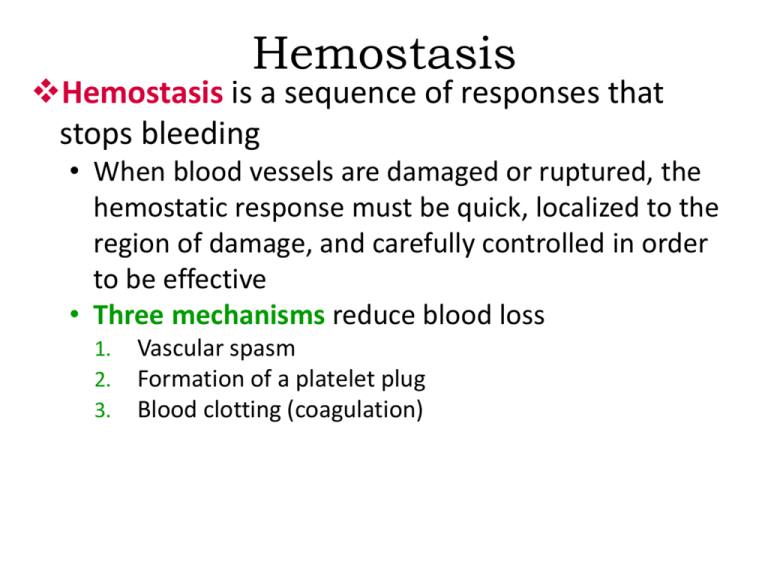
Hemostasis
Hemostasis is a sequence of responses that
stops bleeding
• When blood vessels are damaged or ruptured, the
hemostatic response must be quick, localized to the
region of damage, and carefully controlled in order
to be effective
• Three mechanisms reduce blood loss
1.
2.
3.
Vascular spasm
Formation of a platelet plug
Blood clotting (coagulation)
Hemostasis
1. Vascular spasm occurs as damaged blood vessels
constrict
2. Platelets adhere to damaged
endothelium to form a
platelet plug
Red blood cell
Platelet
Plug
Formation
Platelet
Collagen fibers
and damaged
endothelium
11 Platelet adhesion
Liberated ADP,
serotonin, and
thromboxane A2
22
Platelet release reaction
Platelet plug
33
Platelet aggregation
Hemostasis
3. Clotting (coagulation) is possible because of the
presence of several clotting proteins normally
dissolved (soluble) in the blood. Coagulation
occurs in a cascading fashion whereby one
activated clotting protein triggers the next step in
the process, which triggers the next, and so on once activated,
the soluble clotting factors
become insoluble
• There are 2 pathways to
activate the system
(a) Extrinsic pathway
Stages
of
Clotting
Tissue trauma
(b) Intrinsic pathway
Blood trauma
Damaged
endothelial cells
expose collagen
fibers
Tissue
factor
(TF)
Damaged
platelets
Activated XII
Activated
platelets
Ca2+
Ca2+
+
Platelet
phospholipids
Activated X Activated X
V
1
Ca2+
Ca2+
V +
PROTHROMBINASE
(c) Common
pathway
Ca2+
Prothrombin
(II)
THROMBIN
Ca2+
2
XIII
Fibrinogen
(I)
Activated XIII
Loose fibrin
threads
STRENGTHENED
FIBRIN THREADS
3
Hemostasis
The extrinsic pathway has few
steps and occurs rapidly, often
within seconds, once the
protein “tissue factor” (TF)
leaks into the blood
The intrinsic pathway is more
complex and occurs more
slowly in response to damage
to endothelial cells or
phospholipids released by
activated platelets
Hemostasis
Both the extrinsic and intrinsic clotting pathways
converge at a common point (pathway) where
factor X becomes activated (Xa)
• In this second stage of
blood clotting prothrombin
is converted to thrombin
which in turn converts
soluble fibrinogen to
insoluble fibrin threads
Hemostasis
The mineral Ca2+ plays an important role throughout the
clotting system, and many steps have positive or negative
feedback on various other steps to propagate the
process, yet maintain control
Clot retraction is the consolidation of the fibrin clot. As
the clot retracts, it pulls the edges of
the damaged vessel closer together,
decreasing the risk of further
damage – new endothelial cells can
then repair the vessel lining
Fibrinolysis
Because blood clotting involves amplification and
positive feedback cycles, a clot has a tendency to
enlarge, creating the potential for impairment of
blood flow through undamaged vessels
• The fibrinolytic system dissolves small, inappropriate
clots; it also dissolves clots at a site of damage once the
damage is repaired
both body tissues and blood contain substances that can
activate plasminogen to become plasmin, (the enzyme that
actively dissolves clots)
Intravascular Clotting
Blood clots sometimes form unexpectedly within
the cardiovascular system. Clotting in an
unbroken blood vessel (usually a vein) is called
thrombosis; the clot itself, called a thrombus
• Such clots may be initiated by roughened endothelial
surfaces of a blood vessel resulting from
atherosclerosis, trauma, or
infection
Intravascular Clotting
Intravascular clots may also form when blood
flows too slowly (stasis), allowing clotting factors
to accumulate locally and initiate the
coagulation cascade
Having an undamaged blood vessels with
smooth surfaces, good circulation, and nonsticky platelets are important factors that inhibit
thrombosis
• administration of anticoagulants and platelet
inhibiting drugs (aspirin-like drugs) can also hinder
thrombus formation or reverse a thrombus that has
formed
Intravascular Clotting
A thrombus may become dislodged and be swept
away in the blood. When a blood clot, air bubble,
piece of fat or other debris is transported
by the bloodstream, it is
called an embolus
•In the worst circumstances
(pulmonary embolism or
stroke), emboli can obstruct a
blood vessel and cause ischemia to
the tissue beds distal to the obstruction
Blood Components
Blood transfusion is the process of transferring
blood or blood products from one person to
another
