20 - UTI-341 Final
advertisement

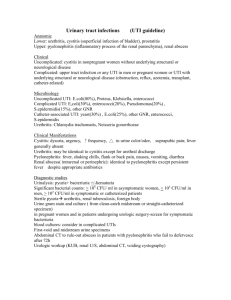
URINARY TRACT INFECTIONS by Dr FARAZ AZIM NIAZ Consultant Nephrologist MRCP(UK), SSC-Nephro(KSA) King Khalid University Hospital, Riyadh Epidemiology of UTI Worldwide, 150 million cases / year 90 % cystitis, 10 % pyelonephritis 75 % sporadic 25 % recurrent 2% complicated Prevalence of urinary tract infections (UTI) almost half of all women will have at least one UTI in their lives. the risk of UTI in women increases after menopause after a UTI: 20 - 40 % will have a recurrence recurring infections are usually reinfections. asymptomatic bacteriuria in women ↑with age & occurs in 2.7% of 15 - 24 year olds 9.3% of over 65 year olds 20 - 50% of over 80 year olds Prevalence of UTIs 2 UTI is rare in young and middle-aged men & often with catheterisation or urological procedures. bacteriuria in elderly men occurs in 10% of those living at home, 20% of those living in nursing homes & 30% of those who are in hospitals urinary catheter increases the risk almost ten-fold in hospitalised patients and those in other care homes. pyelonephritis is common in patients who have been catheterised for over a month. Gender and sexual contact Infant and children : Male >> female Adolescent-menopause : Female >> male Older age : Female = = male Women: Short ureter Sexual contact : colonization of pathogens in bladder Spermicidal : Change of normal flora Men (<50) : Prostate infection, anatomical defects , Lack of circumcision, homosexuals Symptomatic Infection Asymptomatic bacteriuria Classification of UTIs Classification by Type of UTI Asymptomatic bacteriuria Cystitis Upper / Lower UTi Pyelonephritis Symptoms Symptomatic Asymptomatic Recurrence Sporadic < 1 UTI / 6 m Recurrent 1 UTI / 6m Complicating factors Uncomplicated Complicated Urinary Tract Infection- Types urethritis cystitis prostatitis Lower pyelonephritis intrarenal & perinephric abscess Upper UTI- types by complicating factor Uncomplicated UTi: infection in a structurally and neurologically normal urinary tract Complicated UTI: infection in tract with functional or structural abnormalities Complicated or Un-Complicated UTI Uncomplicated UTI is the one occurring in a healthy young nonpregnant woman, & a Complicated UTI is the one occurring in anyone else. vs Pathophysiology Host protective factors inUTI Flushing mechanism of micturition Acid pH of urine (4.6- 6) anti-bacterial Acid vaginal pH (3.5-4.5)) suppresses colonization Urinary Tamm-Horsefall protein (secreted by ascending loop of Henle) & blocks E. coli Chemotactic factors - interleukin-8 Immune responses in UTI Submucosal IgA-producing plasma cells in bacterial cystitis IgM & IgG antibodies produced against bacterial antigens Protective role of antibodies unclear, may limit damage within the kidney & prevent persistent colonization & thus recurrence of infection Host Factors Complicating Bacteriuria Facilitate bacteriuria Residual bladder urine after voiding Turbulent urethral flow(stricture) Foreign bodies Atrophic vaginal mucosa Vesico-ureteral reflux Worse prognosis of UTIs Childhood pyelonephritis Diabetic nephropathy Malignant hypertension Chronic pyelonephritis Bacterial virulence factors in UTI Escherichia coli strains expressing O-antigens cause high proportion of infections Capsular antigens of E. coli associated with clinical severity (antiphagocytic) P-fimbriae enhance attachment of E. coli) to uroepithelial cells Motile bacteria ascend the ureter against urine flow Bacterial virulence factors in UTI Bacterial urease (Proteus) splits urea →NH4 ion alkalinizes urine with loss of acid pH → stone formation → obstruction & survivial of bacteria within stones resisting eradication Gram-negative endotoxin decreases ureteral peristalsis Hemolysin damages renal tubular epithelium & promotes invasive infection Aerobactin of E. coli promote iron accumulation for bacterial replication Pathogenesis of UTI Ascending route most common Colonization of urethra and peri-urethral tissue is the initial event More in women than men due to short female urethra ,so urethral organisms enter bladder during micturition & in close proximity to perianal areas Once in the bladder , multiply, then pass up the