflammatory • Inflammatory mediators released • Vasodilation - provides increased blood supply to injury site • Increase vascular permeability - allows plasma proteins, WBCs, into injured tissue • Migration of WBCs from circulation into interstitium and phagocytose debris/microbes Inflammation Phase III: Proliferative • Angiogenesis • Granulation • fibroblasts deposit extracellular matrix including collagen/elastin • Characteristic beefy red appearance Phase III: Proliferative • Epithelialization • keratinocytes • Contraction • Fibroblast release of actin Phase IV: Remodeling • Collagen remodeled along tension lines • Cells no longer needed are removed by apoptosis • May take many months Patient factors • • • • • • • Age Weight Nutrition Dehydration Blood supply Immunocompromised Chronic Disease Wound Closure • Primary closure • Secondary closure • Tertiary closure Primary Closure • Most common • Preferred method when appropriate • Wounds are re-approximated acutely • Dermis-dermis apposition • Best cosmetic outcome Secondary Closure • Known as healing by secondary intention • Wound edges are left un-approximated • Granulation tissue formed • Migration of keratinocytes provide reepithelialization over granulation tissue • Appropriate in wounds with soft tissue loss or severe contamination not closable by primary or tertiary means Tertiary Closure • Contaminated wound is I&D’d and left open for several days • Wound is then closed as in primary closure when risk of complications declines • Preferred method for high energy and highly contaminated wounds Suture Materials • Traits needed by suture • Tensile Strength • Knot security • Ease of handling • Low tissue reactivity Characteristics • Size • Tensile Strength • Monofiliment (nylon, prolene, monocryl) • Multifiliment (vicryl, ethibond, Silk) • Absorbable • Non Absorbable Characteristics • Dyed • Undyed • Sizes 11-0 to 6 Suture Sizing Absorbable • Broken down in tissues by hydrolysis, enzymes and inflammation • Time to resorb varies by material and diameter • includes vicryl, monocryl, PDS, gut. Non Absorbable • Not broken down by hydrolysis or inflammatory reaction • Walled off in body by fibroblasts or physically removed (skin sutures) • Includes nylon, prolene, stainless steel, silk, polyester (ethibond) Suture Size by Location Needles • Cutting - skin and other tough tissue • Taper - softer tissues inside body (bowel,vessels). Dilates tissues • Blunt - felt to pose less risk of needle sticks. Most useful in fascial closure. Before Closing • Hemostasis • Evaluate • Irrigate • Debride devitalized/contaminated tissues • Should it be closed primarily? Before Closing • Evaluate the wound • Time of injury • Size and shape of wound • Soft tissue loss • Gross contamination/foreign body Before Closing • Wound depth • Nerve, tendon, vascular involvement • Bone involvement (open Fx) • Uncontrolled hemorrhage Wound Preparation • Single most important step in preventing complications • • • • Control bleeding Remove all debris and devitalized tissue Irrigate copiously with NS Do not use iodine or hydrogen peroxide in the wound • • • • • • When to Consult Specialist Deep wounds to hands/feet, thorax, abdomen, or pelvis Full thickness lac to eyelids, lips or ears Lacerations which involve bone, joint, tendon, artery, muscle or nerve Markedly contaminated wounds Crush injuries Concerns about cosmesis When to Not Close • • • • • Active infection Erythema/induration Puncture wounds Human/animal bites Delayed onset of treatment • • 12 hours for body 24 hours for face Anesthesia • General/spinal Anesthesia • Used for large wounds and more invasive procedures • Regional Anesthesia • Lidocaine/bupivicaine infiltrated near peripheral nerve to produce anesthesia distally in extremity • Digital, wrist and ankle blocks most common Anesthesia • Local • Anesthetic agent infused directly into the tissues being treated • Most common method in outpatient setting Lidocaine • • • • • • Most common 1% should be adequate for most procedures Sodium channel blocker Rapid onset Relatively short duration of action Available with epinephrine • helps control bleeding Bupivicaine • Longer duration of action • Useful in prolonged procedures as well as post procedure pain control • Also available with epinephrine Local Anesthetics Caution!! • Do not use local anesthetic with epinephrine on structures with limited circulation • ears, nose, fingers, toes, penis Equipment • • • • • General Considerations Handle tissues as little as possible Limit the time and force used in retracting tissues Do not pinch tissues with forceps, Gently lift wound edges to place suture Irrigate frequently to minimize contaminants and maintain moist wound bed Approximate, don’t strangulate Needle Position Needle should be secured 1/2 - 2/3 down the length needle from the tip Always cross skin at 90 degree angle Rule of Halves • Allows better approximation of tissues • Avoids “dog ears” Rule of Halves 3 1 2 The Instrument Tie • How to tie a perfect square knot every time • • • • Place needle driver parallel to and directly over incision Always wrap needle end over driver toward tail When tightening each throw, move needle driver to opposite side of incision. The key is to always wrap OVER needle driver and to always alternate sides Basic Suture Methods • Simple interrupted • Simple running • locked running • Horizontal mattress • Vertical mattress • Running Subcuticular • Subcutaneous (buried knot) Simple Interrupted • Most common closure performed • Used in superficial wounds with minimal tension. • Nylon or prolene • Be careful of knot security Simple Interrupted Simple Continuous • Rapid • Best in short lacerations with no tension • Helps with hemostasis • If one knot fails, the entire closure is compromised • Contraindicated in infected tissues as infection can propagate along suture line Locked Continuous • Used in wounds closed with moderate tension • Helpful in obtaining hemostasis • Similar concerns with knot security and integrity of closure Horizontal Mattress • For fragile tissue • Distributes tension over wider area • Helps evert skin edges Horizontal Mattress Vertical Mattress • Used for maximal edge eversion • Minimizes deadspace in deeper tissues • Helps minimize tension Vertical Mattress Running Subcuticular • Provides optimum cosmetic results • Not for contaminated or infected wounds Running Subcuticular Subcutaneous • Buries the knot • Useful for minimizing deadspace in deeper wounds • Helps relieve tension on skin closure • May be used in dermis as well Subcutaneous After Closure • Apply antibiotic ointment • Non adherant sterile dressing • Splint if appropriate • Tetanus • Antibiotics • Schedule follow up 2-3 days Suture Removal • Face: 3-5 days • Scalp: 7 days • Chest and extremities: 8-10 days • Joints, palms, soles: 10-14 days