Massive Hemorrhage
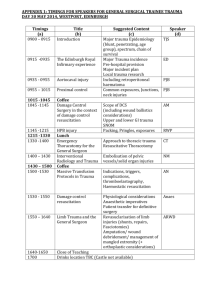
advertisement

Massive Haemorrhage Yolandi Ferreira Definitions • • • • Loss of entire blood volume equivalent within 24hrs Loss of 50% of blood volume within 3hrs Continuing blood loss of 150ml/min Continuing blood loss of 1.5ml/kg/min over 20 min • Rapid blood loss leading to decompensation and circulatory failure despite volume replacement and interventional treatment Lethal triad: Bloody vicious cycle Factors contributing to the Coagulopathy of Trauma Acidosis • Decrease coagulation factor activity thrombin generation platelet aggregation • Enhanced fibrinolysis via increased tPa and depletion of plasma activator inhibitor-1 Factors contributing to the Coagulopathy of Trauma Hypothermia • Platelet dysfunction • Reduced clotting factor activity Dilutional Coagulopathy • Factor deficiency • Thrombocytopenia • Anaemia Factors contributing to the Coagulopathy of Trauma Consumption of • Platelets • Fibrinogen • Clotting factors Crit Care Med 2008 Vol 36, No 7 (Suppl.) Prevent Coagulopathy The aim: Prevent the Coagulopathy • Most Rx arm of the lethal triad • Appropriate choices of resuscitation fluids • The amounts and ratio of these products to one another • The timing of delivery of these products • The use of adjuncts to resuscitation (recombinant Factor VIIa) So how do we do this • Current ATLS protocol • 1:3 Rule Replacement of each 1ml of blood lost with 3ml isotonic crystalloid Adult Hypotensive pt calls for a rapid infusion of 2L of an isotonic crystalloid solution Red cells are recommended for transient or initial non-responders • Time is of the essence Clarke et al found that the probability of death increases approximately 1% for each 3min spent in the emergency department in patients with major injuries isolated to the abdomen. J Trauma 2002;52:420-5 • Intra-osseous access, almost forgotten, has gained renewed attention in adults Permissive Hypotension • Allowing the BP of the patient who has the risk of major ongoing bleeding to not return to normal values, • But to stabilise at values around 75% of normal until surgical control of bleeding is established • Prevention of rebleeding syndrome Permissive Hypotension: When + When not Select +/- 3% of trauma population • Ruptured AAA • Bleeding DU/GU • Major vascular trauma to Non-compressible vessel • Ongoing Intra Abdominal Haemorrhage • Cold-coagulopathic-acidotic patient where temporising surgery is planned Contra-indications Use normal rules for Resuscitation: • • • • • • • Haemodinamically stable patient Prior to exclusion of Obstructive Shock Compressible bleed from isolated / external wounds Major head trauma Pregnant and childhood –no data yet Burns Possible crush syndrome / prolonged entrapment Criteria to achieve • • • • Perfusion not pressure Urine output Lactate < 5 mmol/l Rousable patient • Palpable radial pulse • SBP +/- 80mmHg Massive Transfusion • Many trauma centres have their own protocols: • i.) Massive blood loss with profound haemorrhage / hypovolemic shock • • Adult pts who require >10 U ii.) Continued bleeding after transfusion of 5 u in 4hrs / 10u in 24hrs Iii.) Prolonged PT, Depressed Fibrinogen => DIC • Intended to: Rapid restore blood volume Prevent coagulopathy • Operation Iraqi Freedom offered new evidence supporting a more balanced approach • PRBC/FFP/Platelet ratio 1:1:1 Borgman et al • Retrospective analysis in Iraq • Pt >10 units of PRBC within 24hrs Three groups: • 1:8 1:2.5 1:1.4 (plasma:PRBC) • 65% 34% 19% mortality Massive Transfusion What Rx is available Table 2. Resuscitation Fluids in both Clinical and Experimental Use • Isotonic crystalloids (lactate ringer) • Hypertonic saline solution (7.5% saline) • Artificial colloids (dextran, hydroxyethyl-starch) • Isotonic crystalloids with hydroxyethyl (Voluven®, • HAES-steril®, Hespan®, Hextend®) • Hypertonic saline solution with hydroxyethyl-starch • (HyperHES®) • Hypertonic saline solution with dextran (7.5% saline and 6% • dextran) • Isotonic crystalloids (lactate ringer) with pentoxifylline • Isotonic crystalloids with ethyl pyruvate • Hypertonic saline solution with pentoxifylline • Human colloids (plasma, albumin) • Fresh whole blood (FWB) • Packed red blood cells (PRBCs) • Artificial blood (hemoglobin-based oxygen carriers, • perfluorocarbons, Polyheme®) Fraga et al J Emerg Med 2009 Apr 1 Crystalloids / Colloids: • NO CONSENSUS • Ringers Lactate better than Normal Saline - based mainly on animal studies in 1960! • Colloids: Does NOT decrease ARDS - survival assessment studies grossly under powered - Some suggests even increased mortality Evidence • Cochrane Database Systemic Review • Perel et al concluded: ‘as colloids are not associated with an improvement in survival, and as they are more expensive than crystalloids, it is hard to see how their continued use in these patients can be justified outside the context of randomised clinical trails’ • Nolan concludes that as long as the appropriate volume is given, the type of fluid may not be of importance since anaemia is much better tolerated than hypovoleamia • Regarding bleeding: Colloids may interfere with coagulation more directly than crystalloids Hypertonic Saline • Improves haemodynamics • Rapidly corrects BP • Improves tissue perfusion • as drawing fluid from oedematous endothelium enhances mircocirculatory flow • Hypotensive patients with Penetrating injuries or Head injuries => IMPROVEMENT OF SURVIVAL with the use of hypertonic saline/dextran has been described • • Wade et al J Trauma 1997;42:S61-5 Wade et al J Trauma 2003;54:S144-8 Blood Component therapy Fresh Whole Blood • Key question driving current resuscitation research • ‘What is the optimal resuscitation fluid for a severely injured trauma patient?’ • Simplest answer: ‘Give the patient back the fresh whole blood that he lost’ Reality more complex • Modern experience with FWB is small Animal studies: • Restores myocardial function better than PRBC • Best 24hr hypotensive resuscitation fluid US Army survival benefit • Analysis is ongoing Problem: Cost Safety Mimic delivery of whole blood 1:1:1 Recombinant Factor VIIa (Novoseven) • • • • Topic of considerable debate Boffard et al SA based Prospective trial Reduction of blood transfusions with administration of Factor VIIa in BLUNT trauma patients • No effect on mortality Boffard, Riou, Warren et al J Trauma 2005; 59:8-15 May prolong the ‘golden hour’ of resuscitation rFVIIa enhances platelet thrombin generation rFVIIa • • • Considerable debate Timing Selection of patients • • Less effective in acidosis Remains effective in all but most severely hypothermic settings • • • Theoretical risk of thrombo-embolic events must be balanced against the more acute risk of exsanguination - Less than 0.05% of serious events in >480 000 doses given to pts with haemophilia - >1000 pts with haemophilia no statistically significant difference in events vs placebo group Current limitations: Storage 2’C - 8’C Short t1/2 High cost Require completion of ungoing trails Other Emerging Technologies Topical Sealants • Use in cases in which conventional measures of bleeding control fail • Local application of concentrated clotting factors • Fibrin in WW II for spinal and cranial injuries • Floseal –relatively new agent • Combination of bovine gelatine granules mixed with a human thrombin solution • No randomized studies have been performed HemCon • Shellfish derivative (chitosan) • Causes Ionic attraction of red cells to stick to tissue + over injured vessels • Issued to UK soldiers 1:4 • Highly effective • Now in thinner dressings –easier to push in • Shelf-life 2yrs QuikClot • Volcanic rock • Acts as a sponge, rapidly absorbing fluid to produce coagulation and a stable blood clot in the wound • It is chemically inert and is not absorbed into the body • Safe to stay in the wound as long as needed • Produces heat- can create burns • Manufacturers: Powder: Effective and less heat • Included in US Marine first aid kits and more limited basis by US Army in Iraq and Afghanistan • Shelf life +/- millennium! Anti-fibrinolytics • Potential to reduce blood loss • Aprotinin, Tranexamic acid, Epsilon aminocaproic acid • Aprotinin suspended by FDA 2007 as result of reports of increased mortality in CABG • Increased renal and vascular complications and death • No evidence to support the prophylactic or empiric use of anti-fibrinolytics • Major ongoing international trail CRASH-2 Artificial Hb-based O2 carriers • Artificial Blood acts as O2 bridge • Two classesof Hb substitutes: Modified Hb - Hemopure Perfluorocarbons • Red cell membranes are removed from out-dated red cells • Hb molecules are cross-linked to prolong shelf-life • Phase III testing of Hemopure and Polyheme Artificial blood Advantages • Immediate availability • No need for x-match • O2 carrying capacity • Storage at room temperature • Reduced risk of infectious, immunological and metabolic complications Disadvantages • Short half life 24 – 48 hrs • Interference with laboratory measures • Lack of knowledge about toxicity The Mission • For civilian providers the casualty is the mission • For the military medic, the mission must often continue despite casualties • Warfare has historically resulted in significant advances in surgery and medicine • Iraq and Afghanistan is no exception Military Medicine: • • • • • • • Rapid Identification, Rapid transfer Massive transfusion: Recommend Ratio 1:1:1 Use of FWB advantages Minimization of Crystalloid infusion rFVIIa and other adjuncts Hypothermia: Aggressive prevention and treatment <C>ABC in Battlefield ATLS References: • • • • • • • • • An approach to transfusion and hemmorrhage in trauma: current prospectives on restrictive transfusion strategies. Tien H et al Can J Surg. 2007 Jun;50(3):202-9 Prehospital advances in management of severe penetrating trauma. Robert Mabray Crit Care Med 2008 Jul;36(7 Suppl)S258-66 Exsanguination in trauma: A review of diagnostic and treatment options Geeraedts et al Injury 2009 Jan;40(1):11-20 Epub 2009 Jan 8 The cellular basis of traumatic bleeding Hoffman M. Mil Med. 2004 Dec;196(12Suppl):5-7,4 Monitoring of Hemostasis in combat trauma patients Carr ME Jr. Mil Med. 2004 Dec;169(12 Suppl):11-5,4 Massive transfusion and nonsurgical hemostatic agents Perkins JG et al Crit Care Med 2008 Jul;36(7 Suppl):S325-39 Warm fresh whole blood transfusion for severe hemorrhage Spinella PC Crit Care Med 2008 Jul;36(7 Suppl):S340-5 Damage control resuscitation: a sensible approach to the exsanguinating surgical patient Beekley AC Crit Care Med 2008 Jul;36(7 Suppl):S267-74 Are we giving enough coagulation factors during major trauma resuscitation? Ho AM et al. Am J Surg. 2005 Sep;190(3):479-84 References: • • • • Transfusion practice in military trauma. Hess JR Transfus Med. 2008 Jun;18(3):143-50 Are we giving enough coagulation factors during major trauma resuscitation? Anthony M Am J of Surg 2005 190:479-484 Transfusion of Blood Products in trauma: an update Fraga J of Emerg Med 2009.02.034 Effect of recombinant factor VIIa as an adjunctive therapy in damage control Fox et al J Trauma 2009 Apr; 66(4 Suppl):S112-9 Talks: Prof / Colonel Tim Hodgets <C>ABC Emergency Medicine in the developing world, Cape Town 2007 Tim Hardcastle Fluids in Pre-hospital cases Emergency Medicine in the developing world, Cape Town 2007