CDC SSI DEFINITIONS for LS2 2006
advertisement
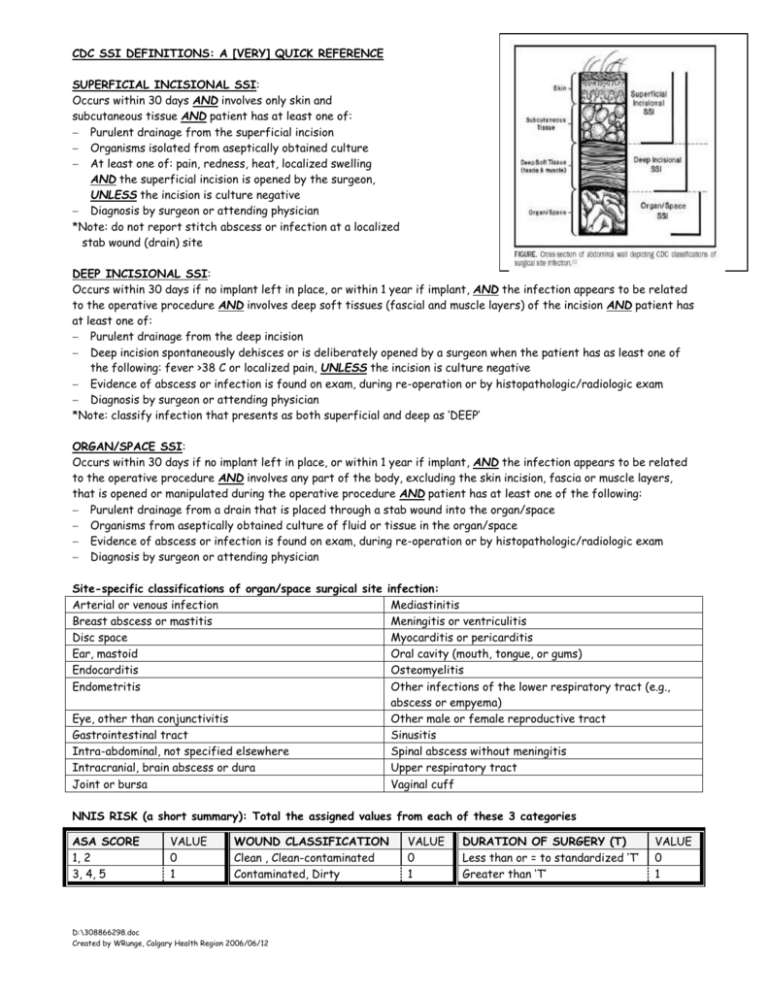
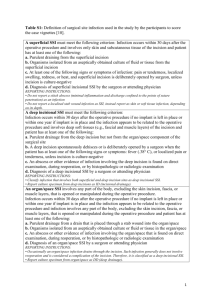
CDC SSI DEFINITIONS: A [VERY] QUICK REFERENCE SUPERFICIAL INCISIONAL SSI: Occurs within 30 days AND involves only skin and subcutaneous tissue AND patient has at least one of: Purulent drainage from the superficial incision Organisms isolated from aseptically obtained culture At least one of: pain, redness, heat, localized swelling AND the superficial incision is opened by the surgeon, UNLESS the incision is culture negative Diagnosis by surgeon or attending physician *Note: do not report stitch abscess or infection at a localized stab wound (drain) site DEEP INCISIONAL SSI: Occurs within 30 days if no implant left in place, or within 1 year if implant, AND the infection appears to be related to the operative procedure AND involves deep soft tissues (fascial and muscle layers) of the incision AND patient has at least one of: Purulent drainage from the deep incision Deep incision spontaneously dehisces or is deliberately opened by a surgeon when the patient has as least one of the following: fever >38 C or localized pain, UNLESS the incision is culture negative Evidence of abscess or infection is found on exam, during re-operation or by histopathologic/radiologic exam Diagnosis by surgeon or attending physician *Note: classify infection that presents as both superficial and deep as ‘DEEP’ ORGAN/SPACE SSI: Occurs within 30 days if no implant left in place, or within 1 year if implant, AND the infection appears to be related to the operative procedure AND involves any part of the body, excluding the skin incision, fascia or muscle layers, that is opened or manipulated during the operative procedure AND patient has at least one of the following: Purulent drainage from a drain that is placed through a stab wound into the organ/space Organisms from aseptically obtained culture of fluid or tissue in the organ/space Evidence of abscess or infection is found on exam, during re-operation or by histopathologic/radiologic exam Diagnosis by surgeon or attending physician Site-specific classifications of organ/space surgical site infection: Arterial or venous infection Mediastinitis Breast abscess or mastitis Meningitis or ventriculitis Disc space Myocarditis or pericarditis Ear, mastoid Oral cavity (mouth, tongue, or gums) Endocarditis Osteomyelitis Endometritis Other infections of the lower respiratory tract (e.g., abscess or empyema) Eye, other than conjunctivitis Other male or female reproductive tract Gastrointestinal tract Sinusitis Intra-abdominal, not specified elsewhere Spinal abscess without meningitis Intracranial, brain abscess or dura Upper respiratory tract Joint or bursa Vaginal cuff NNIS RISK (a short summary): Total the assigned values from each of these 3 categories ASA SCORE 1, 2 3, 4, 5 VALUE 0 1 WOUND CLASSIFICATION Clean , Clean-contaminated Contaminated, Dirty D:\308866298.doc Created by WRunge, Calgary Health Region 2006/06/12 VALUE 0 1 DURATION OF SURGERY (T) Less than or = to standardized ‘T’ Greater than ‘T’ VALUE 0 1