Surgical_Treatment_of_Ulcers
advertisement

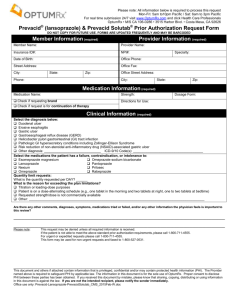
Surgical Treatment of Ulcers Anatomy Introduction Number of admissions for uncomplicated disease is falling Incidence of complications related to NSAID use is increasing Incidence has declined by 50% in last 25 years Surgical intervention is rare now for elective treatment Medical Treatment Biaxin 500 BID and Amoxacillin 1g BID plus Prilosec BID all for 2 weeks. Flagyl 250 QID and Tetracyclin 500 QID and Prilosec BID all for 2 weeks. 80% heal over 6 weeks. 80% recur after 1 year if H.Pylori not treated at same time. Bleeding Ulcer Laser Coagulation of Bleeding Ulcer Coil Embolization of Bleeding Ulcer Pyloroplasty for Bleeding Ulcer Indications For Surgery Bleeding Perforation Obstruction Intractability Surgical treatment is aimed at reduction of acid production one way or another Cure with lowest risk of complications History of Peptic Ulcer Surgery Harberer 1882- first gastric resection for ulcer Billroth 1885- Billroth II gastrectomy Hofmeister 1896- Retrocolic anastamosis Dragstedt 1943- Truncal vagotomy Visick 1948- vagotomy and drainage Johnson 1970- highly selective vagotomy Open Surgical Procedures Truncal vagotomy and pyloroplasty Truncal vagotomy and gastrojejunostomy Truncal vagotomy and antrectomy Highly selective vagotomy Billroth I Gastrectomy Originally described for resection of distal gastric ulcers. Still used in gastric cancers if radical gastrectomy is inappropriate. Later applied in treatment of benign ulcers. Useful for ulcers high on lesser curve, or bleeding ulcer that needs resection. Antrectomy and Truncal Vagotomy with BI Billroth II Gastrectomy Initially described for duodenal ulcers. Some form of vagotomy is treatment of choice for uncomplicated DU. Ulcer heals after surgery. Useful in recurrent ulcers following previous vagotomy. Antecolic vs retrocolic. Antecolic and Retrocolic BII Truncal Vagotomy Resect 1-2cm of each vagal trunk on distal esophagus. Reduces acid by 80%. Denervates parietal cells, antral pump, pyloric sphincter mechanism. Delays gastric emptying, so need drainage. With pyloroplasty recurrence 3-10% With pyloroplasty morbidity 1-2% Pyloroplasty for Bleeding Ulcer Pyloroplasty and Oversew of Ulcer Truncal Vagotomy and Antrectomy Entails distal gastrectomy of 50-60% of stomach. Removes parietal cell mass. Requires a BI or BII reconstruction. Recurrence rate 0.6-4% Morbidity rate 0.9-1.6% Selective Vagotomy Total denervation of the stomach from diaphragmatic crus to pylorus. Procedure still needs drainage, but advantage is other organs are spared, liver, gallbladder, small bowel, colon. Highly Selective Vagotomy Spares nerves of Latarjet, but divides vagal branches to proximal 2/3 of stomach. Antral innervation is thus preserved, gastric emptying preserved, so drainage procedure unnecessary. Recurrence rate 10-15% Lowest morbidity of all Types of Vagotomies Post Gastrectomy Complications Gastric atony 50% Alkaline gastritis Recurrent ulcers 2% Diarrhea 16% Dumping 14% Bilious vomit 10% Anemia 12% B12 deficiency 14% Folate deficiency 32% Roux -en -Y Reconstruction Post Vagotomy Complications Diarrhea 2% Dumping 2% Bilious vomiting <2% Penetrating Gastric Ulcer