Bipolar Disorder - Nancy Rappaport
advertisement
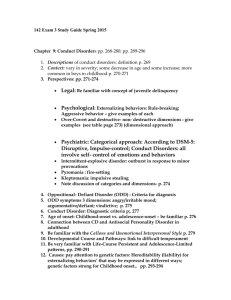
Bipolar Disorder & Post Traumatic Stress Disorder Nancy Rappaport, MD Harvard Medical School Bipolar Disorder • Also known as manic depression, a mental illness that causes a person’s moods to swing from extremely happy and energized (mania) to extremely sad (depression) • Chronic illness; can be life-threatening • Most often diagnosed in adolescence Epidemiology of Bipolar Disorder • Prevalence: 1% of population Adults = Adolescents • Males = Females • 2-3 million American adults are diagnosed with bipolar disorder • NIMH estimates that one in very one hundred people will develop the disorder Time Magazine, August 19, 2002 Nirvana’s Lithium I'm so happy 'cause today I've found my friends They're in my head I'm so ugly, but that's okay, 'cause so are you... We've broken our mirrors Sunday morning is everyday for all I care... And I'm not scared Light my candles in a daze... 'Cause I've found god - yeah, yeah, yeah I'm so lonely but that's okay I shaved my head... And I'm not sad And just maybe I'm to blame for all I've heard... But I'm not sure I'm so excited, I can't wait to meet you there... But I don't care I'm so horny but that's okay... My will is good - yeah, yeah, yeah I like it - I'm not gonna crack I miss you I'm not gonna crack I love you I'm not gonna crack I kill you I'm not gonna crack Controversy • • • • Severity and duration Onset before puberty is estimated to be rare Developmental variability Retrospective study of adults Vincent Van Gogh “It isn’t possible to get values and color. You can’t be at the pole and the equator at the same time. You must choose your own line, as I hope to do, and it will probably be color.” Assessment/Diagnosis of Bipolar Disorder • Often very complicated; it mimics many other disorders and has comorbidity (presents with other disorders) • Alphabet soup diagnosis • Half of bipolar children have relatives with bipolar disorder Other Organic Diagnoses • It is important to first rule out the possibility of any other organic diagnosis: – – – – Thyroid disorder Seizure disorder Multiple sclerosis Infectious, toxic, and drug-induced disorders Genetics • 30-70% • 75% Identical twins Both parents bipolar Mood history • Mania – Giddy, goofy, laughing fits, class clown – Explosive (how often, how long, how destructive and aggressive) – Irritable, cranky, angry, disrespectful, threatening – Grandiosity may present as EXTREME defiance and oppositionality • Depression – Low frustration tolerance, self-destructive, no pleasure, lower level of irritability DSM Criteria • A distinct period of abnormally and persistently elevated, expansive, or irritable mood • DIGFAST acronym (at least 3 of 7 symptoms) DIGFAST – Mental Status Exam • • • • • • • Distractible Increased activity/psychomotor agitation Grandiosity/Super-hero mentality Flight of ideas or racing thoughts Activities that are dangerous or hypersexual Sleep decreased Talkative or pressured speech Bipolar Disorder • Significant functional impairment • Bipolar I people go through cycles of major depression and mania • Bipolar II similar to Bipolar I except that people have hypomanic episodes, a milder form of mania • Rapid cyclers Suicide Risk Factors • 22% of adolescents with completed suicides had bipolar disorder • Family history of suicide • Substance abuse i.e. adolescent with impulse control disorder, depression, suicidality, substance use and access to a weapon is potential for lethality • Major depression often presents first (estimated that 20 - 40% of children presenting with major depression within 5 years will be bipolar) • Comorbidity • 70 - 90 % of adolescents have other disorders • ADHD, Conduct Disorder, Substance abuse Pediatric-Onset Bipolar Disorder • Geller (American Journal of Psychiatry, 2001) followed up 72 depressed prepubertal children into adulthood • 48.6% (N=35) developed bipolar disorder by mean age 20.7 years • Atypical presentation in juvenilesexacerbation of disruptive behavior, moodiness, low frustration tolerance, explosive anger and difficulty sleeping at night • Comorbidity of ADHD/BPD more severe presentation, often severe affect dysregulation, marked impairment, violent temper outbursts Pediatric-Onset Bipolar Disorder: Differential Diagnosis with ADHD Talkativeness Physical hyperactivity Distractibility • ADHD confusion although identifying presence of mood disorder helpful in guiding treatment • ADHD criteria does not include a mood component (usually comorbid ODD) • Look for family history data to help with diagnosis of bipolar disorder • Nonverbal learning disorders overlap Developmental Variability • Discrete episodes may be difficult to