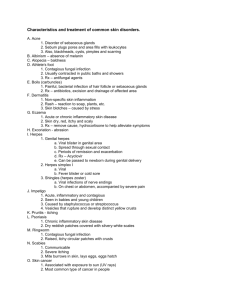
It is how to get

STDs/STI.Froberg.3-4-10.Heather Grothe
Purpose
Learn for the most common/important STIs:
The classification and characteristics of each etiologic agent, epidemiology, prevalence (incr/decr), spectrum of clinical disease, diagnosis, pathology, treatment (pharmacology lectures) and prevention.
Organisms
1. Viruses
Herpes simplex viruses: HSV-1 & HSV-2
Human papilloma viruses: HPV
Human Immunodeficiency Virus: HIV (covered elsewhere)
Hepatitis B Virus: HBV (covered elsewhere)
2. Protozoa
Trichomonas vaginalis
3. Bacteria
Chlamydia trachomatis
Neisseria gonorrhoeae
Treponema pallidum
Haemophilus ducreyi
Important Concepts
Many STIs asymptomatic/subclinical
Are 5 of the 10 most common infections reported by CDC
Rates of STIs probably underestimated
Concurrent infections common
Nearly all STIs
risk of HIV infection
> 15 million STIs per year in US
Rates in US double those of England, Canada, Germany, Sweden
While syphilis & gonorrhea have declined recently, chlamydia, HPV & HSV have all
Physicians may not include an adequate sexual Hx and genital exam as part of routine H & P
www.cdc.gov/std/
Frequency/Impact
HPV: ~ 20 million infected in US, 5.5 million new infections per year
HSV-2: ~ 45 million infected in US
Chlamydia*: > 3 million new infections per year in US
Trichomoniasis: ~ 5.5 million infected
Gonorrhea*: ~ 360,000 cases reported in 2001
Syphilis*: ~ 6,000 cases reported in 2001, 440 congenital
Reportable in Minnesota
HSV 1 & 2
Enveloped DNA viruses causing cold sores & genital herpes
Genital herpes mostly HSV-2, but HSV-1 increasing (up to 40% in some populations)
Facial herpes mostly HSV-1 (5% HSV-2)
Antibodies to one somewhat inhibitory to the other
Genomes show 50-70% homology between HSV-1 & HSV-2
Man only natural host
Clinical Disease
Localized vs disseminated (
in immunosuppressed)
Herpes Labialis : cold sores
Ocular Herpes: keratoconjunctivitis
Herpes Genitalis
Cutaneous lesions: herpetic whitlow
Meningitis- esp in newborns or immunocomprimised
Encephalitis: temporal lobe
Repro_STI/STD_Froberg_3-4-10_Heather Grothe 1
Neonatal herpes
Herpesvirus Particle
HSV-2 virus particle. Note that all herpesviruses have identical morphology and cannot be distinguished from each other by electron microscopy.
Herpes
HSV is spread by contact, virus is shed in saliva, tears, genital and other secretions.
Most common form of infection results from a kiss given to a child or adult from a person shedding the virus.
HSV-1 1
infection is usually trivial or subclinical in most individuals.
There are 2 peaks of incidence, the first at 0 - 5 years and the second in the late teens, when sexual activity commences.
About 10% of the population acquires HSV infection through the genital route and the risk is concentrated in young adulthood.
