Physyiology of haemostasis system
advertisement

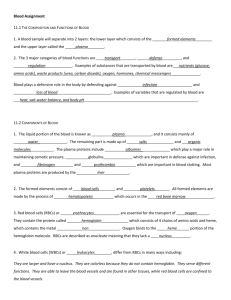
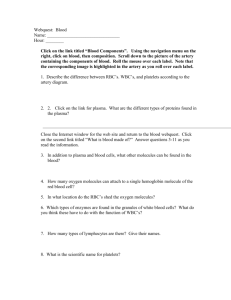
Physiology of haemostasis system Hemostasis system Hemostasis is very important for our life, because if we are live our hemostatic system is very strong. They are includes in a case of trauma, cutting the vessels etc. Hemostasis is the physiologic system, which support the blood in the fluid condition and prevent bloodless. Hemostasis system vital necessary and functionally connect with the cardiovascular, breathing, endocrine and other systems. The components of hemostasis The components of hemostasis are wall of the vessels, blood cells – platelets, erythrocytes, leucocytes, enzymes and nonenzymes components of plasma – clotting and anticlotting substances, fibrinolysis components of hemostasis. There are 2 kinds of hemostasis. They are vessel-platelets (primary) and coagulative (secondary) hemostasis. Primary hemostasis activity begin the first after the destroyed of vessels. Secondary hemostasis starts after that in case the primary hemostasis do not stopped the bloodless. Vessel-platelets hemostasis (or primary hemostasis include in clotting first of all after the destroyed the safe of vessel wall.) Properties and function of platelets Quantity of platelets is 180-320 G/L. Diameter of platelets is 1-4 micrometers, thickness – 0,5-0,75 micrometers. They are the little peace of megacariocytes cytoplasm (from one megacariocytes may develop few hundred of platelets). Platelets circulated in blood from 5 to 11 days and than destroyed in liver, lungs, spleen by the cells of macrophagal system. Function of platelets are: 1. hemostatic function – platelets produce substances, which are secure the hemostasis. 2. Angiotrophic function – provide trophic of endotheliocytes of vessel wall, support structure and functions of microvessels. These function is realize by adgesion of platelets to endotheliocytes and injection the enzymes into the endotheliocytes. For one day near 35 G/L platelets do this function. 3. Transport function – transfer the enzymes, ADP, serotonin and other. 4. Phagocytosis function – the contain of platelets help to kill viruses and antigens bodies. 5. Regeneratory function – platelets have the growth factor, which help to grow the endothelial and muscles cells which are present in the vessel wall. Stages of vessel-platelets hemostasis 1. Shorting spasm of the vessels – vascular spasm duration to 1 minute is caused by catecholamins and other enzymes. Diameter of vessels decrease on ½-⅓. Mechanism of it development determine by secretion of serotonin and thromboxan A2 from platelets and epinephrine from ending of sympathetic nerves. 2. Adgesion of platelets – activation of platelets and stick it to the place of defect in vessel wall. 3. Reverse aggregation of platelets – the thromb which are formed may make way for plasma. 4. Unreverse aggregation of platelets – the thromb which are formed can not may make way for plasma. 5. Retraction of platelets plug – decrease the size of plug, pack down the plug. Investigation of vessel-platelets hemostasis 1. Calculation of the platelets quantity 180-320 G/L. 2. Determination of duration of capillary bleeding after Duke’s method – to 3 minute in norm. 3. Sample of fragility of capillars – to 10 petechias in norm in a round with diameter 5 santimetres. Coagulative (secondary) hemostasis. Characteristics of clotting factors There are 12 clotting factors: I – fibrinogen; II – prothrombine; III – thromboplastin of tissue; IV – ions of calcium; V – proaccelerin; VII – proconvertin; VIII – antihemophylic factor A; IX – Christmas factor or antihemofilic factor B; X – Stuart-Prower factor or prothrombinase; XI – plasma thromboplastin antecedent; XII – Hageman factor; XIII – fibrin stabilizing factor. Some of them are enzymes – II, VII, IX, X, XI, XII,XIII; other are not – I, III, IV, V, VIII. The vitamin K is necessary for the functional activity of II, VII, IX, X factors. External mechanism of the first stage (3 factors from the injure tissues go to plasma and interactions with VII factor, the last is activated. VII active factor and IV factors form the complex 1a: III + VII active + IV, which is activated X factor.) Inner mechanism of the first stage (Factor 3 of platelets – platelets thromboplastine – influence on XII factor. Active XII factor + XI is complex 1. Active XI factor activated IX factor. Active IX factor + VIII factor + IV factor is complex 2. Complex 1a and 2 are activate X factor. Factor X active + V + IV formed complex 3 or thrombinasa complex.) Course of the second and third stages (The second stage – formation of thrombin from prothrombin. The third stage is formation of fibrin from fibrinogen. The last stage has 3 period; formation of fibrinmonomers; formation of fibrin S (solubilis); formation of fibrin I (insolubilis). Calcium is necessary for all stages.) Regulation of the clotting mechanisms Increase of clotting names hypercoagulation, decrease – hypocoagulation. Hypercoagulation may be in a stress cases. It depends on epinephrine, which concentration increased in the cases of stress. Epinephrine increase from the vessels walls factors from which produced prothrombinasa. In cases of big concentration epinephrine should activate XII factor in a bloodstream. It divides fats and fat acids, which have prothrombinase activity. After the hypercoagulation stage may be secondary hypocoagulation. Coagulogram Time of clotting by Ly-Wait – 5-10 minutes; time of plasma recalcification – 60-120 seconds; thrombotest – IV, V, VI degree; thromboplastin time – 12-15 seconds; thromboplastin index – 80-105 %; concentration of fibrinogen – 2-4 g/L; tolerancy of plasma to heparin – 6-11 minutes; heparin time – 50-60 seconds; fibrinolysis – 15-20 %. Anticoagulative mechanisms. Fibrinolysis. The tendency of blood to clot is balanced by a number of limiting reactions that tend to prevent clotting inside the blood vessels and to break down any clots that do form. The primary anticoagulants are antithrombin III (It is the most important anticoagulant in the blood); heparin (This substance was originally found in the liver, by large basophilic cells (mast cells) in tissues of various organs. Heparin reduces the ability of the blood to clot by blocking the change of prothrombin to thrombin. It can also be used to aid in reducing clots in cases in which internal clotting has already occurred. Heparin form complex with antithrombin-III. Activate nonenzyme fibrinolysis.); alpha-2-macroglobulin, alpha-1-antitripsin, protein C (Alpha2-macroglobulin is a similar to antithrombin-heparin cofactor in that it combines with the proteolytic coagulation factors. Its activity is not accelerated by heparin. Its function is mainly to act as a binding agent for the coagulation factors and prevent their proteolytic action until they can be destroyed in various ways. It a faint inhibitor of thrombin, connect with plasmin. Alpha-1-antitripsin inhibits thrombin activity, IXa, XIa, XIIa factors, plasmin and kallilrein. Protein C inhibits VIIIa, Va factors. It activity depend of thrombin and vitamin K concentration. Functionation of secondary anticlotting substances Primary anticoagulants are produce and present all time in plasma and secondary anticoagulants form in a case of blood clotting. They are antithrombin-I or fibrin and products of fibrinolysis or products of fibrinogen degradation. Fibrin is sorbs and inactivates thrombin and Xa factor. Products of fibrinolysis inactivate ending stage of clotting, IXa factor, platelets' agregation. THANK YOU!