delineate more CHRONIC COURSE • Children with bipolar disorder are more likely to present with aggressive temper outbursts or affective storms rather than euphoric presentation Prioritizing Target Symptoms 1. Treat mania and/or psychosis 2. Treat depression 3. Anxiety and ADHD Medications • Mood Stabilizers • Lithium • Divalproex Sodium (Depakote) • Carbamezapine • Improvement is seen when mood stabilizers are used • Kowatch et al (JAACAP 2000) • Response rates: – 53% – 38% – 38% depakote lithium carbamazepine Geller et al. • High relapse rate • Geller longitudinal study – 1 year f/u recovery rate – Relapse rate 37% 38% Newer Agents • • • • • Neurontin Lamictal Topamax Gabatril Atypical antipsychotics Atypical Antipsychotics • • • • • Risperidol Olanzapine (Zyprexa) Quetiapine (Seroquel) Abilify Geodon Atypical Antipsychotics (ctd.) • Increasingly used because they can cause rapid patient stabilization • Zyprexa can help with depression, mania and psychosis • Weight gain Key Point • Just because a child improves on a mood stabilizer does not prove the diagnosis. Mood stabilizers have been used for a long time to help with aggression in children. Multiple Modalities • • • • • • • • Psychotherapy Psychoeducation/Support School Support/Consultation Residential Placement, Acute Hospitalization Mood Charting Teach Good Sleep Hygiene Legal intervention Hope The Explosive Child Ross Greene, PhD The Basket Model Common Approaches to Problems/Unmet Expectations • Basket A: Impose adult will • Basket B: Collaborative problem solving (work it out); problem-invitation • Basket C: Drop it (for now, at least) Entering the Baskets • Basket A: “No”, “You must,” “You can’t” • Basket B: Empathy, problem, invitation • Basket C: I didn’t bring it up Basket Model (ctd.) • Basket A: He did what I said • Basket B: We worked it out, we solved the problem. • Basket C: I didn’t bring it up Treatment Objectives • • • • Reduce meltdowns Teach lacking skills Flexibility Frustration tolerance Reminder!! • Meltdowns are 99.9% predictable Post Traumatic Stress Disorder • Impact of traumatic experiences affects capacity to function in school • Physical abuse • Sexual abuse • Domestic violence PTSD • Nature, duration, severity, and history of exposure is critical in shaping the brain response. Children reflect the world in which they are raised. • Dramatic, unpredictable, threatening changes in the environment • Stress response Trauma and Immigration • Escaping political terror or ethnic persecution • Cumulative losses • Staggered patterns of entry PTSD - Symptoms • Hyperarousal (most common symptom; startled response, behavioral irritability, sleep disturbances, regulatory functions off, hypervigilance, emotional numbing, or dissociation) • Nightmares • Flashbacks • Upsetting reminders and triggers Active Avoidance Passive Avoidance Fight or Flight • Fight or Flight response alarm reaction then fear (experience in the high school, sometimes inappropriate escalating behavior by adults to child’s apparent impertinence) • Freezing: hyperarousal, dissociation response seen as oppositional Trauma: Common Ways of Thinking (Automatic) • • • • • • “All or nothing” “Again and Again” “Must”, “Should”, or “Never” “End of the world” Always blaming yourself Thinking on the downside Impact of Trauma on Learning • Hypervigilant • Highly aroused • High speed “on” or “off” Impact of Trauma on Learning (ctd.) • Interference with cognition and information processing • Difficulty processing verbal information with a disproportionate emphasis on nonverbal clues • Difficulty regulating emotions and differentiating emotions • Language used to distance people • Locus of control gives up easily PTSD • • • • Secondary attachment figure Pianta’s work “Banking” Error history - disorganized attachment Islands of competency PTSD (ctd.) • No particular medication • Low doses of SSRI if depression and anxiety present • Risks/benefits Exercise: The 5 Steps of Cognitive Restructuring 1. SITUATION Ask yourself: What happened that made me upset?” Write down a brief description of the situation. Situation: _________________________ 2. FEELING Circle your strongest feeling (if more than one applies, use a separate sheet for each feeling): Fear/Anxiety Guilt/Shame Sadness/Depression Anger 3. THOUGHT Ask yourself: “What am I thinking that is leading me to feel this way?” Identify the thought that is most strongly related to the circled feeling. Write down your thought below. THOUGHT: _______________________ __________________________________ __________________________________ If it applies, circle your common style of thinking: Again and Again Too Much Risk Must/Should/Never End of the World Always Blaming YourselfAll or None