Herpes Pathology
Latency in craniospinal ganglia
Reactivation: 45% for facial, 60% for genital
More likely (to become reactivated) if immunosuppressed
Triggers: stress, menstruation, infection, fever
Genital recurrence: 1.6 episodes/yr,
with time
Asymptomatic shedding highest in 1st six months following 1
infection – doesn’t have to have clinical disease to shed the virus
Genital Herpes
Causes latent & recurrent infections
Transmission: direct contact (genital/genital or oral/genital)
Most transmission when there are no active lesions
1
infection often more severe than recurrences
60% of pts have recurrent disease
Genital Herpes Pathology
Infection by direct contact with mucocutaneous tissue breaks
Prodrome of tingling, burning, pain
Polykaryons with intranuclear inclusions at base of vesicle
Papule
vesicle
ulcer
Intra-nuclear inclusions (Cowdry A & B), multinucleated giant cells at base of vesicle-(polykaryon)
Ulcer
2
infection (Staph, Strep, Candida)
Neonatal Herpes
HSV spread to neonate during vaginal delivery (doesn’t cross placenta)-contact problem
Mostly from asymptomatic mothers
Incidence: 1/4000 LBs in US
Transmission more common with 1
vs recurrent infection (33 vs 3% in one series)
Earlier gestational delivery
risk
Caesarian section
risk
80% due to HSV-2
50% mortality
CS x within first 10 days of life
Pathology: foci of necrosis in multiple organs (liver, adrenal, lung, brain)
Long-term CNS deficits/blindness in 25-30%
Cowdry A inclusion s of
HSV
Herpes/Histo
Polykaryons with intranuclear inclusions (nucleus looks clear, chromatin to periphery of cell
Laboratory Diagnosis
Virus Isolation o HSV-1 and HSV-2 are among the easiest viruses to cultivate. It usually takes only 1 - 5 days for a result to be available. Is gold standard.
Direct Detection o Tzanck smear of vesicle base
Repro_STI/STD_Froberg_3-4-10_Heather Grothe 2
o Immunofluorescence of skin scrapings - can distinguish between HSV and VZV o PCR - now used routinely for the diagnosis of herpes simplex encephalitis
Serology o Not that clinically useful.
Cell Culture o Cytopathic Effect of HSV in cell culture: Note the ballooning of cells.
Herpes Treatment
Antiviral chemotherapy indicated where the primary infection is especially severe, dissemination, sight is threatened, and herpes simplex encephalitis.
Acyclovir – this is the drug of choice for most situations.
I.V. (HSV infection in normal and immunocompromised patients)
Oral (treatment and long term suppression of mucocutaneous herpes and prophylaxis of HSV in immunocompromised patients)
Cream (HSV infection of the skin and mucous membranes)
Ophthalmic ointment
Famciclovir and valacyclovir – oral only, more expensive than acyclovir.
Acyclovir
Converted to acyclovir monophosphate by viral thymidine kinase
Then to acyclovir triphosphate by cellular kinases
inhibits viral DNA polymerase
early termination of viral
DNA
~1% of HSV lack thymidine kinase
resistant to acyclovir (amy be higher in some sub-populations)
Human Papilloma Virus
Naked dsDNA virus of papovavirus family
Produce latent & chronic infections
HPV replicates in epithelial cells of skin, vagina, cervix, larynx, etc.
Transmitted by direct contact
Tumorogenic: causes warts, anogenital condylomas and dysplasia
60-100 different types described, 30-40 infect human genitalia
Classified by genotyping (not serotyping like most other viruses)
Small virus (55 nm), circular DNA with 10 ORFs (E1-8, L1 & L2)
New type defined as having < 50% homology with known HPV types
Clinical Disease
Common warts: verruca vulgaris
Most common types: 1, 2, 4
Predilection for keratinized epithelium/do not cause genital lesions (except HPV 2)
Laryngeal warts: HPV 11 (~congenital transmission, can be big problem and obstruct breathing)
Tumorogenic Types
Anogenital warts (condyloma accuminatum): HPV 6, 10, 11, 40-45 (episomal viral DNA)
Types 6 & 11 ~ 70%
Cervical cancer: HPV 16, 18, 33, 45, 46
70% HPV 16 or 18 (integrated viral DNA)
HPV 16 most common type (50%) overall
HPV genomes found in >95% of all cervical cancer specimens
(squamous cell & adenocarcinomas)
270,000 deaths from cervical cancer worldwide
Pathology
Infected epithelial cells
koilocytes
Koilocytes: cells with
nuclear size,
N/C, irregular nuclear contours (raisinoid), nuclear hyperchromasia, perinuclear halo
Can transform cells in culture
E6 binds p53 (early degradation blocks apoptosis)
E7 binds Rb gene (unrestrained cell proliferation)
E7 from HPV replaces E2F at binding site with pRb. This allows transcriptional activation and cell proliferation.
