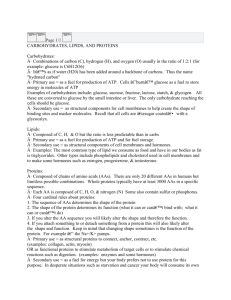
biochem ch 37 [2-9
advertisement

BC Chap 37 Protein Digestion and Amino Acid Absorption Proteolytic enzymes (proteases) break down dietary proteins into their constituent AAs in stomach and intestine o Many synthesized as zymogens In stomach, pepsin begins digestion of proteins by hydrolyzing them to smaller polypeptides In small intestine, pancreatic proteases (trypsin, chymotrypsin, elastase, and carboxypeptidases) cleave polypeptides into oligopeptides and AAs o Further cleavage of oligopeptides to AAs accomplished by enzymes produced by intestinal epithelial cells; enzymes include aminopeptidases located on brush border and other peptidases located within the cells o AAs produced by protein digestion absorbed through intestinal epithelial cells and enter blood Large number of overlapping transport systems exist for AAs in cells o Some systems contain facilitative transporters, whereas others express sodium-linked transporters, which allow active transport of amino acids into cells Proteins continually synthesized and degraded (turnover) in cells o Lysosomal proteases (cathepsins) degrade proteins that enter lysosomes o Cytoplasmic proteins targeted for turnover covalently linked to small protein ubiquitin, which then interacts with large protein complex (proteasome) to degrade protein in ATP-dependent process Protein Digestion Digestion of protein begins in stomach and is completed in intestine No single enzyme can completely digest a protein; by acting in concert, they can digest dietary proteins to AAs and small peptides, which are cleaved by peptidases associated with intestinal epithelial cells Pepsinogen secreted by chief cells of stomach, and gastric parietal cells secrete HCl o Acid in stomach lumen alters conformation of pepsinogen so it can cleave itself to pepsin Dietary proteins denatured by acid in stomach; inactivates proteins and partially unfolds them so they are better substrates for proteases o At low pH of stomach, pepsin not denatured and acts as endopeptidase, cleaving peptide bonds at various points within protein chain o Although pepsin has fairly broad specificity, it tends to cleave peptide bonds in which carboxyl group provided by aromatic or acidic AA o Cleavage produces smaller peptides and some free AAs Kwashiorkor – caused by deficiency of protein in diet that is adequate in calories o Patients suffer muscle wasting and decreased concentration of plasma proteins, particularly albumin o Result is increase in interstitial fluid that causes edema and distended abdomen o Muscle wasting caused by lack of essential AAs in diet; existing proteins must be broken down to produce AAs for new protein synthesis o Problems may be compounded by decreased ability to produce digestive enzymes and new intestinal epithelial cells because of decreased availability of AAs for synthesis of new proteins In small intestine, pancreas secretes bicarbonate, which raises pH so pancreatic proteases can be active o Because active forms of pancreatic enzymes can digest each other, it is important for their zymogen forms all to be activated within a short span of time; accomplished by cleavage of trypsinogen to trypsin, which then cleaves the other pancreatic zymogens o Trypsinogen cleaved to trypsin by enteropeptidase (a protease) secreted by brush border cells of small intestine Trypsin catalyzes cleavages that convert chymotrypsinogen to chymotrypsin, proelastase to elastase, and procarboxypeptidases to carboxypeptidases Trypsin cleaves dietary proteins as well o Trypsin, chymotrypsin, and elastase are serine proteases that act as endopeptidases Trypsin is most specific of enzymes, cleaving peptide bonds in which carboxyl (carbonyl) group provided by lysing or arginine Chymotrypsin favors residues that contain hydrophobic AAs Elastase cleaves elastin, and proteins at bonds that carboxyl group is contributed by AAs with small side chains (alanine, glycine, and serine) o Smaller peptides formed by action of trypsin, chymotrypsin, and elastase attacked by exopeptidases (proteases that cleave one AA at a time from end of chain) Procarboxypeptidases (zymogens produced by pancreas) converted by trypsin to active carboxypeptidases that remove AAs from carboxyl ends of peptide chains Carboxypeptidase A preferentially releases hydrophobic AAs, and carboxypeptidase B releases basic AAs (arginine and lysine) Elastase also found in neutrophils; neutrophils frequently act in lung, and elastase sometimes released into lung as neutrophils work o In normal individuals, released elastase blocked from destroying lung cells by action of circulating α-1antitrypsin (protease inhibitor) that is synthesized and secreted by liver o Certain individuals have genetic mutation that leads to production of inactive α-1-antitrypsin protein (α1-antitrypsin deficiency) Lack of α-1-antitrypsin leads to development of emphysema caused by proteolytic destruction of lung cells, which results in reduction in expansion/contraction capability of lungs o Deficiency of α-1-antitrypsin can be measured using dried blood spot – blood solubilized using buffer and various amounts of blood sample incubated with antibodies specific for α-1-antitrypsin Antibody-antigen complexes disperse light, and extent of light scattering proportional to concentration of α-1-antitrypsin in solution Procedure called rate nephelometry Obtaining blood from finger prick and allowing blood to dry on card enables rapid screening of individuals with this disorder Exopeptidases produced by intestinal epithelial cells act within brush border and within cell Aminopeptidases located on brush border cleave one AA at a time from amino end of peptides Intracellular peptides act on