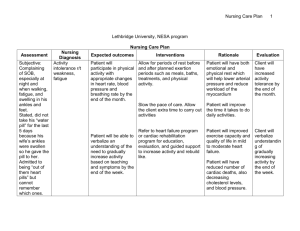
Manifestations of isotonic fluid volume deficit Acute weight loss
advertisement
Disorders of water and sodium balance Zhao Chenghai Pathophysiology Outline Introduction of water and sodium balance Edema Alterations in isotonic fluid volume • isotonic fluid volume deficit • isotonic fluid volume excess Alterations in sodium concentration • hyponatremia • hypernatremia Introduction of water and sodium balance Water and sodium balance Total fluid volume and distribution Body fluid composition Osmolality of the body fluid Water balance Mechanisms of regulation of body fluid and sodium balance Total fluid volume and distribution Total body fluid accounts for 60% of body mass in males. Total body fluid is mainly distributed in intracellular and extracellular compartments Intracellular fluid ( ICF) : 40% Extracellular fluid (ECF): 20% Interstitial fluid: 15% Plasma: 5% Body fluid composition The ICF is separated from the ECF by a selective cell membrane that is only permeable to a limited number of substances such as water, oxygen and carbon dioxide, but not to most of the electrolytes in the body. The concentration of ions in the interstitial fluid and plasma are considered to be equal except for protein. Osmolality of the body fluid The total osmolality is almost equal among plasma, the interstitial and intracellular fluids with a range from 280-310 mOsm/L, due to a free permeability of cell membrane to water. Nearly 80% of the osmolality of plasma and the interstitial fluid is induced by sodium and chloride ions. And approximately half of the intracellular osmolality is caused by potassium. Water balance Water intake • Ingestion in the form of liquid and water in food: 2100ml/day • Metabolism in the body following the oxidation of carbohydrates: 300ml/day Water output • Insensible evaporation from respiratory tract and through the skin: 700ml/day • Sweating: 100ml/day • Feces: small amount • Urine: 1500ml/day Mechanisms of regulation of body fluid and electrolyte balance Sensation of thirst Antidiuretic hormone (ADH) Renin-angiotensin-aldosterone system Atrial natriuretic peptide (ANP) ADH Main target sites: distal tubules and collecting ducts in kidney Function: to Promote the water reabsorption and cause increased ECF volume and decreased urinary output. Stimulating factors: • Blood pressure↓ • Plasma osmolality↑ • Blood volume ↓ Renin-angiotensin-aldosterone system Arterial pressure ↓ Plasma sodium content↓ Arterial pressure↑ Sympathetic nerve ↑ ECF volume ↑ Glomerulus (juxtaglomerular cells) Renal retention of sodium Increase potassium secretion renin Angiotensin I Angiotensin II Angiotensin converting enzyme Adrenal gland aldosterone ANP ANP is a hormone produced by specific cells of cardiac atrim in response to blood volume expansion. Function: ANP inhibits the reabsorption of sodium and water by the renal tubules, which in turn increases urinary excretion and helps to return blood volume back toward normal. ANP exerts a negative regulation against ADH in the central nervous system. Edema Definition of edema Edema can be defined as palpable swelling produced by expansion of the interstitial fluid volume. Edema is caused by excessive fluid in the interstitial compartment. Causes and pathogenesis of edema Increased capillary filtration pressure Decreased capillary colloidal osmotic pressure Increased capillary permeability Obstruction to lymph flow Increased capillary filtration pressure Increased vascular volume • heart failure • kidney disease • pregnancy Venous obstruction • liver disease with portal vein obstruction • venous thrombosis Decreased capillary colloidal osmotic pressure Increased loss of plasma proteins • protein-losing kidney diseases • extensive burns Decreased production of plasma proteins • liver disease • starvation • malnutrition Increased capillary permeability Inflammation Allergic reaction Malignancy Tissue injury and burns Obstruction to lymph flow Malignant obstruction of lymphatic structures Surgical removal of lymph nodes Manifestations of edema Life threatening in some locations, such as brain, larynx, lungs. Interfering with movement and limiting joint motion. Increasing the distance for diffusion of oxygen, nutrients and wastes at the tissue level. Treatment of edema Correcting or controlling the cause , and preventing tissue injury Diuretic therapy Elastic support stockings and sleeves for patients with lymphatic or venous obstruction Administering albumin intravenously to raise the colloidal osmotic pressure when edema is caused by hypoalbuminemia. Alterations in isotonic fluid volume Alterations in isotonic fluid volume