Repro_STI/STD_Froberg_3-4-10_Heather Grothe 3
Epidemiology
Incidence and prevalence unknown
65% of sexual contacts of partners with condylomas displayed genital warts within 6 weeks
Multiple HPV types in ~ 25% of infections
Most infections spontaneously regress within 2 yrs
Most common in young adults, decline with age
Only a small minority of women with HPV DNA by molecular techniques have gross or microscopic abnormalities
HPV infection
4x if HIV +
HPV
Pathology & Rx: refer to lecture on cervix
HPV 16 vaccine clinical trials:
Females age 16-23 got HPV-16 virus- like-particle vaccine (x3) or placebo, followed and tested for HPV-16 infection for ~17 months
768 got vaccine with 0 HPV-16 infections
765 got placebo with 41 HPV-16 (3.8%/100 women-years) infections (NEJM 2002;347:1645-51)
Vaccine
Gardasil
recombinant virus-like particles (VLPs) from L1 protein (major capsid protein) o Lack viral DNA- thus no way they can get the infection o Prevents infection from types 6, 11, 16 & 18 (cause condylomas and dysplasia) o 6 & 11 cause ~90% of genital warts o FDA approved June 2006
Trichomonas vaginalis
Ubiquitous flagellated protozoan, most common non-viral STD per WHO
Lives in lumen of vagina, urethra, prostatic ducts, under foreskin of uncircumcised males
Does not invade tissues
170 million cases worldwide
Causes trichomoniasis
Humans only natural host
Fastidious, anaerobe
Iron from menses may facilitate overgrowth
Not reportable in US (~3-6 million new cases/yr)
Prevalence in STD clinics may approach 40%
Much less frequent in men (~5% of urethritis)
Peak incidence 16-35 yrs of age
risk if African-American, multiple sexual partners
Trichomoniasis
Transmission via sexual intercourse
Rate of infectivity estimated at 70-80%
Rates higher from men to women than women to men
Incubation period 4-28 days
Not spread by fomites
Clinical Disease
Acute or chronic vaginitis
Yellow-green, frothy or bubbly, purulent discharge, pruritis and dysuria
Discharge in < 50% of women
Exacerbated by menses (pH 5-5.5)
Urethritis more common in men
White, milky urethral discharge
Pathology
Gross: discharge, multiple, punctate hemorrhages and/or areas of capillary dilitation on cervix (“strawberry cervix”)
Organism may adhere to squamous epithelium
Repro_STI/STD_Froberg_3-4-10_Heather Grothe 4
Acute inflammation
Diagnosis & Treatment
Wet mount of scrapings of vaginal fornices
Can see motile organisms under phase contrast microscope
Others: Giemsa stain of scrapings , PAP smear, ELISA on vaginal secretions
Rx: metronidazole
82-100% cure rates
Should Rx sexual partners of women that have this
Chlamydia trachomatis
Small Gram negative bacterium , Obligate intracellular pathogens
Biphasic developmental cycle
Infectious form is elementary body (EB) : 0.3-0.4
m
EB is metabolically inert, more spore like
EB taken up by epithelial cells
reticulate body (RB) :RB metabolically active, Utilizes host cell ATP for energy
Multiples by binary fission within endosome (inclusion body with 100-500 progeny)
Result
host cell ruptures or expels inclusion body -> then spread to ther tissue
Infect columnar epithelium
Chlamydia inhibit fusion of endosome with lysosomes (resist intracellular killing)
Multiple biovars
D-K cause nongonococcal urethritis in men; urethritis, cervicitis, salpingitis and pelvic inflammatory disease
(PID) in women
Can cause inclusion conjunctivitis in neonates
L1-3 cause lymphogranuloma venereum (LGV rare in US- <600/yr)
Epidemiology
Most common bacterial STD in developed world
Rate in STD clinics 15-19%
Leading cause of ectopic pregnancy (PID)
Risk factors: < 25 yrs, African-American race, multiple sexual partners. Concurrent infection with GC
Majority of infections subclinical
Incubation period ~ 3 weeks
Diagnosis
Cell culture (takes 3-7 days) of vigorous swab of mucous membranes: use dacron or rayon swabs-submit in viral/chlamydial transport medium at 4
C
Endocervix preferred site (urethra from men)
DFA, gene probes, EIA
Clinical Disease
Ophthalmia neonatorum ( inclusion conjunctivitis) acquired during passage through birth canal
May develop pneumonitis
Adults may get from autoinoculation from genital tract (trachoma)- inflammation of the keratoconjuctival tissue
Males: 75% symptomatic
urethritis, dysuria & pyuria, proctitis
Females: 80% asymptomatic, some cervicitis, urethritis, salpingitis
40% of untreated females
pelvic inflammatory disease (PID)
Leads to tubal pregnancy, infertility
Tubal pregnancy = leading cause of 1st trimester pregnancy-related deaths
Females with chlamydia 3-5 fold
risk of HIV
More Clinical Disease
Reiter’s Syndrome: conjunctivitis, polyarthritis & genital infection
most HLA-B27 +
Lymphogranuloma venereum (L biovars): painful “buboes” = enlarged draining lymph nodes, may develop elephantiasis, ulcers or fistulas
Treatment
Tetracycline or erythromycin
No vaccines
Penicillin ineffective
Repro_STI/STD_Froberg_3-4-10_Heather Grothe 5
Important since gonococcus co-infections may occur
Gonorrhea
Neisseria gonorrhoeae
Gram negative diplococci, gonococcus (GC)
Frequently found intracellularly in PMNs
Is oxidase positive: cytochrome C oxidase phenylenediamine black color
Have pili
attach to mucosal surfaces
Pili show antigenic variation
Protein II (opacity)
clumping (self-aggregation)
IgA proteases
may degrade host IgA (produces in reproductive tract)
LPS
May bind to sperm, rbcs, non-ciliated fallopian tube epithelium
May invade
dissemination
Epidemiology
Incidence declining
May be under diagnosed in females (more apparent in males)
Still 500-700,000 cases per year in US
Highly contagious: 50% transmission rate
Chlamydia coexists in 45-50% of pts with gonorrhea
PAP smear with chlamydial inclusion body
Clinical Disease
Incubation 2-7 days
Males: urethritis, dysuria, pyuria (copius urethral discharge), epididymitis, proctitis, orchitis
Conjunctivitis in newborns exposed to infected secretions in birth canal
50% of women asymptomatic
Cervicitis, adenitis, proctitis, salpingitis, ovaritis, PID in 15% (less likely to cuase PID- CHalmydia main culprit)
Disseminated : more common during pregnancy (endocytosis of GC) seen in 0.3 - 3% of pts
Dermatitis
papules & pustules with hemorrhagic component
Arthritis
knees, elbows, tenosynovitis
Rarely
endocarditis, meningitis, Waterhouse-Friderichsen syndrome (hemorrhagic infarction of adrenals)
Diagnosis
Culture on Thayer-Martin media in high CO
2
(oxidase + colonies)
Gram negative cocci in pairs
GC don’t ferment maltose, meningococci do –( can distinguish from neisseri mennigits)
Gene Probe
Treatment
Penicillin resistance 15-19%
Tetracycline resistance 17-23%
Emerging fluoroquinolone resistance
No resistance to 3rd generation cephalosporins
Disseminated: 7-14 days
Syphilis
Treponema pallidum
Spirochete with axial filament (motile)
Gonorrhea
Gram negative but too thin to see by light microscopy (0.2 by 6-15
m)
Man only natural host (grows in rabbit skin/testes)
Never cultured in vitro
Transmission by direct sexual contact- with the open sores from syphyllis
Periods of latency and clinical disease
Infection may last decades
Since arrival of penicillin in 1940’s, rate has
Repro_STI/STD_Froberg_3-4-10_Heather Grothe 6
Produces no known toxins
Pathology likely from humoral and cellular immune responses
Syphilis
risk of HIV (HIV