small peptides that are absorbed by cells Concerted action of proteolytic enzymes produced by cells of stomach, pancreas, and intestine cleaves dietary proteins to AAs Digestive enzymes digest themselves as well as dietary protein and can digest intestinal cells that are regularly sloughed off into lumen o Sloughed cells replaed by cells that mature from precursor cells in duodenal crypts o Amount of protein digested and absorbed each day from digestive juices and cells released into intestinal lumen may be equal to or greater than amount of protein consumed in diet Pancreas synthesizes and stores zymogens in secretory granules; pancreas also synthesizes secretory trypsin inhibitor to block any trypsin activity that may occur from accidental trypsinogen activation o If inhibitor not present, trypsinogen activation would lead to activation of all the zymogens in the pancreas, which would lead to digestion of intracellular pancreatic proteins o Multiple episodes of this can lead to pancreatitis Absorption of Amino Acids AAs absorbed from intestinal lumen through secondary active Na+-dependent transport systems and through facilitated diffusion Patients with cystic fibrosis have genetically determined defect in function of Cl- channels o In pancreatic secretory ducts, which carry pancreatic enzymes into lumen of small intestine, this defect causes inspissation (drying and thickening) of pancreatic exocrine secretions, leading eventually to obstruction of these ducts o One problem is inability of pancreatic enzymes to enter intestinal lumen to digest dietary proteins AAs absorbed from lumen of small intestine principally by semispecific Na+-dependent transport proteins in luminal membrane of intestinal cell brush border o Cotransport of Na+ and AA from outside apical membrane to inside cell driven by low intracellular Na+ concentration; low intracellular Na+ results from pumping Na+ out of cell by Na+/K+/ATPase on serosal membrane; primary transport mechanism is creation of sodium gradient; secondary transport process is coupling of AAs to influx of sodium Allows cells to concentrate AAs from intestinal lumen AAs then transported out of cell into interstitial fluid principally by facilitated transporters in serosal membrane o At least 6 different Na+-dependent AA carriers located in apical brush border membrane of epithelial cells; carriers have overlapping specificity for different AAs One carrier preferentially transports neutral amino acids, another transports proline and hydroxyproline, the third transports acidic AAs, fourth basic AAs (lysine, arginine, and urea-cycle intermediate ornithine) and cystine (2 cysteine residues linked by disulfide bond) Some AAs transported across luminal membrane by facilitated transport carriers Most AAs transported by more than one transport system + Na -dependent carriers also present in renal epithelium o Different isozymes present in PMs of other tissues o Facilitated transport carriers in serosal membrane of intestinal epithelia similar to those found in other cell types in body o During starvation, intestinal epithelia take up AAs from blood to use as energy source; AA transport across serosal membrane is bidirectional Hartnup disease – genetically determined, relatively rare autosomal recessive disorder caused by defect in transport of neutral AAs across both intestinal and renal epithelial cells (system B0, gene SLC6A19) o SLC refers to solute carrier family of transport proteins (of which there are 55) with a total of 362 genes o Signs and symptoms caused in part by deficiency of essential AAs o Cystinuria (system B0,+, genes involved are SLC7A9 and SLC3A1, as transporter is heteromeric complex) and Hartnup disease involve defects in 2 different transport proteins In each case, defect present both in intestinal cells, causing malabsorption of AAs from digestive products in intestinal lumen, and in kidney tubular cells, causing decreased resorption of AAs from glomerular filtrate and increased concentration of AAs in urine o Patients with cystinuria and Hartnup disease do not absorb affected AAs at normal rate from digestive products in intestinal lumen and don’t readily resorb AAs from glomerular filtrate into blood Normally only a few percentage of AAs that enter glomerular filtrate excreted in urine; most are resorbed; in these diseases, much larger amounts of affected AAs excreted in urine, resulting in hyperaminoaciduria o Patients with cystinuria have genetically determined defect in transport of cystine and basic AAs (lysine, arginine, and ornithine) across brush border membranes of cells in both small intestine and renal tubules (system B0,+) Patients don’t have symptoms of AA deficiency, in part because AAs cysteine (which is oxidized in blood and urine to form disulfide cystine) and arginine can be synthesized in body Ornithine can also be synthesized Most serious problem for these patients is insolubility of cystine, which can form kidney stones that may lodge in ureter, causing genitourinary bleeding and severe pain (renal colic) AAs that enter blood transported across PMs of various tissues principally by Na+-dependent cotransporters and, to lesser extent, by facilitated transporters o Na+ dependence of AA transport in liver, muscle, and other tissues allows them to concentrate AAs from blood; transport proteins have different genetic bases, AA compositions, and somewhat different specificities than those in luminal membrane of intestinal epithelia o N-system for glutamine uptake present in liver but either is not present in other tissues or is present as isoform with different properties o There is some overlap in specificity of transport proteins, with most AAs being transported by more than