Tactical Field Care - Center for Disaster and Humanitarian
advertisement

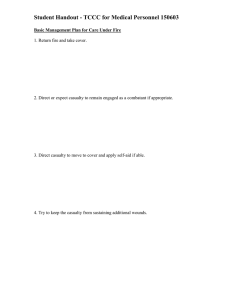
Tactical Combat Casualty Care Charles W. Beadling, MD, FAAFP, IDHA, DMCC Center for Disaster and Humanitarian Assistance Medicine Department of Military and Emergency Medicine Uniformed Services University PART II Tactical Field Care Tactical Field Care • Care rendered by the Medic once he and the casualty are no longer under effective hostile fire. • Applies to situations in which an injury has occurred, but there has been no hostile fire. • Available medical equipment still limited to that carried into the field by medical personnel. Time to evacuation to a MTF may vary considerably. Tactical Field Care • Casualty Assessment • Airway – Adjuncts – Definitive Control • Chest Wounds • Continued Hemorrhage Control – Hemostatic Agents, Pressure Dressings – Fluid resuscitation • Hypothermia, Infection Tactical Field Care • If a victim of a blast or penetrating injury is found without a pulse, respirations, or other signs of life, DO NOT attempt CPR • Casualties with confused mental status should be disarmed immediately of both weapons and grenades Tactical Field Care • • • • • • • Initiate Shock Prevention Protocols Pain Control Antibiotics Splint Fractures Prevent Hypothermia Prepare Casualty for Evacuation Documentation Airway Adjuncts and Control • Recovery Position • NPA • Cric Nasopharyngeal Airway Why No Endotracheal Intubation • • • • • DEBATABLE No studies on well trained medics Most medics have never used live tissue Standard ETT uses white light Extremely difficult with bloody maxillo-facial wounds • Esophogeal intubations much less identifiable in the field Tension Pneumothorax Breathing • Tension Pneumothorax – – – – – Respiratory distress Decreased breath sounds Hyperresonance Tracheal deviation JVD Needle Thorocostomy • 1996 – Presumptive Dx and Tx – Unilateral penetrating chest trauma & progressive respiratory distress • 2003 & 2006 – modified slightly – Now includes blunt torso trauma & respiratory distress even if it is not progressive Needle Thoracentesis • Emergently decompress affected hemithorax with 14gauge needle inserted over 3rd rib in 2nd inter-costal space at mid-clavicular line SubCommitee on Hemostatic Agents (CoTCCC Feb, ’09) By 26/1 vote WountStat is no longer recommended in TCCC guidelines Combat Gauze Emergency Bandage (Israeli Pressure Dressing) Emergency Bandage Fluid Resuscitation Protocol Hemorrhage Controlled • No Radial Pulse or Poor Mentation • Gain Access (saline lock) - 18Ga • Intraosseos What Fluid? • Bolus 500cc Hextend® – Re-assess after 30 min – 500cc Hextend® Bolus – No more than 1L Hextend® • Crystalloid – Normal Saline, Ringer’s Lactate • Blood PO Fluids? Blood Products PRBC on CASEVAC (if feasible) 1:1 FFP Reasons NOT to start an IV • Takes time • Potential waste of fluids Combat Pill Pack • Tylenol 650mg x 2 • Mobic (meloxicam) 15mg • Moxifloxacin 400mg Provider Adjuncts • Fentanyl (Oral Transmucosal Fentanyl Citrate) 800 mg taped to finger • Morphine 10 mg IV/IM • Promethazine 25mg IV/IM • Cefotetan 2gm IV/IM or Ertapenem 1gm IV/IM Improved First Aid Kit Tourniquet Nasopharyngeal Airway Gloves Israeli Battle Dressing Gauze Tape IFAK Combat Casualty Evacuation Care Combat Casualty Evacuation Care • Care rendered during transport to higher level care. • First opportunity for additional medical resources (if pre-staged and available during this phase of operation). Evacuation Terminology CASEVAC MEDEVAC Both types of evacuation are included in the new term “Tactical Evacuation” 31 Combat Casualty Evacuation Care • MEDEVAC = transporting casualties via vehicles SPECIFICALLY CONFIGURED, EQUIPPED, AND STAFFED to provide medical care • CASEVAC = moving casualties via NONMEDICAL assets Hypothermia Prevention • Lethal Triad: – Hypothermia – Acidosis – Coagulopathy • Hypothermia Prevention Kit – Blizzard® Wrap – Readi-Heat® Blanket – Thermo-lite Stokes, SKED, Talon II Litters Future Issues • • • • Recombinant factor VIIa Fresh Frozen Plasma Fresh whole blood Ketamine Summary • Addressing Leading Causes of Preventable Deaths may Reduce KIA rate by 15% – #1: Extremity Hemorrhage – #2: Tension Pneumothorax – #3: Airway Occlusion • Cannot Rely on Traditional Measures to Assess Casualty Status – Monitors/BP cuff/stethoscope – Tools Summary • Hemorrhage Control Techniques – Tourniquet – Pressure Dressing – Combat Gauze • Recognize Tension Pneumothorax in Tactical Environment – Penetrating/blunt Chest Wound – Respiratory Distress Summary • CASEVAC First Opportunity for Additional Assets – Oxygen – Blood – Special Equipment – Monitors – Additional Providers Only available if you were in on the Planning and fought for the space Summary • Tactical Casualty Care Requires Aggressive, Full-Contact Measures • MUST Know Equipment Capabilities and Limitations • Adapt to Environment AND situation Conclusion “If during the next war you could do only two things, 1) place a tourniquet and 2) treat a tension pneumothorax, then you can probably save between 70 and 90 percent of all the preventable deaths on the battlefield.” -COL Ron Bellamy Questions?