Metabolic acidosis_02 (ΔAnion gap)
advertisement
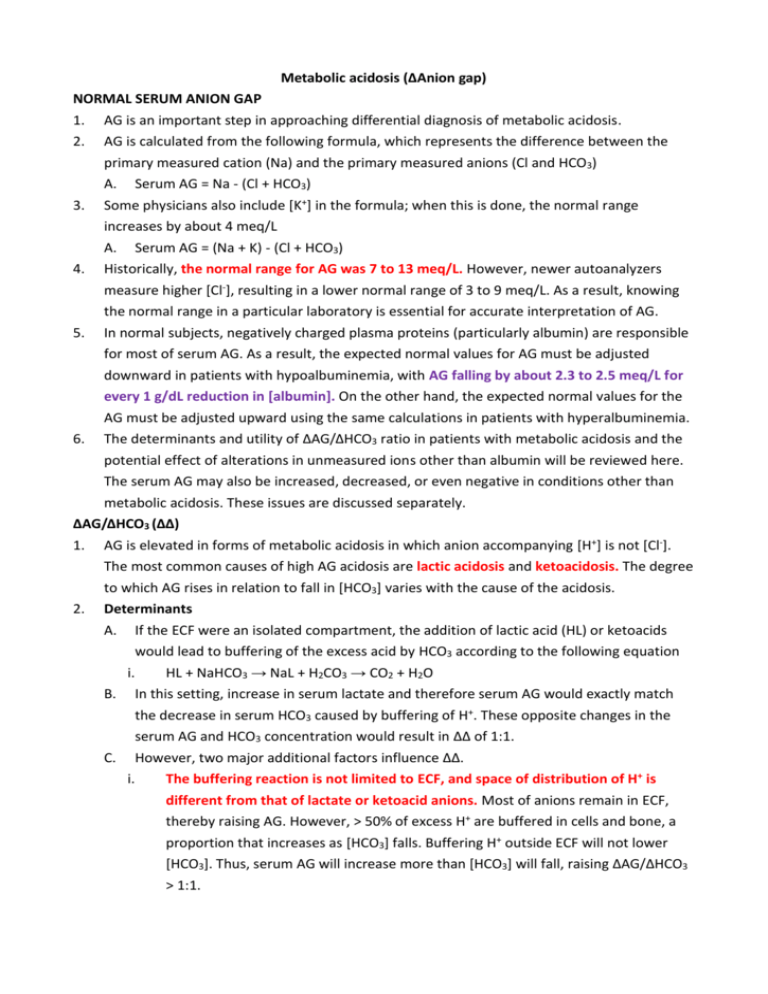
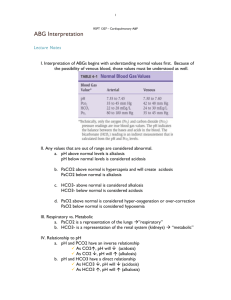
Metabolic acidosis (ΔAnion gap) NORMAL SERUM ANION GAP 1. 2. 3. 4. 5. 6. AG is an important step in approaching differential diagnosis of metabolic acidosis. AG is calculated from the following formula, which represents the difference between the primary measured cation (Na) and the primary measured anions (Cl and HCO3) A. Serum AG = Na - (Cl + HCO3) Some physicians also include [K+] in the formula; when this is done, the normal range increases by about 4 meq/L A. Serum AG = (Na + K) - (Cl + HCO3) Historically, the normal range for AG was 7 to 13 meq/L. However, newer autoanalyzers measure higher [Cl-], resulting in a lower normal range of 3 to 9 meq/L. As a result, knowing the normal range in a particular laboratory is essential for accurate interpretation of AG. In normal subjects, negatively charged plasma proteins (particularly albumin) are responsible for most of serum AG. As a result, the expected normal values for AG must be adjusted downward in patients with hypoalbuminemia, with AG falling by about 2.3 to 2.5 meq/L for every 1 g/dL reduction in [albumin]. On the other hand, the expected normal values for the AG must be adjusted upward using the same calculations in patients with hyperalbuminemia. The determinants and utility of ΔAG/ΔHCO3 ratio in patients with metabolic acidosis and the potential effect of alterations in unmeasured ions other than albumin will be reviewed here. The serum AG may also be increased, decreased, or even negative in conditions other than metabolic acidosis. These issues are discussed separately. ΔAG/ΔHCO3 (ΔΔ) 1. AG is elevated in forms of metabolic acidosis in which anion accompanying [H+] is not [Cl-]. The most common causes of high AG acidosis are lactic acidosis and ketoacidosis. The degree to which AG rises in relation to fall in [HCO3] varies with the cause of the acidosis. 2. Determinants A. If the ECF were an isolated compartment, the addition of lactic acid (HL) or ketoacids would lead to buffering of the excess acid by HCO3 according to the following equation i. HL + NaHCO3 → NaL + H2CO3 → CO2 + H2O B. In this setting, increase in serum lactate and therefore serum AG would exactly match the decrease in serum HCO3 caused by buffering of H+. These opposite changes in the serum AG and HCO3 concentration would result in ΔΔ of 1:1. C. However, two major additional factors influence ΔΔ. i. The buffering reaction is not limited to ECF, and space of distribution of H+ is different from that of lactate or ketoacid anions. Most of anions remain in ECF, thereby raising AG. However, > 50% of excess H+ are buffered in cells and bone, a proportion that increases as [HCO3] falls. Buffering H+ outside ECF will not lower [HCO3]. Thus, serum AG will increase more than [HCO3] will fall, raising ΔAG/ΔHCO3 > 1:1. ii. 3. little or no renal function. To the extent that ketoacid anions are excreted with sodium or potassium, serum AG will fall without concomitant increase in [HCO3], lowering the ΔAG/ΔHCO3 < 1:1 and resulting in the development of hyperchloremic (normal AG) acidosis after insulin therapy is initiated and extracellular volume repletion has been achieved. Lactic acidosis A. In lactic acidosis, lactic acid is buffered by HCO3 according to following equation. i. HL + NaHCO3 → NaL + H2CO3 → CO2 + H2O B. The ensuing increase in unmeasured anion lactate will raise AG. From this equation, it C. 4. The renal excretion of anions and H+ occur at different rates. This applies more to ketoacidosis than hypoperfusion-induced lactic acidosis in which there is typically may be assumed that there is 1:1 relationship between increase in ΔAG and fall in ΔHCO3. However, most of lactate anions remain in ECF, and urinary lactate excretion is limited in hypoperfusion-induced lactic acidosis where there is typically little or no renal function. In contrast, > 50% of the excess [H+] are buffered in cells and bone in mild metabolic acidosis and higher proportion in more severe metabolic acidosis. The net effect of