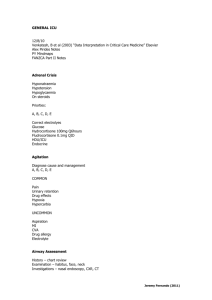
Inhalational Injury
advertisement
Inhalational Injury 16/12/10 SP Notes FANZCA Part II Notes Toon, M. H. et al (2010) “Management of acute smoke inhalational injury” Crit Care Resus, 12:pages 53-61 - 20% in burn patients - 60% in burns patients with central facial burns - causes a massive increase in mortality PATHOPHYSIOLOGY Components of smoke that cause damage: - heat particulates systemic toxins (CO and CN) respiratory irritants (ammonia, HCl, oxides of nitrogen, phosgene and aldehydes) Thermal Injury - oropharyngeal area - lower airway affected if steam, volatile gases, explosive gasses or hot liquids are inhaled Asphyxiation - combustion utilises O2 -> low FiO2 -> hypoxaemia - CO: tissue hypoxia, left shifted ODC, cytochrome oxidase binding, myocardial myoglobin binding with decreased contractility - CN: poisoning of electron transport chain -> lactic acidosis - MetHb: heat denaturation of Hb, oxides produced in fire, nitrites -> decreased O2 carrying capacity Pulmonary Irritation - direct tissue injury acute bronchospasm activation of inflammatory cascade oxygen radical and proteolytic enzymes mucosal damage bronchitis mucus plugging pulmonary oedema bronchospasm bronchorrhoea hypoxaemia/raised A-a gradient SIRS Jeremy Fernando (2011) CLINICAL FEATURES - events: enclosed space, explosion, LOC, toxic gases, did you breathe fire, voice changes - burns in face, especially around mouth/nose - singed nasal hair - carbonaceous sputum - nasal deposits - soot, charring, mucosal erythema/oedema/blistering/necrosis - voice changes/hoarseness - respiratory distress: hypoxaemia, raised A-a gradient, stridor, wheeze, tachypnoea, dyspnoea - high CO levels – might look ‘cherry red’ - CN: bitter almond odour - CO and CN toxicity: lactic acidosis, high SvO2, mental confusion, hypotension INVESTIGATIONS - CXR: diffuse atelectasis, pulmonary oedema, bronchopneumonia (not reliable investigation however) MANAGEMENT Prehospital - minimise exposure time - high flow O2 Inhospital Airway - proportional to severity acutely compromised airway: RSI, smaller ETT +/- surgical airway less severe: RSI or AFOI not compromised: nasal endoscopy, have low threshold for elective intubation leave tube uncut tie tube firmly (wire to teeth) elevate head (decreases oedema) adrenaline and steroids (controversial) Breathing - high flow O2 for 6 hours and until CO levels return to normal - bronchospasm: B2 agonists (multiple benefits – bronchodilation, anti-inflammatory, improves airspace fluid clearance and stimulates mucosal repair) - humidification - NAC and heparin nebulisers (5000U heparin + 3mL of 20% NAC Q4 hrly for 7 days reduced reintubation and mortality in children) - aggressive toileting - suction - cultures - protective lung ventilation strategy: low volume, high PEEP, permissive hypercapnia Jeremy Fernando (2011) - HFOV - ECMO Circulation - no good data tendency to avoid increased fluids should be guided by urine output and haemodynamic parameters use dynamics parameters (pulse pressure variation, fluid responsiveness) early albumin after 24 hours Carbon Monoxide Toxicity - 100% oxygen - rapid transport to a hyperbaric centre Cyanide Toxicity - sodium thiosulphate -> produces metHb which can bind CN and allows metabolism by liver enzymes - hydroxocobalamin (vitamin B12) -> actively binds CN and allows renal elimination Other Experimental Therapies - nebulised heparin + antithrombin high dose IV heparin IV tPA anti-inflammatories NO inhibitors antioxidants (nebulized vitamin E) methylprednisolone phenytoin (for anti-inflammatory properties) endothelin-1 receptor antagonist (tezosentan) nebulized deferoxamine + pentastarch complex APC decontamination of lungs with amphorteric, hypertonic chelating agents Jeremy Fernando (2011)