Almost all donated blood in the U.S. is separated
into its various components to make better use
of it
• Whole blood is fractionated into units of packed red
blood cells (PRBCs), fresh frozen plasma (FFP),
platelets, and WBCs
• Albumin, coagulation factors, and antibodies can be
individually collected
Plasma vs. Serum
If the liquid part of blood is allowed to
coagulate it is called serum - serum is just plasma
without the clotting factors
•Serum is stable at room temperature
and can be stored on a shelf
it is also used for diagnostic testing because it won’t
coagulate in the machine
and mess it up!
Blood Groups
Red cells (and all cells in the body) have
proteins on their surface which act as antigens
or surface markers
• Even within the same species, the antigens of one
individual are not necessarily compatible with those
of another. For this reason, before donor blood cells
can be transfused to another person the major
surface antigens must be determined
the most significant of the 100 markers currently known
to exist on RBCs are the A and B antigens
Blood Groups
In transfusion medicine the presence or absence
of the
A and B red cell antigens forms the basis of the ABO
blood group system
Another major red cell antigen is the Rh antigen, which
85% of the population have, and comprises another
important blood grouping
Blood Groups
For reason that are not totally clear, serum
contains anti-ABO antibodies of a type opposite
to the ABO antigen on the red cell surface
• For instance, those with A antigens on their red cells
have anti-B antibodies in their serum
Blood Groups
By knowing the status of the A antigen, B antigen, and
Rh antigen, most of the major blood incompatibility
issues can be avoided
• Type AB individuals are “universal recipients”
because they has neither anti-A nor anti-B antibodies
in their serum that would destroy transfused RBCs
• Type O individuals are “universal donors” because
their RBCs have no antigens on the cell surface that
can potentially react with the recipients serum
Blood Groups
Blood typing for ABO
status is done using single
drops of blood mixed with
different antisera
• Agglutination with an
antisera indicates the
presence of that antigen on
the RBC
Rh Incompatibility
• Normally, blood plasma does not contain anti-Rh
antibodies; individuals whose RBCs have the Rh
antigen are said to be Rh+ while those who lack
the Rh antigen are Rh– Rh incompatibility can cause problems with any
blood transfusion, so it is screened just as carefully as the ABO
group
• perhaps the biggest problem with Rh incompatibility,
however, involves mother and child in pregnancy
Rh Incompatibility
If blood from an Rh+ fetus sensitizes an Rhmother during birth, anti-Rh antibodies will form
in the blood of that woman. During her next
pregnancy those antibodies can cross the
placenta to affect the next baby
• Hemolytic disease of the
newborn (HDN) results
when an Rh+ fetus
develops in the womb
of an Rh- woman
Rh Incompatibility
To prevent HDN, mothers who are Rh- are given
a injection of RhoGAM - a commercially
produced anti-Rh antibody – at various points
in her pregnancy
• The administered RhoGAM destroys any Rh+ cells
from the baby before the mother’s immune system
can become sensitized to them and produce her
own anti-Rh antibody. For this same reason,
RhoGAM is given to Rh- patients who have
abortions or miscarriages
Transfusion Reactions
In a blood transfusion, if the recipient receives
the wrong blood type, antigen-antibody
reactions will cause a rapid destruction
(hemolysis) of the donor red blood cells
• Giving the wrong type blood can cause the patient
to develop a fever, develop serious renal failure, or
go into shock. The most common cause is clerical
error (i.e. the wrong unit of blood being given to the
patient)
End of Chapter 19
Copyright 2012 John Wiley & Sons, Inc. All rights reserved.
Reproduction or translation of this work beyond that permitted
in section 117 of the 1976 United States Copyright Act without
express permission of the copyright owner is unlawful. Request
for further information should be addressed to the Permission
Department, John Wiley & Sons, Inc. The purchaser may make
back-up copies for his/her own use only and not for distribution
or resale. The Publisher assumes no responsibility for errors,
omissions, or damages caused by the use of these programs or
from the use of the information herein.