the larger space of distribution of [H+] compared to lactate acid and the low rate of lactate excretion is that ΔΔ is typically > 1 in lactic acidosis, and is usually about 1.6. Thus, patient with lactic acidosis and [HCO3] of 14 meq/L should have serum AG of approximately 25 meq/L (16 meq/L above normal if the normal value is approximately 9 meq/L). However, [H+] buffering in cells and bone may take several hours to reach completion. Thus, ratio will initially be close to 1:1 with acute lactic acidosis and then increase with time. Urinary loss of unmeasured anions A. Urinary excretion of unmeasured anions can affect ΔΔ. This most often occurs in patients with DKA but can also be seen in D-lactic acidosis and toluene intoxication. B. Ketoacidosis i. The ΔΔ in patients with ketoacidosis averages about 1:1. This is in contrast to average ratio of 1.6 described in preceding section in lactic acidosis due to hypoperfusion. An important reason for this difference is relative maintenance of renal function in ketoacidosis, which allows ketoacid anions to be lost in urine as ii. Na+ and K+ salts. The loss of ketoacid anions lowers AG without affecting [HCO3], thereby reducing ΔΔ. The quantity of ketoacid anions excreted in patients with DKA depends upon the degree to which GFR is maintained 1. Patients with impaired renal function (due to underlying diabetic nephropathy and/or volume depletion) will retain greater fraction of ketoacid anions and have relatively high ΔΔ, similar to that seen in hypoperfusion-induced lactic acidosis. 2. iii. iv. v. Patients who maintain relatively normal renal function (including those with alcoholic or fasting ketoacidosis) can lose large quantities of ketoacids in urine and may have ΔΔ < 1. The urinary loss of ketoacid anions as Na+ and K+ salts represents loss of what has been called "potential HCO3" since, if they had not been excreted, metabolism of these anions would have resulted in regeneration of bicarbonate and reversal of the acidosis. In addition, loss of Na+ and K+ with ketoacid anions contributes to both ECF depletion and K+ depletion. Following institution of appropriate therapy for DKA, correction of hypovolemia with IV saline will initially result in increased excretion of ketoacid anions, while insulin therapy will slow ketogenesis and promote metabolism of ketoacids. As result of urinary loss of potential HCO3, almost all patients with DKA who have relatively intact renal function develop hyperchloremic (normal AG) metabolic acidosis following insulin. The findings are different in patients with advanced CKD. In this setting, there is only limited loss of ketoacid anions (potential HCO3) in urine and insulin therapy will return [HCO3] to values close to those at baseline. In contrast to tubular reabsorption of some of filtered β-hydroxybutyrate and acetoacetate in ketoacidosis, there is limited or no reabsorption of D-lactate or hippurate (generated from toluene metabolism). As a result, these anions will be more rapidly eliminated from plasma, potentially normalizing anion gap in D-lactic acidosis or after toluene inhalation. C. D-lactic acidosis i. D-lactic acidosis is rare disorder that most often occurs in patients with jejunoileal bypass or short-bowel syndrome. It is caused by combination of bacterial overgrowth and increased glucose and starch delivery into colon (due to lack of normal absorption in small intestine). As a result, dietary carbohydrate is converted to D-lactate, rather than physiologically occurring L-lactate. ii. The sodium-L-lactate cotransporter in proximal tubule is stereospecific and does not bind D-lactate. Thus, filtered D-lactate is rapidly excreted in urine and serum AG is increased less than expected from degree of fall in serum bicarbonate and may be normal. D. Toluene inhalation i. Urinary anion loss is even more rapid after toluene inhalation due to glue-sniffing. Toluene is converted in part into hippuric acid, which will initially tend to cause high AG acidosis. However, hippurate is both filtered across glomerulus and secreted into tubular lumen by proximal tubular cells. The net effect is that almost all of the hippurate presented to kidney is excreted (largely as sodium and potassium salts). Thus, most patients with toluene ingestion present with volume depletion, hypokalemia that is often severe, and normal AG acidosis. 