risk of neurosyphilis) – b/c it causes open ulcer on genitalia
Clinical Disease
“Great Imposter”
Three stages: each involve lesser numbers with more severe CS x
1
syphilis
chancre (hard, clean, painless, shallow ulcer) occurs ~ 3weeks after exposure o Chancre: male
70% on penis or scrotum, female
50% on vulva or cervix, rest
lips, oral cavity, finger, base is teeming with treponema o Chancre resolves in 3-8 weeks
Rx o May have fever, lymphadenopathy
2
stage
2-10 weeks after
1 o 2
dissemination of spirochetes: diffuse macular rash including soles & palms, lymphadenopathy, erosions on mucous membranes, condyloma lata – these are anogenital warts (look a lot like HPV)
3
stage
latency may last decades
Three categories of tertiary syphilis: o Cardiovascular
aortitis, aortic aneurysm, aortic insufficiency (80% of mortality)- invasde vasovasorum of atora, develop aortic aneurism o Neurosyphilis
general paresis, meningovasculitis, tabes dorsalis (loss of posterior columns), psychiatric disease o Benign tertiary syphilis
gummas = necrotizing granulomas
skin, bones, subQ
Congenital Syphilis
Treponemes cross placenta after 5th month of gestation (more common if early syphilis)
Causes stillbirth, spontaneous abortion (50% mortality), early or late congenital syphilis
Early congenital: desquamating skin lesions,vesicles on mucous membranes, osteochondritis, pulmonary fibrosis, hepatosplenomegaly
Late congenital: interstitial keratitis, gummas, saddle nose, saber shin (> 2 yrs), Charcot joints
Classic triad: interstitial keratitis, notched incisors, eighth-nerve deafness
Pathology
Treponemes adhere to endothelium
obliterative endarteritis
Two major types of lesions: o perivascular plasma cells ( also lymphocytes, macrophages) o Gummas
necrotizing granulomas 2
to delayed type hypersensitivity
Diagnosis
Screening serology via non-treponemal tests:
1.
VDRL (Venereal Disease Research Laboratory)
2.
RPR (Rapid Plasma Reagin)
These test for anti-cardiolipin antibodies (are
in syphilis & many other diseases)
Are sensitive but non-specific
If chancre present
dark field microscopy of material from base of lesion
May be seen in silver stains or DFA staining of condylomas and skin lesions (less reliable)
Confirmatory Tests for 2
& 3
syphilis : more specific and expensive o FTA-ABS most widely used, remains + after Rx (TOC) o Microhemagglutination-TP also used
Hutchinson (notched) incisors
Treatment
Penicillin - no known resistance
Single dose for active, multiple doses for latent
May see Jarisch-Herxheimer reaction following Rx of 2
or 3
syphilis (hypersensitivity)
Like other STIs
condoms may not entirely prevent
Chancroid
Haemophilus ducreyi
Repro_STI/STD_Froberg_3-4-10_Heather Grothe 7
Gram negative rod
Now uncommon in US, common in Africa & SE Asia
Causes soft chancre: painful genital ulcer
Can be confused with syphilis, herpes, LGV
Male:female ratio 9:1
Predisposes to HIV
Characterized by single or multiple ulcers and inguinal adenopathy
Grows on chocolate agar
gram negative coccobacilli
Presumably make cytotoxin and endotoxin
Rx and Prevention
Some resistance to ampicillin and penicillin
Condoms may prevent
Vaginitis
Yeast vaginitis
80-90% Candida albicans
Are NL flora
overgrowth (birth control pills, antibiotics, diabetes)
May be sexually transmitted (usually not)
Dx: KOH wet mount for yeast, pseudohyphae & hyphae
Dysuria, creamy discharge
Rx: nystatin, imidazoles
Bacterial Vaginitis
Gardnerella vaginalis
Gram negative anaerobe
NL flora
Mild signs/increased odor (fishy)
Dx: clue cells-epithelial cells covered with bacteria
Rx: alter microenvironment
Repro_STI/STD_Froberg_3-4-10_Heather Grothe 8