(acronym) Trial - Clinical Trial Results
advertisement

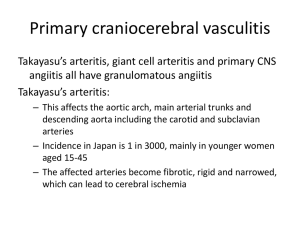
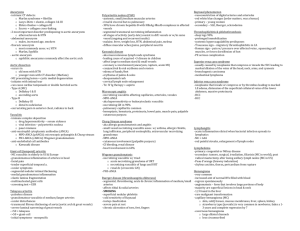
Vasculitis and Connective Tissue Disease Evaldas Giedrimas, MD Duane Pinto, MD The PVD . org Vasculitis Classification • Based on size of the vessel and histology of inflammatory cell: • Large Vessel - mononuclear infiltrates and inflammatory giant cells – Temporal or Giant Cell Vasculitis/Arteritis – Takayasu’s Arteritis – Cogan’s Syndrome • Medium Vessel – Polyarteritis Nodosa – Kawasaki’s Disease The PVD . org Vasculitis Classification (cont.) • Small Vessel – – – – Churg-Strauss Hypersensitivity Vasculitis Wegener’s Granulomatosis Bechet’s Disease • Scleroderma • Lupus (SLE) The PVD . org Vasculitis Overview • Definition – inflammation and necrosis of blood vessels • Idiopathic • Secondary • Etiology/Pathogenesis – humoral or cellular immune-related injury – Inflammation leads to narrowing or occlusion of the vascular lumen (stenosis), corresponding ischemia, local aneurysms, and possible ruptures • Epidemiology – rare The PVD . org Vasculitis Overview (cont.) • Symptoms • Physical Exam • Presentation – “Red Flags”: – Fever of unknown origin – Unexplained arthritis or myositis – Suspicious rash • Palpable purpura – Mononeuritis multiplex – Glomerulonephritis The PVD . org Vasculitis Overview (cont.) • Diagnosis • Differential Diagnosis • Treatment and Prognosis The PVD . org Large Vessel Vasculitis Temporal Arteritis/Vasculitis • Large branches of the carotid artery and aorta • Epidemiology – Age >50 – Women 3 X > Men – Whites > non-whites • Symptoms: – slow to develop tenderness, erythema, nodularity over the temporal artery; fever/headaches, PMR, jaw claudication and visual loss The PVD . org Large Vessel Vasculitis Temporal Arteritis/Vasculitis (cont.) • Physical Exam: – tender/thickened temporal arteries; bruits over carotid, supraclavicular, brachial, axillary and rarely over the orbits areas. May have associated distal joint synovitis (15-20%) • Diagnosis: – – – – high ESR, CRP, anemia, thrombocytosis, elevated IL-6 Temporal biopsy is preferred form of diagnosis Temporal arteritis patients should be screened for AAA US findings of hypoechoic halo can be helpful • Treatment: – 40-60 mg daily prednisone immediately after diagnosis The PVD . org Large Vessel Vasculitis Takayasu’s arteritis • Aorta and main branches • Epidemiology – Young, Asian women • Symptoms: – HTN, decreased peripheral pulses, AR The PVD . org Large Vessel Vasculitis Takayasu’s arteritis (cont.) • Diagnosis: – aortography/MRI, w/ narrowing of affected arteries and collateral circulation – associated with aorta coarctation and RAS – screening • Treatment: – glucocorticoids, cytoxic agents, – angioplasty, bypass and invasive intervention reserved for: • • • • The PVD . org HTN from RAS CVA Extremity ischemia with functional limitations Cardiac ischemia Large Vessel Vasculitis Cogan’s Syndrome • Mixed infiltrate of neutrophils and mononuclear cells with disruption of elastic lamina and vessel wall necrosis • Medium/small arteries, can extend to aortitis/carditis; • Autoimmunity against ocular and audiovestibular systems. • Epidemiology – Young The PVD . org Large Vessel Vasculitis Cogan’s Syndrome (cont.) • Symptoms: – interstitial keratitis and audiovestibular symptoms, often preceded by URI • Physical Exam: – – – – fever, myalgia, fatigue or weight loss, vertigo, nausea, vomiting, tinnitus, hearing changes, uveitis, optic neuritis, scleritis, AR due to valve inflammation; • Treatment: – early Prednisone 40-60 mg QD; hearing