ureters (esp. if vesico-ureteral reflux) to the renal pelvis & parenchyma Hospital infection associated with lower urinary tract instrumentation (catheterization, cystoscopy) Pathogenesis of UTI- blood borne Hematogenous seeding less frequent than ascending infection Kidney a common site of abscess formation in Staphylococcus aureus bacteremia, less often in candidemia, rarely with gram-negative bacteremia Hematogenous seeding of kidney also occurs with Salmonella (typhoid) and Mycobacterium tuberculosis Source of uropathogens: enteric bacteria Pathogenesis of UTIs: Risk Factors ↓resistance of mucous membranes (e.g. in menopause) sexual intercourse disturbances in ureteral functioning in children the re-entering of urine back into the ureters (vesicoureteral reflux), Uterine prolapse Diabetes Pathogenesis of UTIs - 2 Predisposing Conditions- contd benign prostatic hypertrophy any illness, eg diabetes, affecting the emptying -Neurogenic Bladder spinal injury →disturbances in bladder emptying or urinary catheter) Stones catheterisation & other urological procedures Renal Transplantation Terminology of UTI Cystitis: localized infection of the bladder Prostatitis: localized infection of the prostate = lower UTI Pyelonephritis: infection of the kidney with acute inflammation of the pelvis, medullary and cortical tubules, & intersititum = upper UTI Urosepsis: bacteremia ( in blood) due to pyelonephritis Perinephric abscess: associated with obstruction of an infected kidney with abscess formation in the peri-nephric space due to extension of infection across the renal capsule Clinical Symptoms of UTI Types of UTI Typical Symptoms & Signs Cystitis Frequent voiding, suprapubic pain Burning micturition Hematuria, cloudy urine Pyelonephritis Fever chills, flank pains, N/Vomiting Cystitis Sx Urosepsis Fever- chills Shock Urethritis ? Acute dysuria, frequency Suspect sexually transmitted pathogens, no hematuria, no suprapubic pain, new sexual partner, cervicitis Cystitis Symptoms: frequency, dysuria, urgency, suprapubic pain Cloudy, malodorous urine (nonspecific) Leukocyte esterase positive = pyuria Nitrite positive (but not always) WBC (2-5 with sx) and bacteria on urine microscopy Cystitis Acute Pyelonephritis Pyelonephritis Fever, chills Nausea/Vomiting, diarrhea, tachycardia, Costo-vertebral angleTenderness or deep abdominal tenderness Leukocytosis Urine microscopy: Pyuria + WBC casts, bacteria & hematuria Possibly signs of Gram negative sepsis ? Pyelonephritis Complications: sepsis, papillary necrosis, abscess, ureteral obstruction ↓renal function if scarring, in pregnancy – ↑incidence of preterm labor Diagnosis of UTI History Physical exam Lab parameters: Urinalysis with microscopy for WBC, bacteria Urine culture with sensitivities Diagnose acute uncomplicated cystitis in women based on Hx, PE, and UA alone, no need for culture to treat Diagnosis Urinalysis Leukocyte-esterase positive. = pyuria Nitrite positive from urease producing bacteria eg proteus (but not always) Microscopy – WBC ( > 5 in pt with symptoms) -- Bacteria Diagnosis algorithm Symptomatic patient Uncomplicated cystitis in a woman, no risk factors not a relapse Yes No No Bacterial culture, "on the spot" testing to confirm diagnosis Typical symptoms, < 2 infections / year, patient familiar with her illness Yes Start treatment based on results Antibiotic therapy Dipstick Methods pH, Sp.Gravity, protein, glucose, blood, ketone, Leukocyste esterase + Pyuria Nitrite + Gram(-) bacteriuria except pseudomonas FACTS NITRITE: Screening test for bacteria in urine Gm –ve bact convert urine nitrate to nitrite False –ve: enterococcus, ascorbate, urine <4 hrs LEUCOCYTE – ESTERASE by granulocytes Test threshold is 5 – 15 WBC/HPF False –ve in : glycosuria, high sp. Gravity, cephalexin, tetracyclin, ↑oxalates, vaginal debris Microscopic Examination Pyuria: WBC > 5 / HPF in spun urine Bacteriuria > 105 cfu/ml Diagnosis of UTI Urinalysis : Leukocyte esterase : On Dipstick exam Nitrate nitrite : On Dipstick exam gram negative bacteria except pseudomonas • Pyuria : > 5 WBC /HPF, WBC cast Bacteriuria : > 105 cfu/ml Collecting a sample in adults, mid stream urine (MSU) sample usually reliably represents the urine in the bladder. samples