Isotonic fluid volume disorders represent an expansion or contraction of the ECF brought about by proportionate changes in both sodium and water. Two types: • Isotonic fluid volume deficit • Isotonic fluid volume excess Isotonic fluid volume deficit Definition: Isotonic fluid volume deficit results when water and sodium are lost in isotonic proportions Causes: • Inadequate fluid intake • Excessive fluid losses Inadequate fluid intake Oral trauma or inability to swallow Inability to obtain fluids Impaired thirst sensation Therapeutic withholding of fluids Unconsciousness or inability to express thirst Excessive fluid losses Excessive gastrointestinal fluid losses vomiting, diarrhea, gastrointestinal suction Excessive renal losses diuretic therapy, osmotic diuresis, adrenal insufficiency Excessive skin losses fever, exposure to hot environment, burns and wounds that remove skin Third-space losses intestinal obstruction, edema, ascites Manifestations of isotonic fluid volume deficit Acute weight loss Compensatory increase in ADH Decreased extracellular fluid volume Shock Treatment of isotonic fluid volume deficit Treating the underlying causes Using isotonic electrolyte solutions for replacement. Isotonic fluid volume excess Definition: It represents an isotonic expansion of the extracellular fluid compartment. Water and sodium are increased in isotonic proportions. Causes: • Inadequate sodium and water elimination • Excessive sodium and water intake Inadequate sodium and water elimination Congestive heart failure Renal failure Hyperaldosteronism Liver failure Excessive sodium and water intake Excessive sodium intake Food, sodium containing medications or fluid Excessive fluid intake • ingestion of fluid in excess of output • administration of fluids or blood at an excessive rate Manifestations of isotonic fluid volume excess Acute weight gain Increased interstitial fluid volume Dependent and generalized edema Increased vascular volume Treatment of isotonic fluid volume excess Sodium-restricted diet Diuretic therapy is commonly used to increase sodium elimination. Alterations of sodium concentration Alterations of sodium concentration • Hyponatremia • Hypernatremia Hyponatremia • Definition Hyponatremia represents a decrease in plasma sodium concentration below 135 mmol/L. Causes of hyponatremia Excessive sodium losses and replacement with sodium-free water Excessive water intake in relation to output Excessive sodium losses and replacement with sodium-free water Exercise- or heat-induced sweating Gastrointestinal losses Renal losses (some chronic renal diseases) Excessive Water Intake in Relation to Output Excessive administration of sodiumfree solutions Repeated irrigation of body cavities with sodium-free solutions Irrigation of gastrointestinal tube with distilled water Kidney disorders that impair water elimination Increased ADH level Manifestations of hyponatremia Signs Related to Hypo-osmolality of Extracellular Fluids and Movement of Water Into Brain Cells and Neuromuscular Tissue Muscle cramps, Weakness, Headache, Depression, Personality changes, Lethargy and coma Gastrointestinal Manifestations Anorexia, nausea, vomiting, Abdominal cramps, diarrhea Treatment of hyponatremia water intoxication Limit water intake Administer diuretics sodium deficiency Administer saline solution orally or intravenously Hypernatremia • Definition Hypernatremia implies a plasma sodium level above 145 mmol/L. Causes of hypernatremia Excessive Water Losses Decreased Water Intake Excessive Sodium Intake Excessive water losses Watery diarrhea Excessive sweating Hyperventilation Decrease level of ADH Decreased Water Intake Unavailability of water Oral trauma or inability to swallow Impaired thirst sensation Withholding water for therapeutic reasons Unconsciousness or inability to express thirst Excessive Sodium Intake Rapid or excessive administration of sodium-containing solutions Manifestations of hypernatremia Thirst and signs of increased ADH levels Oliguria or anuria Intracellular dehydration – Dry skin and mucous membranes – tongue rough and fissured – decreased salivation Signs related to hyperosmolality of ECF and movement of water out of brain cells – Headache, agitation and restlessness, seizure and coma Treatment of hypernatremia Treating the underlying causes of the disorder Fluid replacement therapy to treat the accompanying dehydration. Today you learned: How to regulate the normal water and sodium balance? Definition, causes, manifestations and treatment of the following pathological conditions • • • • • Edema Isotonic fluid volume deficit Isotonic fluid volume excess Hyponatremia hypernatremia