aids; AVR; The PVD . org Medium Vessel Vasculitis Polyarteritis Nodosa • Disseminated necrotizing vasculitis, initially involves intima and then progresses transmurally • Medium-sized and small muscular arteries • Symptoms: – SOB, LE edema – multi-organ: glomerulonephritis, mesenteric ischemia, polyarthralgia, overlapping connective tissue disease/myositis; The PVD . org Medium Vessel Vasculitis Polyarteritis Nodosa (cont.) • Physical Exam: – HTN, palpable purpura, CHF, scleritis • Diagnosis: – renal dysfunction – arteriographic documentation +/- biopsy • Treatment: – corticosteroids +/- cyclophosphamide The PVD . org Medium Vessel Vasculitis Kawasaki’s Disease • Mucocutaneous lymph node syndrome with mononuclear infiltrate with endothelial cell proliferation, elastic laminar disruption and vessel wall necrosis and potential aneurysm within 2 weeks • Large, medium or small arteries, carditis in 50% of patients The PVD . org Medium Vessel Vasculitis Kawasaki’s Disease (cont.) • Epidemiology – Male, children • Symptoms: – fever for 5+ days, and at least 4/5 of below: – Rash – Peripheral extremity changes such as erythema or edema of palms/soles and periungal desquamation – Bilateral conjunctival injection – Oral mucous membrane changes (fissured lips, injected pharynx, strawberry tongue) – Cervical lymphadenopathy The PVD . org Medium Vessel Vasculitis Kawasaki’s Disease (cont.) • Physical Exam: – cervical lymphadenopathy, oral changes • Diagnosis – anemia, neutropenia, thrombocytosis – EKG for MI findings with ruptured coronary aneurysm – Echo for aortic aneurysm The PVD . org Medium Vessel Vasculitis Kawasaki’s Disease (cont.) • Treatment and Prognosis – aspirin 80-100 mg/kg/day x 2 weeks AND – single high-dose IV IgG infusion of 2 g/kg within first 10 days of illness – No steroids – Echo at 8 weeks after diagnosis, if normal, then therapy can be stopped, otherwise ASA continued for at least 1 year. The PVD . org Small Vessel Vasculitis Churgg-Straus • Allergic angitis and granulomatosis with eosinophilia and extravascular granulomas in patients with asthma and/or allergic rhinitis – Small/medium muscular arteries • 40 The PVD . org y.o. male Small Vessel Vasculitis Churgg-Straus (cont.) • Symptoms – Respiratory: Initially URI, allergic rhinitis, asthma; – GI: diarrhea (2/2 to eosinophils bowel infiltration) +/- bleeding, bowel obstruction (due to nodules); – CNS: similar to polyarteritis nodosa – mononeuritis multiplex, symmetric peripheral neuropathy, ischemic optic neuritis and CN palsies; – Cardiac: pericarditis, MI; – Renal: UTI, FSGN; The PVD . org Small Vessel Vasculitis Churgg-Straus (cont.) • Physical Exam: – transient pulmonary findings, skin manifestations – purpura with leukocytoclastic vasculitis, granulomatous nodules • Diagnosis: – eosinophilia, + ANCA, extravascular granulomas, pulmonary infiltrates, hilar shadows, large pulmonary nodules, necrotizing vasculitis • Differential Diagnosis: – The PVD . org Wegener’s granulomatosis (no asthma, but more destructive airway component), Loffler’s syndrome, sarcoidosis, allergic bronchopulmonary aspergillosis. Small Vessel Vasculitis Churgg-Straus (cont.) • Treatment and Prognosis: – Corticosteroids – Immunosuppressives – Mean survival of 10 years after remission – Mortality due to cardiac and pulmonary failure The PVD . org Small Vessel Vasculitis Hypersensitivity Vasculitis • Cutaneous necrotizing, allergic, leukocytoclastic (small debris) vasculitis • Small vessels with <1 mm necrotic inflammation (PMNs +/- lymphocytes) • Epidemiology: – all ages, abrupt The PVD . org