from urinary bags or bedpans should not be used as they invariably will be contaminated the most reliable sample is obtained via a suprapubic puncture urine in bladder >4 hours (any shorter time will increase the risk of false negative findings) Diagnosis- interpretation Urine culture 105 colonies per mL considered standard for diagnosis - but misses up to 50% Now, 103 to 104 accepted as significant if patient symptomatic if several bacterial strains are grown on culture; contamination of the sample is the likely cause Sensitivities for better tailoring of therapy Significant bacteriuria Clinical status or methods of sampling Significant concentration (microbes / ml) MSU; symptomatic patient or urine in bladder <4 h >103 MSU; urine in bladder >4 h >104-5 Male patient, catheter specimen sample >103 Female patient, catheter specimen sample >104 Asymptomatic bacteriuria >105 Suprapubic puncture sample any growth Asymptomatic bacteriuria microbiological diagnosis Positive Urine culture repeatedly (105 cfu/ml) in the absence of signs of UTI pyuria does not affect interpretation Investige & treat asymptomatic bacteriuria → only in pregnant women Its prevalence varies from 1-5% to 100% in selected population groups. . Causative agents of UTIs Escherichia coli most common 80% of community - acquired 50% of hospital-acquired Others: enterococci Staphylococcus saprophyticus and klebsiella pseudomonas and proteus are more rare % of Organisms in UTI % of types of Organisms in UTI Localization of UTI No definite standard method Ultrasonography IVP Abdominal CT / MRI Tc-99m DMSA renal scan A B C D CT images at different levels –> hypodense areas of ?pyelonehritis T1 MRI- hypointense area T2 MRI- hyperintense area Axial MRI- hyperintense area MRI – Fluid (abscess) in lower pole Emphysematous Pyelonehritis: (a) CT – air in wall of U.B (b) Plain X ray- mottling in UB (A gas forming infection of renal parenchyma & perinephric tissues ) Xanthogranulomatous Pyelonephritis Enlarged cystic areas + a stone in the pelvis Tc-99m DMSA Renal Scan DDx Scar Renal infarction ↓Renal cortical uptake Indentation at upper pole Sterile Pyuria- causes Pyuria in the absence of bacterial infection Recent UTI treated with antibiotics Glucocorticoid therapy Acute febrile episode Cyclophosphamide Pregnancy Renal transplant rejection Genitourinary tract trauma Prostatitis and cystourethritis Renal T.B. Therapy in UTIs - 1 Acute uncomplicated cystitis: in women patient with typical symptoms, not belonging to any of the risk groups, is treated without laboratory investigations if the symptoms are atypical, a strip test urinalysis may be carried out to support diagnosis if the strip test is negative, the urine should be cultured and other reasons for the symptoms should be considered Treatments of UTI - options Lower UTI (Cystitis) : in women 3-7 days course of antibiotics ( short is preferable) •Trimethoprin/SMX = 1st choice •Cephalosporines ( Cefpodoxime)/ Nitrofurantoin •Fluoroquinolone ( ciprofloxacin, Norfloxacin etc) Lower UTI (Cystitis) : in men Longer course for 7 days •TMP/SMX • Flouroquinolones •B-lactams( Augmentin) or Nitrofurantoin: not recommended If no improvement→ consider Prostatis ORAL Treatment of pyelonephritisUncomplicated pyelonephritis: Mild to moderate pts can be treated orally as outpatient with either a quinolone ( ciprofloxacin or levofloxacin) sulpha-trimethoprim for Duration : 7-14 days course of antibiotics B- lactams, Nitrofurantoin: not favoured If Amoxil: then give for 14 days. Inpatient management is appropriate in the following : 1. 2. 3. 4. Severe illness with high fevers, pain, and marked debility Pt unable to maintain oral hydration or take oral medications Pregnancy Concerns about patient compliance Oral drugs Treatment of pyelonephritis-Complicated ie :progression to renal corticomedullary abscess, perinephric abscess, emphysematous pyelonephritis, or papillary necrosis Consider underlying anatomic or functional abnormalities An unwell patient should be admitted to hospital Parentral treatment is commenced with either Cephalosporines i.v. ( ceftriaxone ) or fluoroquinolone orally/ I.V & change to oral, when response is obvious Note: Antibiotics alone may not be