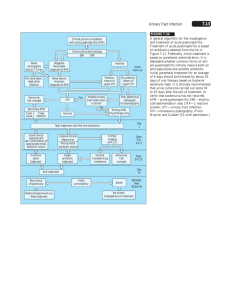
Complicated Pyelonephritis

Surgical
Complications of
Pyelonephritis
Carly Thompson
MD, CCFP, EM Resident
January 15, 2009
Case
Patient: 56 yo female
PMHx: Previously healthy
CC: Fever, L flank pain
O/E: HR 98, Temp 38.0C, BP 118/58
Appears slightly obese
Left CVA tenderness
Labs:
Labs: Elevated WBC 17.8, glucose 12.0, Cr 100
Urine: Many WBC on R+M
What would you like to do next?
Identify:
Black arrow?
White arrows?
Star?
Grayson DE et al. