Surveillance definitions CDC NHSN Manual
advertisement

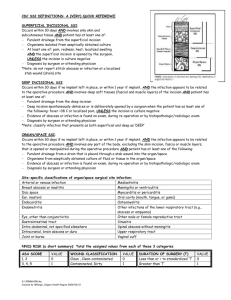
Surveillance definitions of CLABSI, VAP, SSI and CAUTI: A summary of definition criteria in the CDC NHSN Manual CDC National Healthcare Safety Network Before reporting an HAI (healthcare-associated infection), it must satisfy the specific criteria It is very important to use the criteria consistently to achieve accuracy of reporting of infections Use clinical, laboratory, pharmacy, radiology and other diagnostic information as well as patient charts and notes DO NOT USE LABORATORY RESULTS ALONE! (as these may indicate colonization only) Physician’s diagnosis alone, in absence of other available criteria, is acceptable except for pneumonia HAI ( Healthcare-associated Infection) A localized or systemic condition resulting from adverse reaction to the presence of an infectious agent/s or its toxin/s There must be no evidence that the infection was present or incubating at the time of admission The source of the infection may be endogenous or exogenous Infections in infants that result from the passage through the birth canal are HAI’s Infections that are NOT HAI Complications or extensions of infections already present on admission, UNLESS a change of pathogen or symptoms strongly suggests the acquisition of a new infection ( a new event) Infections in infants that are acquired trans-placentally, eg. rubella, CMV, syphilis, AND become evident < 48 hours after birth. Re-activation of a latent infection eg. Herpes zoster (shingles), herpes simplex, syphilis, TB Conditions that are NOT infections Colonizations: presence of microbes but no adverse clinical signs and symptoms eg. positive Microscopy on urine report Inflammation in response to tissue injury or chemicals & other non-infectious agents CLABSI Event Primary bloodstream infections that are associated with the presence of a central line (or umbilical catheter in neonates) at the time of or within 48 hours before the onset of the event (infection) There is no minimum time that the line must be in place before the event LCBI (Laboratory-confirmed bloodstream infection) or CSEP( clinical sepsis) in <1 year-olds Location of attribution ( where the event became evident) and transfer rule( exception) – see details in NHSN Manual. What is a central line? An intravascular catheter that terminates at or close to the heart or in one of the great vessels (aorta, pulmonary artery, superior & inferior vena cava, brachio-cephalic veins, internal jugular veins, subclavian veins, external iliac veins and common femoral veins) Neonates: umbilical artery or vein Must be a lumened device through which fluids are infused, pushed or withdrawn. May be temporary or permanent (e.g. dialysis tunneled or implanted catheters, including ports) LCBI – must meet 1 of 3 criteria Criterion 1 and 2 apply for all ages, including babies Criterion 1: Pt has a RECOGNIZED pathogen cultured from 1/more blood cultures AND the organism in the blood is NOT related to an infection at another site Recognized pathogens: S. aureus, Enterococcus spp, E.coli, Pseudomonas spp, Candida spp. What if it is a common skin contaminant? (Coagulase negative staphylococci, diptheroids, Bacillus spp, viridans group streptococci, Propionibacterium spp, Micrococcus & Aerococcus spp) It must have been identified in 2 or more blood cultures Drawn on separate occasions ( but within 2 days of each other) AND Patient must have symptoms AND not related to other site. LCBI – must meet 1 of 3 criteria Criterion 1 and 2 apply for all ages, including babies Criterion 2: Patient has at least 1 of the following S/S: fever ( >38 for adults: 38 rectal or tympanic, 37 oral or 36 axilliary for babies ), chills, or hypotension AND S/S and pos lab results are not related to infection at another site AND common skin contaminant cultured from 2 or more blood cultures drawn at different times LCBI (Laboratory confirmed bloodstream infection) Positive catheter tip cultures alone DO NOT indicate a BSI (bloodstream infection) Purulent phlebitis with positive culture of catheter tip and NO or negative blood culture is reported as CVS-VASC, not a BSI Only report as a primary BSI if there is no other site of infection. Secondary BSI’s are associated with an infection at another site with the same antibiogram CSEP ( Clinical sepsis in babies) Criterion 3: Patient under 1 year of age has at least one of the following clinical S/S with no other recognized cause: Fever ( >38 rectal), hypothermia ( <37 rectal), apnea, or bradycardia AND Blood culture not done or no organisms detected AND No apparent infection at another site AND Physician commences treatment for sepsis Temperature: 38 rectal/tympanic/temporal artery = 37 oral = 36 axillary 37 rectal/tympanic/temporal artery = 36 oral = 35 axillary VAP (Ventilator Associated Pneumonia) event Diagnosed on radiological, clinical and laboratory criteria Report PNEU’s that are ventilator-associated if the patient was intubated and ventilated at the time of surveillance, OR within 48 hours before the onset of the event, including the weaning period There is no minimum period of time the ventilator must be in place in order for the PNEU to be considered VAP Location of attribution: Where patient was on the date PNEU was identified (eg. Operating room cannot be allocated) Pt extubated and discharged from hospital A. Admitted hospital B next day with PNEU. = VAP for hospital A Transfer rule for internal transfers: if VAP develops within 48 hours of transfer, it is attributed to the transferring location Physician’s diagnosis ALONE is NOT acceptable, except in outbreaks of respiratory syncitial virus, influenza or adenovirus Definition of a ventilator A device to assist or control respiration continuously, Through a tracheostomy or By endotracheal intubation Lung expansion devices like: Intermittent positive pressure breathing ( IPPB) or Nasal positive end-expiratory pressure ( PEEP) or Continuous nasal pos airway pressure ( CPAP or hypoCPAP) Are not considered ventilators UNLESS Delivered via tracheostomy or endotracheal intubation (e.g. ET- CPAP) When it is not PNEU When clinical status changes are due to: Myocardial infarction, pulmonary embolism, RDS, atalectasis, malignancy, COAD, hyaline membrane disease, bronchopulmonary dysplasia, etc. Intubated patients with tracheal colonization or URTI (eg. tracheo-bronchitis) rather than early onset PNEU Patients with tracheitis, tracheo-bronchitis, or bronchiolitis without pneumonia are reported as BRON Patients with lung abscess or empyema without pneumonia are reported as LUNG When patient is elderly, an infant, or immunocompromised, typical S/S of pneumonia may be masked – see algorithms Interpret sputum samples carefully – may be contaminated with airway colonizers, eg. Candida (However Gram stain can be an important clue) Nosocomial pneumonia Characterised by onset: Early onset: occurs within the first 4 days of hospitalization Moraxella catarrhalis, H. influenzae, S. pneumoniae including MRSA Viruses can cause early and late onset Yeasts, fungi, legionellae and Pneumocystis carinii usually cause late onset Pneumonia due to gross aspiration is considered nosocomial if it meets any specific criteria and was not present at admission Multiple episodes of pneumonia may occur in critically ill patients with long ICU stays. Late onset: often caused by gram negative bacteria and S. aureus, If the episode resolved and a new episode occurred, it is a new event. Change in pathogen alone is NOT indicative of a new event – there must be new S/S and radiographic evidence. Refer NHSN Manual for Algorithms:P18–21 and footnotes P21 – 22 and flow diagrams: P 23 - 24 Footnotes to algorithms for VAP The diagnosis of HAI PNEU in non-ventilated patients is not always easy. Pulmonary or cardiac disease will cloud the clinical picture, eg. Pulmonary oedema from CCF may simulate S/S of pneumonia Thus serial X-rays are necessary to confirm the diagnosis. Look at X-rays 3 days prior to the diagnosis and on days 2 and 7 after the diagnosis Pneumonia may have a rapid onset and progression, but it does not resolve quickly. Radiographic changes persist for weeks If X-rays confirm rapid resolution, then it is probably NOT a pneumonia, but a non-infectious process like atalectasis or CCF Footnotes to algorithms for VAP X-ray terminology that may indicate PNEU: Purulent sputum: Air-space disease; focal opacification; patchy areas of increased density Secretions from lungs / bronchi / trachea that contain > 25 neutrophils and <10 squamous epithelial cells per low power field ( x100) A single notation of purulent sputum or change in character of sputum is not meaningful – changes must be documented over a 24 hour period before they can be seen as indicative of the onset of disease Patients with pneumonia due to viruses & mycoplasma will have scant or watery sputum ( or sometimes muco-purulent), few S/S, changes will only be seen on X-rays. Infants with RSV or influenza may produce copious sputum Patients with pneumonia due to Legionella spp, mycoplasma or viruses: few bacteria seen on gram stain Footnotes to algorithms for VAP Tachypnoea: Adults: > 25 breaths per minute Prems : > 75 breaths/min Under 2 months old: > 60 breaths / min 2-12 months: > 50 breaths / min Children > 1 year old: > 30 breaths / min “Rales” = crackles An endo-tracheal aspirate is NOT a minimally contaminated specimen, therefore, it does NOT meet the laboratory criteria Semi-quantitative or non-quantitative cultures of sputum obtained by deep cough, induction, aspiration, or lavage are acceptable Footnotes to algorithms for VAP Immunocompromised patients include: Neutropaenia (absolute neutrophil count Leukaemia Lymphoma HIV with CD 4 count < 200 Splenectomy Early post-transplant Cytotoxic chemotherapy High dose steroids < 500/cubic mm) Algorithms for VAP PNU 1: an algorithm used for clinically defined pneumonia PNU 2: Table 5: Pneumonia with common bacterial or filamentous fungal pathogens and specific laboratory findings Table 6: Pneumonia with viral, Legionella, Chlamydia, Mycoplasma and other uncommon pathogens and specific laboratory findings PNU 3: Pneumonia in immunocompromised patients CAUTI event Catheter-associated UTI’s are classified into 2 groups: SUTI and ASB. ( excludes OUTI) Report UTI’s that are catheter-associated if the patient had an in-dwelling catheter at the time or within 7 days before the onset of the event There is no minimum time the catheter must be in situ in order for the UTI to considered catheter-associated Location of attribution and transfer rule as per VAP Definition of an in-dwelling catheter A drainage tube That is inserted into the urinary bladder Through the urethra Is left in place And is connected to a closed drainage system Does NOT include straight in-and-out catheters SUTI (Symptomatic Urinary Tract Infection) Must meet at least 1 of the following: Criterion 1: Patient has at least 1 of the following S/S with no other recognized cause: fever > 38, urgency, frequency, dysuria, or suprapubic tenderness and Patient has positive urine culture, i.e. > 100,000 microorganisms per ml of urine with no more than 2 species of microorganism SUTI (Symptomatic Urinary Tract Infection) Criterion 2: Patient has at least 2 of the following S/S with no other recognized cause: fever>38, urgency, frequency, dysuria, or suprapubic tenderness and at least 1 of the following: positive dipstick for leukocyte esterase &/or nitrate pyuria ( > 10 wbc/cubic mm) organisms seen on gram stain of unspun urine at least 2 urine cultures with repeated isolation of same uropathogen ( G negative bacteria or S. saprophyticus) with >100 cfu/ml in non-voided specimens < 100 000cfu/ml of a single uropathogen in a patient on antibiotics for UTI Physician diagnosis of UTI Physician commences specific therapy for UTI SUTI (Symptomatic Urinary Tract Infection) Criterion 3: Patient under 1 year has at least one of the following S/S with no other recognized cause: fever ( >38 rectal), hypothermia ( <37 rectal), apnea, bradycardia, dysuria, lethargy, or vomiting and Patient has positive urine culture, >100 000 cfu/ml with no more than 2 species of microorganisms SUTI (Symptomatic Urinary Tract Infection) Criterion 4: Patient < 1 year has at least one of the following with no other recognized cause: fever > 38 rectal, hypothermia < 37 rectal, apnea, bradycardia, dysuria, lethargy, or vomiting and At least one of the following: Positive dipstick for leukocytes &/or nitrate Pyuria ( > 10 wbc/ cubic mm) Organisms seen on gram stain of unspun urine At least 2 cultures with repeated isolation of the same uropathogen with > 100 cfu/ml in non-voided specimens < 100 000 cfu/ml of a single uro-pathogen in a patient on specific UTI antibiotics Physician diagnosis or physician commences specific UTI therapy Comments on UTI A culture of a urinary catheter tip is NOT an acceptable laboratory test to diagnose UTI Urine cultures must be obtained appropriately: clean catch or catheterization In infants, a urine culture should be obtained by bladder catheterization or suprapubic aspiration; a bag culture is NOT reliable. ASB : Asymptomatic Bacteriuria Patient has had an indwelling catheter within 7 days before the culture AND patient has positive urine culture; > 100 000 organisms per ml with no more than 2 species AND patient has no fever, urgency, dysuria, suprapubic tenderness SSI (Surgical Site Infection) Event Definition of an operation: takes place in an operating room during a single trip to the OR( operating room) where the surgeon makes at least one incision through the skin or mucous membrane, including laparoscopy and closes the incision before the pt leaves the operating room An OR includes an operating room, C-section room, interventional radiology room, cardiac cath lab An implant includes any non-human foreign body that is permanently placed in a patient, including screws, mesh, wires that are left permanently. Superficial incisional SSI Infection occurs within 30 days after the operation AND involves only skin and subcutaneous tissue of the incision AND patient has at least one of the following: Purulent drainage Report organisms isolated from wound swabs as follows: ( Prof Duse criteria) if mono-microbial growth ( one organism) if a Strep. pyogenes ( beta haemolytic Strep Group A) isolated if 2 organisms, must be known wound pathogens in a quantity 2+ or more if > 2 organisms, report only the one associated with predominant growth, provided that pus cells were seen on microscopy if 3 or more organisms, do not report unless found on a repeat specimen or wound aspirate At least one of the following: pain / tenderness, localized swelling, redness/ heat and the incision is deliberately opened by surgeon and is culture pos or not cultured. If culture neg, it does not meet this criterion. Diagnosis of superficial SSI by surgeon There are 2 types: SIP (primary incision) . Patient has more than 1 incision for the operation, eg. Chest incision for CABG SIS (secondary incision) eg. Donor site incision on leg or arm for CABG Reporting instructions for SSI Do not report a stitch abscess Do not report a localized stab wound infection as SSI – it is reported as skin or soft tissue Cellulitis, by itself, does not meet the criteria for SSI Infected circumcision site is reported as CIRC Infected burn wound is reported as BURN and not SSI If incisional site infection extends into fascial or muscle layers, report as deep ( DIP / DIS) Deep Incisional SSI Infection occurs within 30 days if no implant or Within 1 year if implant is placed and infection is related to the operative procedure AND Involves deep soft tissues ( fascia / muscle) AND Patient has at least ONE of the following: Purulent drainage from deep incision, but not organ / space Deep incision spontaneously dehisces or Is opened by surgeon and Is culture-pos or not cultured when the pt has at least one of the following S/S: Fever>38, localized pain/tenderness ( A culture-negative finding does not meet this criterion) An abscess or other evidence of infection found by direct exam / x-rays / histopathologic exam Diagnosis by a surgeon 2 Types: DIP (primary incision), and DIS ( secondary incision) Organ / space SSI Involves any part of the body ( including skin incision, fascia, muscle layer) that is opened and manipulated during an operative procedure Specific additional sites are assigned to organ/space SSI’s to identify the location e.g. Appendectomy with sub-diaphragmatic abscess = SSI – IAB (intra-abdominal specific site) SSI - BONE ( Table on P 37, NHSN Manual) Organ / space SSI Infection occurs within 30 days after the operation if no implant and within 1 year if implant is placed & infection is related to operative procedure AND Infection involves any part of the body, excluding skin incision, fascia, muscle) that is opened or manipulated during the operation AND Patient has at least one of the following: Purulent drainage from a drain placed through a stab wound into the organ / space Organisms obtained from aseptically obtained culture of fluid or tissue in the organ / space Abscess found on direct examination or x-rays or histopathology examination Diagnosis by surgeon or physician