successful unless underlying conditions are corrected I.V Drugs Prevention of UTI Recurrent UTI Women with > 3 episodes of UTI per year Avoidance of spermicidal or diaphragm frequent and complete voiding Immediate voiding after sexual contact Good hydration Antibiotics after sexual contact Low dose antibiotics prophylaxis Prophylaxis of recurrent UTI with antimicrobial agents prophylaxis should be considered when more than 3 infections per year or 2 in 6 months prophylaxis to continue for 6 months if infections recur after prophylactic treatment, the prophylaxis is recommenced for 6 – 12 months (D) Pregnancy and UTI Incidence of UTI in pregnant women: 2-8 % 20-30 % of pregnant women with asymptomatic bacteriuria : Upper UTI (pyelonephritis) in 2nd-3rd trimester b/c Ureteral dilatation, reflux Effects ofUTI in pregnancy : Increased incidence of fetal death and growth retardation UTI in Pregnancy - TREATMENT Flouroqinolones are CONTRA-INDICATED •Low urinary tract infection : 7 day course antibiotics Ampicillin, cephalosporine Pyelonephritis: 2-4 weeks course antibiotics Cephalosporins, extended spectrum penicillins Parenteral treatment Thereafter, follow-up urine culture, monthly Asymptimatic bacteriuria Antibiotics Tx & f/u Treatment during pregnancy asymptomatic bacteriuria & cystitis are treated in the same way Requires longer tx of 7-14 days Cephalosporin, nitrofurantoin, augmentin, sulfonamides (do not use near term b/c risk of kernicterus single-dose treatment is not recommended due to foetal risk fluoroquinolones should be avoided during the whole of pregnancy, and sulphatrimethoprim during the latter part of pregnancy Treatment of UTI in diabetics Cystitis in diabetics drugs of choice for initial treatment are same as for uncomplicated UTI antibiotic treatment must always be based on the results of urine culture treatment to continue for 7 days Acute pyelonephritis in diabetics treatment is the same as for uncomplicated pyelonephritis consider urological imaging earlier than normal, if there is no response to appropriately chosen medication the causative agents of recurrent UTI’s in diabetics are often unusual, resistant microbes (species of pseudomonas, enterococci and enterobacter) and various candida species. Treatment of Complicated UTI Catheter - related Ampicillin/gentamycin or Tazocyn or ticaricillin/clav or imipenem or meropenem x 2-3 weeks Switch to PO FQ or TMP/SMX when possible Rule out obstruction Watch out for enterococci and pseudomonas UTI in CHILDREN- Needs prompt recognition & treatment Symptoms, non-specific,so difficult to distinguish between upper & lower, however, in < 2 yrs old child History of UTI Temperature >40ºC most helpful Suprapubic tenderness Lack of circumcision UTI in CHILDREN- in verbal children Abdominal pain Back pain Dysuria, frequency, or both New onset urinary incontinence SAMPLING of Urine – difficult ( catheter, suprapubic) Diagnosis: in usual ways. Therapy : Dose of AB as per Weight UTIs in men a UTI in men can be associated with either acute or chronic bacterial prostatitis prostatitis or epididymitis may play a part particularly in febrile UTI it is advisable to palpate both the prostate and scrotum chronic bacterial prostatitis, or at least the retention of bacteria in the prostatic ducts, should be suspected in relapses with the same causative bacteria UTIs in men 2 Afebrile lower urinary tract infection in men: if the infection is not associated with urinary stricture or prostatitis,it is treated with the same drugs as cystitis in women, but the treatment should continue for 7 - 10 days nitrofurantoin should not be used in men as adequate prostatic concentrations are not achieved (D) Febrile urinary tract infection in men is treated with a long course of antibiotics with good prostatic and epididymal penetration first choice: a fluoroquinolone for 2 weeks UTIs in men 3 UTI in men associated with acute bacterial prostatitis treatment for 4 - 6 weeks (depending how quickly patient responds to treatment) to be followed up with low dose prophylaxis with e.g. trimethoprim or nitrofurantoin Chronic bacterial prostatitis recurrent UTI’s and calcifications in prostate oral quinolones for 2 – 3 months (D) to be followed up with