5. 6. Other causes of low ΔΔ A. Several conditions other than those associated with urinary loss of unmeasured anions can lead to metabolic acidosis and ΔΔ < 1. i. In CKD, tubular damage may result in increased excretion of filtered anions while the degree of hydrogen secretion is limited. ii. In combined high and normal AG acidosis, as might occur if diarrhea were superimposed upon any high AG metabolic acidosis or if severe diarrhea led to reduced tissue perfusion and lactic acidosis. Other causes of high ΔΔ A. Some patients with high AG metabolic acidosis have ΔΔ that is higher than expected (> 1.6:1 in lactic acidosis or > 1:1 in ketoacidosis occurring in patients with preserved renal function). These patients have mixed acid-base disorder in which [HCO3] is higher than expected due to concurrent metabolic alkalosis (vomiting) or to compensatory increase in [HCO3] induced by preexisting chronic respiratory acidosis. POTENTIAL SOURCES OF ERROR 1. The utility of ΔΔ in patients with high AG metabolic acidosis is dependent upon several assumptions. A. That the baseline serum AG can be accurately estimated, an issue that is particularly important in view of the lower normal serum AG with newer autoanalyzers. Evaluation of recent previous blood test results, if available; provide the best way of determining the usual serum AG for a specific patient. In addition, normal values for the AG must be B. C. adjusted downward in patients with hypoalbuminemia, with the serum AG falling by about 2.3 to 2.5 meq/L for every 1 g/dL reduction in serum albumin. That the accumulating anions are derived from acids that are responsible for the acidemia. In some cases, unmeasured anions accumulate in plasma that is unrelated to metabolic acidosis. As an example, severe diarrhea can induce both hyperproteinemia due to hemoconcentration and hyperphosphatemia due to acidosis-induced movement of phosphate from cells into ECF. The net effect will be an elevation in AG, even though diarrhea alone produces normal AG acidosis (unless the volume losses are so large that lactic acidosis is superimposed). Hyperphosphatemia may also contribute to high AG in patients with DKA. Changes in concentration of other unmeasured anions (hypoalbuminemia) or of unmeasured cations (K+, Ca2+, or Mg2+). As an example, both hypoalbuminemia and hyperkalemia can lower AG. Thus, a patient with one or both of these disorders may have baseline AG of 4 rather than 8 meq/L. In this setting, AG of 13 meq/L, which is mildly above "normal," represents a true elevation in the AG of 9 meq/L. As a result, calculation of the ΔΔ is most accurate when the pre-acidosis AG is known. SERUM AG WITHOUT METABOLIC ACIDOSIS 1. Although the serum anion gap is primarily measured in patients with metabolic acidosis, it can be increased, low, or even negative in conditions other than metabolic acidosis. SUMMARY AND RECOMMENDATIONS 1. Assuming that the baseline serum AG is known or can be accurately estimated, ΔΔ in an 2. 3. uncomplicated high AG metabolic acidosis (shock-induced lactic acidosis) should be between 1 and 2. A lower value of ΔΔ can be seen in number of settings A. With urinary anion losses, as in ketoacidosis, D-lactic acidosis, or toluene intoxication. In these disorders, the ΔΔ is often < 1 and the serum AG may be normal. B. In some cases of chronic kidney disease in glomerular filtration is relatively well preserved and tubular damage results in increased excretion of filtered anions while the degree of hydrogen secretion as ammonium is limited. C. In a combined high and normal AG acidosis, as might occur if diarrhea were superimposed upon any high AG metabolic acidosis or if severe diarrhea led to reduced tissue perfusion and lactic acidosis On the other hand, higher value (ΔΔ > 2) usually reflects a mixed acid-base disorder in which [HCO3] is higher than expected