Hypoxia in a Teen Inpatient
advertisement
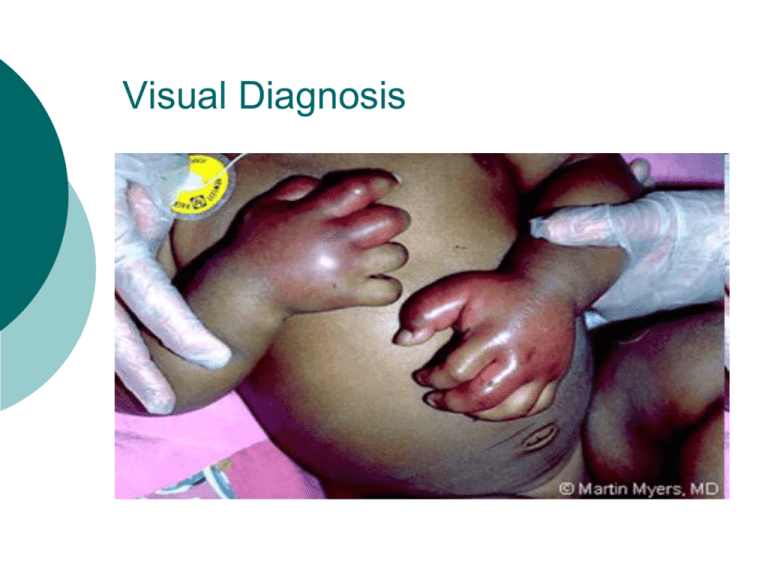
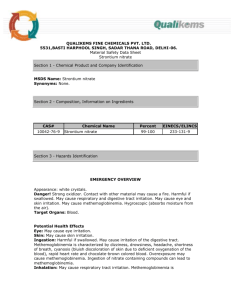
Visual Diagnosis A Hypoxic Teen Inpatient Eva Delgado, MD Morning Report Overview Case Presentation Work-up based on Differential Significance of the Diagnosis Understanding the Presentation Treating the Pathology Take Home Points Case Presentation 16 y/o F with synovial sarcoma in L thigh/hip, metastatic to lungs at diagnosis. Radiation wound complication, transferred to ortho debridement, revision of hip arthroplasty Case Presentation Patient with long course and poor nutrition, so pediatric hospitalist service consulted. Day peds MD ordered NG tube with local anesthetic and CXR to confirm placement. RN calls Night peds MD due to desaturation shortly afterward. Physical Exam VS: RR 12, O2sat 85-90% on 10L NC Gen: No ↑WOB, alert HEENT: No cyanosis Chest: CTA b/l, good aeration CV: RRR, no murmur Ext: wwp, cap refill < 2 sec, New pulse ox trialed, well-placed, with same reading on different digits Work-up to Diagnosis Chart Review: History- tumor burden/growth, medications, hypercoagulability, similar past episodes Labs/Studies: CXR ABG/VBG CBC xxxxxxxxxxxxx xxxxxxxxx xxxxxxxxx CBC: Hbg 8.6, HCT 25 VBG: 7.36/44/53/25 -0.1 MetHb: 40% Diagnosis: Methemoglobinemia CO-Hb: 0.9% A Review of Hemoglobin Hemoglobin = 4 globin chains, 4 heme molecules, each bound to Fe++ Oxygen binds Iron (Fe++) Hemoglobin Methemoglobin Oxidation = loss of 4 electrons from Fe atoms Methemoglobin = 4 globin chains, 4 heme molecules, each bound to Fe+++ **Can’t bind O2 in this form** Significance to Practice MetHb is 2% of normal blood Endogenous enzymes reduce to Hb Methemoglobinemia: Oxidation >2% MetHb Oxyhemoglobin curve Danger: tissue hypoxia *MetHb level 70% fatal Etiologies of Methemoglobinemia Congenital: Deficiency of enzymes that reduce MetHb back to Hb G6PD Deficiency Hb M Disease Diet: Nitrites from nitrate-rich food or from well water oxidation of Hb Etiologies of Methemoglobinemia Meds = most common cause 42% of 138 cases due to Dapsone Local Anesthetics: Prilocaine, Lidocaine, Tetracaine, and… Topical benzocaine most severe ↑MetHb Ifosfamide Bactrim Methylene Blue* Tobias et al, J of Intensive Care Medicine, 2009. Presentation: Clinical No resp distress if MetHb < 20%; +dyspnea > 45% Cyanosis if MetHb > 15-20% Hypoxemia manifested as low oxygen saturation on pulse oximetry SpO2 not responsive to ↑FiO2 Presentation: Serology Chocolate-colored blood ABG with normal or high pO2 AND low O2sat on pulse oximetry “The Saturation Gap” VBG with elevated MetHb level Chung et al.J of Emergency Medicine, 2009. Tobias, J of Intensive Care Medicine, 2009. Pulse Oximetry Measures O2 saturation of Hb Sensor contains infrared (940nm) and red (660nm) wavelengths of light Oxygenated Hb absorbs light at 660nm vs. deoxygenated Hb at 940nm Ratio of wavelengths absorbed gives O2sat Pulse Oximetry and Methemoglobin SpO2 = BLUE SaO2 = RED MetHb absorbs at both wavelengths MetHb < 20% detected by deoxyHb sensor MetHb > 20% detected by oxyHb sensor Newer pulse ox coming with more wavelengths So and Farrington, J Ped Healthcare 2008 Detecting Methemoglobinemia Co-oximetry: Measurement of oxygen concentration in blood using numerous UV light wavelengths Detects oxyHb, deoxyHb, MetHb, carboxyHb Reducing MetHb Physiologic response to MetHb: NADH-dependent MetHb reductase shifts MetHb back to Hb Rate of conversion = 15%/hour Infants have small supply of enzyme Infants and elderly = 50% of Methemoglobinemia cases So and Farrington, J Ped Healthcare 2008 Treating Methemoglobinemia Poison Control! Methylene Blue: Give if symptomatic and MetHb < 20% or if level > 30% Facilitates reduction via NADPH MetHb Reductase NADPH enzyme produced by G6PD* N-acetylcysteine in G6PD Deficiency Back to the Case Patient treated with Methylene Blue Developed chills, rigors, SpO2 70% No intervention, improved – 96% Added Benzocaine and Lidocaine to allergy list (along with Ifosfamide) Risk of recurrence with re-exposure Guay, Anesthesia and Analgesia, 2009. Take Home Points Low SpO2 and lack of response to ↑FiO2 implies abnormal Hb Don’t forget ABG or VBG, and the saturation gap with normal pO2 Beware local/topical anesthetics Review history and meds if unsure Watch for new pulse oximeters!! Works Cited Tobias and Ramachandra, “Intraoperative Diagnosis of Unsuspected Methemoglobinemia Due to Low Pulse Oximetry Values,” Journal of Intensive Care Medicine, July 2009. So and Farrington, “Topical Benzocaine-induced Methemoglobinemia in the Pediatric Population,” Journal of Pediatric Health Care, 2008. Chung et al., “Severe Methemoglobinemia Linked to Gel-Type Topical Benzocaine Use: A Case Report,” Journal of Emergency Medicine, 2009. Guay, “Methemoglobinemia Related to Local Anesthetics: A summary of 242 Episodes,” Anesthesia and Analgesia, 2009. Bong, Hilliard and Seefelder, “Severe Methemoglobinemia from Topical Benzocaine 7.5% (baby orajel) Use for Teething Pain in a Toddler,” Clinical Pediatrics, 2009. Mack, “Focus on Diagnosis: Co-oximetry,” Pediatrics in Review, 2007.