prophylactic medication Lower UTIs in children treatment principles are the same as for adults little evidence to support short term treatment in children (C) drugs of choice nitrofurantoin 5 mg/kg/day or trimethoprim 8 mg/kg/day treatment to continue for 5 days (C) Probable lower UTI with generalised symptoms in children treated so that any possible infection of the kidney is also covered, i.e. with antibiotics with high tissue penetrability oral medication acceptable drugs of choice sulphatrimethoprim (trimethoprim 8 mg/kg/day) cefalexin 30 - 50 mg/kg/day in 3 divided doses cefuroxime axetil 20 mg/kg/day in 2 divided doses or mecillinam 20 - 40 mg/kg/day in 3 divided doses treatment to continue for 7 days (C) Treatment of pyelonephritis in children all infants with febrile UTI should be admitted to hospital drugs of choice cefuroxime (100 mg/kg/day in 3 divided doses) or ceftriaxone (80 mg/kg/day daily) intravenous therapy until obvious response when obvious response to treatment is observed, medication is changed over to oral until the total course of treatment, i.e. 10 days, is completed follow-up treatment according to culture and sensitivity results, with an antibiotic with good tissue penetrability (e.g. sulphatrimethoprim or a cephalosporin) Treatment ? Uncomp. cystitis with less than 48 hours of sx, non-pregnant, usu. 3 days tx sufficient Bactrim DS, Septra DS Cipro or other FQ (avoid in preg.) Nitrofurantoin (7 days) Augmentin Bladder analgesis, Pyridium Asymptomatic Bacteriuria ? 105 org/mL growth Empiric treatment of all asymptomatic bacteriuria (ASB) in pregnancy. Screening at first visit. ASB if untreated = inc. PTD and LBW, 20-30% develop pyelo. Do TOC in 2 weeks and each trimester. Screen Sickle cell trait each trimester. Twofold inc. risk of ASB Asymptomatic Bacteriuria Treatment failures: repeat tx based on sensitivities for 1 week, then prophylactic therapy for remainder of pregnancy Prophylaxis: Nitrofurantoin, Ampicillin, TMP/SMX Treatment of Pyelonephritis -Outpatient Uncomp. Nonpreg pyelo Primary – any FQ x 7 days, cipro Alt. -- Augmentin, TMP/SMX, or oral CSP for 14 days Treatment of Pyelonephritis – Inpatient ? Treat IV until patient is afebrile 24-48 hours. Then, complete 2 week course with PO meds Use FQ or amp/gent or ceftriaxone or piperacillin If no improvement on IV, consider imaging studies to look for abscess or obstruction All pregnant patients with pyelo get inpatient tx, appropriate IV antibiotics immediately Predisposing conditions Neurogenic bladder: dysfunction or bladder diverticulum (incomplete emptying) Age - Postmenopausal women with uterine or bladder prolapse (incomplete emptying), lack of estrogen, decreased normal flora, concomitant medical conditions such as DM Vesicoureteral reflux Bacterial virulence Genetics Change in urine nutrients, DM, gout Predisposing conditions to UTI Female Short urethra, proximity to anus, termination beneath labia Sexual activity Pregnancy 2-3% have UTI in preg, 20-30% with asx bacteriuria may lead to pyelonephritis Increased risk of pyelo = decreased ureteral tone, decreased ureteral peristalsis, temp. incomp of vesicoureteral valves Symptoms of UTIs 1 Cystitis: typical symptoms include frequency and burning sensation when passing urine. Pyelonephritis: only some patients have difficulties in micturition temperature (> 38oC) and flank or back pain nausea in the elderly or sudden collapse in health status (”off-legs”) Symptoms of UTIs 2 incontinence or offensive urine in the elderly should not be considered as UTI as such; even though they may be indicative signs of an infection almost any signs of infection in infants may be indicative of a UTI (C) in a small child a temperature alone, without any other signs of an infection, should raise a suspicion of a UTI UTI in children and the elderly may manifest itself as incontinence or retention. Complicated UTIs are those occurring in… Men Children Pregnancy People with suspected pyelonephritis People with recurrent UTI Failed antibiotic treatment or persistent symptoms Catheterised patients Hospital-acquired infections Recent urinary tract instrumentation People with abnormalities of genitourinary tract People with renal impairment and People with impaired host defences Catheter-Associated UTI 10-15% of hosp. pts with catheter develop bacteriuria Risk of infection is 3-5% per day of catheterization UTI after one-time bladder cath approx. 