one carrier Trace amounts of polypeptides pass into blood; may be transported through intestinal epithelial cells, probably by pinocytosis, or they may slip between cells that line gut wall o This process troublesome for premature infants because it can lead to allergies caused by proteins in their food Protein Turnover and Replenishment of Intracellular Amino Acid Pool AA pool within cells generated both from dietary AAs and from degradation of existing proteins within cell o All proteins in cells have half-life (t1/2); some proteins inherently short-lived, with half-lives of 5-20 minutes, while others have half-lives of many hours to days o Proteins continuously being synthesized and degraded in body, using variety of enzyme systems to do so Proteins that undergo extensive synthesis and degradation are hemoglobin, muscle proteins, digestive enzymes, and proteins of cells sloughed off from GI tract o Hgb produced in reticulocytes and reconverted to AAs by phagocytic cells that remove mature RBCs from circulation on daily basis o Muscle protein degraded during periods of fasting, and AAs used for gluconeogenesis After ingestion of protein in diet, muscle protein resynthesized Adults cannot increase amount of muscle or other body proteins by eating excess amount; if dietary protein consumed in excess of our needs, it is converted to glycogen and triacylglycerols, which are then stored Large amount of protein recycled daily in form of digestive enzymes, which are themselves degraded by digestive proteases About ¼ of cells lining walls of GI tract lost each day and replaced by newly synthesized cells; as cells leave GI wall, their proteins and other components digested by enzymes in lumen of gut, and products absorbed RBCs have life span of 120 days; Hgb in these cells degraded to AAs by lysosomal proteases, and AAs reused in synthesis of new proteins Only about 6% of protein that enters digestive tract (including dietary proteins, digestive enzymes, and proteins in sloughed-off cells) excreted in feces each day; remainder recycled Proteins recycled within cells; differences in AA composition of various proteins of body, vast range of turnover times, and recycling of AAs important factors that help determine requirements of specific AAs and total protein in diet Intracellular proteins damaged by oxidation and other modifications that limit their function o Mechanisms for intracellular degradation of unnecessary or damaged proteins involve lysosomes and ubiquitin/proteasome system Lysosomes participate in autophagy, in which intracellular components surrounded by membranes that fuse with lysosomes and endocytosis o Autophagy – complex regulated process in which cytoplasm sequestered into vesicles and delivered to lysosomes o In lysosomes, cathepsin family of proteases degrades ingested proteins to individual AAs o Recycled AAs can leave lysosome and rejoin intracellular AA pool o Can be triggered by starvation of cell – allows old proteins to be recycled and newly released AAs to be used for new protein synthesis to enable cell to survive starvation conditions mTOR plays key role in regulating autophagy Ubiquitin – small protein that is highly conserved; targets intracellular proteins for degradation by covalently binding to ε-amino group of lysine residues (accomplished by 3-enzyme system that adds ubiquitin to proteins targeted for degradation) o Often, target protein is polyubiquitinylated (additional ubiquitin molecules added to previous ubiquitin molecules, forming long ubiquitin tail on target protein) o After polyubiquitinylation complete, targeted protein released from 3-enzyme complex and directed to proteasome via variety of mechanisms Proteasome – protease complex that degrades targeted protein, releasing intact ubiquitin that can again mark other proteins for degradation o Basic proteasome is cylindrical 20S protein complex with multiple internal proteolytic sites; ATP hydrolysis used both to unfold tagged protein and to push protein into core of cylinder of proteasome o Complex regulated by 19S regulatory particles (cap complexes), which bind ubiquinylated protein (requires ATP) and deliver them to complex o After target protein degraded, ubiquitin released intact and recycled o Resulting AAs join intracellular pool of free AAs Many proteins that contain regions rich in AAs proline (P), glutamate (E), serine (S), and threonine (T) have short half-lives; regions are known as PEST sequences o Most of proteins that contain PEST sequences are hydrolyzed by ubiquitin-proteasome system γ-Glutamyl Cycle γ-glutamyl cycle necessary for synthesis of glutathione (compound that protects cells from oxidative damage) Can salvage cysteine Enzymes of cycle present in many tissues, although certain tissues lack one or more of enzymes of cycle Extracellular AA reacts with glutathione (γ-glutamyl-cysteinyl-glycine) in reaction catalyzed by transpeptidase present in PM; γ-glutamyl AA formed, which travels across PM and releases AA into cell o Other products of the two reactions reconverted to glutathione Reactions that convert glutamate to glutathione in γ-glutamyl cycle are same reactions as those required for synthesis of glutathione o Enzymes for glutathione synthesis (except transpeptidase) found in most tissues o Oxoprolinase missing from many tissues, so major role of this pathway is one of glutathione synthesis from glutamate, cysteine, and glycine o Transpeptidase is only protease in cell that can break γ-glutamyl linkage in glutathione Glutathione also involved in reducing compounds such as H2O2; protects cells, particularly erythrocytes, from oxidative damage through formation of oxidized glutathione (2 glutathione residues connected by disulfide bond)