Thinking on the Downside Thinking With Your Feelings 4. CHALLENGE YOUR THOUGHT Rewrite thought from Step 3: __________ Now ask yourself: “What evidence do I have for this thought? Is there an alternative way to look at the situation? How would someone else think about the situation?” Write down the answers that DO and DO NOT support your thought: Things that DO support my thought: __________ ________________________________________ Things that DO NOT support my thought: ______ ________________________________________ 5. OUTCOME Next, ask yourself: “Overall, does the evidence support my thought or not?” Look at all the things that support your thought and balance them against all the things that do not support your thought. Check the box below to see whether your thought it supported by the evidence or not: No, my thought is not supported by the evidence. If your thought is NOT supported by the evidence, come up with a new thought that is supported by the evidence. These thoughts are usually more balanced and helpful. Write your new, more helpful thought in the space below. And remember, when you think of this upsetting situation in the future, replace your unhelpful, automatic thought with the new, more accurate thought. New Thought: __________________________ ______________________________________ In some cases, even if you decide that your thought is not supported by the evidence, or is only partially supported, you may want to come up with an action plan. Typically this is to help you cope with upsetting feelings that arise even though you have come up with a more balanced thought. If you have an action plan for the situation, write it below. Action Plan: _________________________ YES, my thought is supported by the evidence. If your thought IS supported by the evidence, decide what you need to do next in order to deal with the situation. Ask yourself: “Do I need to get more information about what to do?” “Do I need to get some help?” “Do I need to take steps to make sure I am safe?” Write down your action plan to deal with the upsetting situation below. Action Plan: _____________________________ ________________________________________ Guide to Thoughts and Feelings FEELINGS ASK YOURSELF Related Thoughts Fear, nervousness, anxiety What bad thing do I expect to happen? What am I scared is going to happen? •Something terrible is going to happen •I am going to be attacked or hurt •I am going to be rejected or abandoned •I am going to lose control or go crazy Sadness or depression What have I lost? What is missing in me or in my life? •I am not worth anything •I don’t have anyone I can depend on •Nothing will ever get better •Life is not worth living Guide to Thoughts and Feelings FEELINGS ASK YOURSELF Related Thoughts Guilt or shame What bad thing have I •I am not good enough done? •I am to blame for what What is wrong with me? happened to me •I am a bad person •I am a failure Anger What is unfair about the situation? Who has wronged me? •I am being treated unfairly •I am being used •The situation is unfair •Someone has done something wrong to me I AM SPECIAL I am special. In all the world there is nobody like me. Since the beginning of time, there has never been another person like me. Nobody has my smile. Nobody has my eyes, my nose, my hair, my voice. I am special. No one can be found who has my handwriting. Nobody anywhere has my tastes - for food or music or art. No one sees things just as I do. In all of time there has been no one who laughs like me, No one who cries like me. And what makes me laugh or cry will never provoke identical laughter and tears from anybody else, ever. No one reacts to a situation just as I would react. I am special. I am the only one in all creation who has my set of abilities. Oh, there will always be somebody who is better at one of the things I am good at, but no one in the universe can reach the quality of my combination of talents, ideas, abilities and feelings. Like a room full of musical instruments, some may excel alone, but no one can match the symphony sound when all are played together. I am a symphony. Through all of eternity no one will ever look, talk, walk, think or do like me. I am special. I am rare. And in rarity there is a great value. Because I am rare, I need not attempt to imitate others. I will accept and even celebrate my differences. I am special. And I am beginning to realize it is no accident that I am special. I am beginning to see that I was made for a very special purpose. There must be a job for me that no one else can do as well as I. Out of all the billions of applicants, only one is qualified, only one that has the right combination of what it takes. That one is me. Because…I am…special.