2% Gram neg. bacteremia- most significant complication Greater antimicrobial resistance Urine Culture Study Significant bacteriuria Midstream clean technique: 105 CFU/ml Suprapubic puncture, catheter collected urine: 102 CFU/ml Women with symptomatic cystitis Pyuria +102 CFU/ ml Symptomatic pyelonephritis patients Pyuria +104 CFU/ml Diagnosis of UTIs 1 No need to do any urinalysis, if a female patient, who does not belong to any of the risk groups, clearly has occasional cystitis based on her symptoms Urine microscopy is not usually necessary to diagnose cystitis Diagnosis of UTIs 2 Bacterial culture of urine should be carried out in all cases, except in uncomplicated cystitis, even though the results will not be available when medication is commenced (B) In early pregnancy bacterial culture should be carried out in all pregnant women if only to diagnose asymptomatic bacteriuria (A) In adult febrile infections with generalised symptoms, and in children’s infections, C-reactive protein (CRP) concentration above 40 mg/l is suggestive of a kidney infection (C) Interpretation of Urine Cultures: General Guidelines A single species of Enterobacteriaceae recovered at >105 cfu’s/mL urine: with patients symptomatic for urinary tract infection, 95% probability of true bacteriuria A single species of Enterobacteriaceae recovered at 104-105 cfu’s/mL urine: with patients symptomatic for urinary tract infection, 33% probability of true bacteriuira Gram-positive, fungal, and fastidious uropathogens often present in lower numbers (104-105 cfu’s/mL urine) Urethral commensals recovered at <104 cfu’s/mL urine Commensal Microflora of the Urethra Coagulase-negative staphylococci (except S. saprophyticus) Viridans and non-hemolytic streptococci Lactobacilli Diphtheroids (Corynebacterium except C. urealyticum) Saprophytic Neisseria Anaerobic bacteria Common Bacterial Contaminants Staphylococcus epidermidis Corynebacteria(diphtheroids) Lactobacillus Gardnerella vaginalis Anaerobic bacteria Urine culture is not helpful for women with uncomplicated lower urinary tract infections as it does not improve outcomes. In women with classical presentation of uncomplicated UTI, treatment can begin based on the strength of clinical presentation. In women with dysuria and vaginal symptoms consider both a UTI and STIs. A dipstick positive to nitrites or leukocytes has a probability of a UTI of about 80% A dipstick negative to both nitrites and leukocytes, has a probability of a UTI of about 20%. Contents When is urine culture helpful? Urine culture should be performed for: 1. Women with a UTI with complicating features 2. All pregnant women 3. Men with suspected UTI 4. Suspected acute pyelonephritis 5. Prostatitis Contents Complicating features in women include: • Abnormal urinary tract e.g. stone, reflux, catheter, • Impaired host defences e.g. pregnancy, diabetes, immunosupression, • Impaired renal function, • Suspicion of pyelonephritis, • More than three UTIs in one year, or • UTI recurrence within two weeks. Contents Urine culture is recommended for pregnant women Women with asymptomatic bacteriuria in early pregnancy have a 20-30 fold increased risk of developing pyelonephritis, premature delivery and low birth weight infants. All pregnant women should be screened for asymptomatic bacteriuria at 12-16 weeks gestation. If bacteriuria is detected by screening, the patient should be treated and a urine culture performed monthly throughout the pregnancy Contents Urine culture is indicated for lower UTI in Men All UTIs in men are considered complicated, therefore a urine culture is indicated, even if the urine dipstick is negative. Contents A urine culture is indicated when acute pyelonephritis is suspected Dipstick testing of the urine may be useful if clinical findings are equivocal Antibiotics should be commenced while waiting for culture results Post-treatment urine cultures are recommended one to two weeks after antibiotic therapy Contents Screening for asymptomatic bacteriuria Screening for asymptomatic bacteriuria is not in: recommended 1. Non pregnant women 2. Elderly people 3. People with indwelling urinary catheter. 