Small Vessel Vasculitis Hypersensitivity Vasculitis (cont.) • Physical Exam: - constellation of syndromes – cutaneous signs: palpable purpura, petechiae, vesicles, urticaria, papules, pustules, necrotic ulcerations, nodules – usually grouped; arthralgias, arthritis – knees ankles, wrists, elbows; hematuria – Cryoglobulinemia – MSK/NS involvements along with connective tissue disorders – HSP – gastrointestinal/IBS • Diagnosis: – high ESR, leukocytosis, eosiniphilia, anemia, hemepositive stool, hematuria, proteinuria, cryoglobulinemia, elevated LFTs/Cr. The PVD . org Small Vessel Vasculitis Hypersensitivity Vasculitis (cont.) • Differential Diagnosis: - collection of all or individual syndromes – Serums Sickness, drug hypersensitivity, Henoch-Schonlein purpura (IgA dominated), mixed cryoglobulinemia, and urticarial vasculitis (hypocomplement) • Treatment: – removal of offending agent, tx of systemic illness, spontaneous resolution up to 4 weeks, may require corticosteroids; hyperpigmentation scars The PVD . org Small Vessel Vasculitis Wegener’s Granulomatosis • Necrotizing granulomatous process of respiratory tract with GN – of unknown etiology, usually with FSGN • Necrotizing small artery and vein (fibrinoid) vasculitis – – at different healing stages, with mononuclear cell involvement • Young, middle-aged, male • Symptoms – upper and lower pulmonary involvement, cutaneous lesions, ocular disease, peripheral and CNS, carditis The PVD . org Small Vessel Vasculitis Wegener’s Granulomatosis (cont.) • Diagnosis: – may require tissue biopsy – high ESR, leukocytosis, thrombocytosis, anemia of chronic disease; – + Ab again proteinase 3, myeloperoxidase, human leukocyte elastase; + ANCA (93% with active disease), ANA • Differential Diagnosis: – SLE, other vasculitides, cholesterol atheroemboli, infective endocarditis, malignancies, fibromuscular dysplasia, and radiation fibrosis The PVD . org Small Vessel Vasculitis Wegener’s Granulomatosis (cont.) • Treatment: – cyclophosphamide and steroids; requirement of HD can be reversed; – if unTx, 90% of patients die within 2 years with respiratory or renal failure The PVD . org Small Vessel Vasculitis Behcet’s Syndrome • Vasoa vasorum vasculitis in large arteries and veins of unknown etiology – abnormal neutrophil and lymphocyte dysfunction • Eastern Mediterranean region, Turkey, prevalent along “Silk Road” – Associated with HLA-B51, HSV, parvovirus B19, HCV infection The PVD . org Small Vessel Vasculitis Behcet’s Syndrome (cont.) • Presentation: - multi system – oral aphthous and genital ulcers, skin lesions, uveitis, synovitis, valvular and coronary disease, meningioencephalitis, renal vascular hypertension, CVA, cerebral venous thrombosis, thrombophlebitis of both superficial and DVT, claudication The PVD . org Small Vessel Vasculitis Behcet’s Syndrome (cont.) • Diagnosis: CT, MRI, angiography, VQ scan – Recurrent Oral ulceration - Aphthous or herpetiform ulcers, • observed by MD or patient, with >3 episodes over 12 months – Recurrent Genital Ulceration - Aphthous ulceration or scarring – Eye lesions - detection by an ophthalmologist • Anterior and posterior uveitis, retinal vasculitis, vitreous cells on slit-lamp examination; The PVD . org Small Vessel Vasculitis Behcet’s Syndrome (cont.) • Diagnosis (cont.) – Skin lesions • Erythema nodosum, papulopustular, pseudofollicular lesions or acneform nodules in post-adolescent patient w/out corticosteroids – Positive pathergy test: • + by MD at 24-48 hours (skin hypersensitivity to HLA B5 Ag) • Treatment: – estradiol, dapsone, colchicine, cyclosporine, levamisole The PVD . org Buerger’s Disease (Thromboangiitis Obliterans) • Non-atherosclerotic, segmental, inflammatory thrombotic disease with sparing of vessel wall – Small and medium arteries, veins and nerves – Distal extremities, iliac arteries, renal, mesenteric, internal thoracic arteries, pulmonary, coronary, aorta and cerebral arteries, • PMNs, micro-abscesses, and multinucleated giant cells, progressive organization of thrombus, with subsequent quieting of inflammation • 40-45 y.o. men, Far & Middle East, Ashkenazi Jews, tobacco use The PVD . org Buerger’s Disease (Thromboangiitis Obliterans) (cont.) • Symptoms: – ischemia of distal small arteries/veins in proximal distribution, manifesting as ulcers and claudication of the feet, legs, hands or arms, Raynaud’s. • Diagnosis: – Highly pathognemonic: • (1) Age <45, (2) current/recent tobacco use, (3) distal extremity ischemia and exclusion of autoimmune and hypercoagulable diseases (4) Nl ESR, nl CRP, nl ANA, RF, cryoglobulins, complements (5) Positive Allen test in young smoker with leg ulcerations – TTE to r/o embolization, arteriogram to assess multiple limb involvement The PVD . org Buerger’s Disease (Thromboangiitis Obliterans) (cont.) • Differential Diagnosis: – scleroderma, CREST, emboli, hypercoagulable states, repetitive trauma, other vasculitides • Treatment: – discontinuation of cigarette smoking – Surgery is not recommended due to diffuse segmental involvement The PVD . org Scleroderma • Presence of thickened, sclerotic skin +/- vascular involvement – CREST (Calcinosis, Raynod’s, Esophageal dysmotility, sclerodactyly, telangiectasia) – Systemic sclerosis – includes skin and diffuse disease/organ involvement • Fibrosis of musculoskeletal, renal, pulmonary, cardiac and GI systems The PVD . org Scleroderma (cont.) • Immune system, endothelial dysfunction, enhanced fibroblast activity – Vascular injury occurs through endothelial cell injury leading to eventual obliteration of the vessel lumen and ensuing ischemia • Activated cytokines (IL-2, TGF-b) • Symptoms: – Raynaud’s, digital ulcers or infarcts, arrhythmias The PVD . org Scleroderma (cont.) • Diagnosis: – clinical findings, skin Bx not necessary – Systemic scleroderma - Should fulfill 1 major or 2/3 minor criteria • Major criteria: – proximal to MCP sclerodermitis skin changes • Minor criteria: – sclerodactyly, digital pitting, scars of fingertips or loss of substance – of the finger pad, bibasilar pulmonary fibrosis The PVD . org SLE Affects skin, joints, kidneys, lungs, nervous system, serous membranes • – unknown cause – Chronic deposition of immune complexes, cytokine effects, direct attack by Ab or leukocytes on renal glomeruli, joins, pleural or pericardial serosa, cardiac or vascular endothelium, cardiac valves, and oral or conjuctival mucosa – fatigue, fever, pleuritic chest pain, in a young woman, found to have hypertension, mallar rash, a pleural friction rub, several tender and swollen joints, and mild peripheral edema The PVD . org SLE (cont.) • Epidemiology – Women in 20-30 – Genetic, environmental – Meds: phenytoin, hydralazine, procainamide, isoniazide can contribute to SLE. The PVD . org SLE • Vasculitis Presentation – Small vessels - degenerative changes with minimal inflammatory changes, chronic immune complex deposition, cytokine effects on vascular endothelium – Large to medium vessels - more classic vasculitis with local thrombosis from anti-phospholipid Ab, which can involve various sized arteries or veins. – Endocarditis, with sterile inflammation with diffuse microembolization The PVD . org