4. People with spinal cord injuries. The prevalence of asymptomatic bacteriuria varies from 1-5% to 100% in selected population groups. Asymptomatic bacteriuria is a microbiological diagnosis based on the isolation of a specified count of bacteria in the absence of signs of UTI. Contents Causative Microbes of APN-I Microorganism No(%) E.Coli 191 (88) Klebsiella pneumoniae 8 (3.7) Staphylococcus species 8 (3.7) Enterococcus species 7 (3.2) Acinetobacter iwoffii 1 (0.5) Enterobacter aerogenes 1 (0.5) Xanthomonas maltophilia 1 (0.5) 민 등, 대한신장학회지 1998 Microorganisms in Urine(OPD) Microorganisms Escherichia coli Enterococcus faecalis Klebsiella pneumoniae ssp Enterococcus faecium Staphylococcus aureus Pseudomonas aeruginosa Proteus mirabilis Enterobacter cloacae Klebsiella oxytoca % 51 13 6 3 3 3 2 2 1 CNUH, 2003 Antibiotics Sensitivity for E. Coli Antibiotics Ampicillin Trimethoprim/Sulpha Cefazolin Amikacin Imipenam Ciprofloxacin Gentamycine No(%) 27.3 43.9 82.0 98.3 98.4 76.1 79.8 이 등, 대한신장학회지 2002 Single-dose therapy single-dose therapy is slightly less effective than conventional therapy effective in infections caused by E. coli, but less so in S. saprophyticus infections recommended particularly when practical reasons warrant its use (e.g. self-care) Preparations: phosphomycin 3 g norfloxacin 800 mg ciprofloxacin 500 - 750 mg ofloxacin 200 mg as a single dose Antimicrobial therapy in UTIs 2 Reserve drugs: Quinolones (norfloxacin, ofloxacin or ciprofloxacin) for 3 days if first choice drugs are not suitable or if the infection has not responded to first choice drugs or recurrent infection within 4 weeks if there is a relapse, urine must be cultured and the treatment should be continued for 7 days In special cases: cefalexin or cefadroxil for 5 days (if the above are contraindicated) sulphatrimethoprim for 3 days (particularly if the level of infection is unclear) amoxicillin for 5 days (particularly in enterococcal infections) Treatment of Recurrent uncomplicated UTI 3 or more episodes in one year, 2 in 6 months Bactrim DS ( or septra DS) QD for 3-6 months - once infection eradicated, self-admin.,Single dose at symptom onset or one DS tab post-coitus Measures for prevention: voiding after intercourse, good hydration, frequent and complete voiding Underlying Conditions Diseases Percents(%) Diabetes mellitus 56 (49.6) Urinary tract stone 22 (19.5) Congenital anomaly 7(6.2) Renal cyst 6(5.3) Pregnancy 5(4.4) Neurogenic bladder 5(4.4) Vesico-Ureteral reflux 4(3.5) 민 등, 대한신장학회지, 1998 Drugs of choice in UTI prophylaxis First choice: trimethoprim 100 mg in the evenings nitrofurantoin 50 - 75 mg in the evenings Second choice: methenamine hippurate 1 g twice daily norfloxacin 200 mg daily or on 3 evenings per week nitrofurantoin (not if serum creatinine is above 150 μmol/l) quinolones (in cases where there is no response with other prophylactic medication or tolerance to other medications is poor) During pregnancy: nitrofurantoin 50 mg daily or methenamine hippurate 1 g daily for the rest of the pregnancy particularly if recurrent bacteriuria is diagnosed in early pregnancy Un-Complicated or complicated UTI ‘Uncomplicated’ UTI are occasional lower UTI in women with no predisposing factors ‘Complicated’ infections are all other UTIs including lower UTIs in men Children pregnant women catheter-induced infections UTI - also categorized into Non-catheter associated (community- acquired) Catheter associated (hospital- acquired) Any category may be symptomatic or asymtomatic Causative organisms of AcutePyelonephritis Microorganism No (%) E.Coli 122 (91.7) Enterococcus spp 4 (3.0) Pseudomonas spp 2 (1.5) S. viridans 2 (1.5) Proteus 1 (0.8) Coag.N.Staph 2 (1.5) Not isolated 113 이 등, 대한신장학회지 2002 Microorganisms in Urine (ER) Microorganisms Escherichia coli Enterococcus faecalis Klebsiella pneumoniae ssp Alcaligenes xylosoxidans Burkholderia cepacia Staphylococcus aureus Proteus mirabilis Enterococcus faecium Enterobacter cloacae % 51 9 7 5 5 3 3 3 2 CNUH, 2003 Xanthogranulomatous Pyelonephritis Mass-like lesion of Ch.PN b/c obstruction due to infected renal stones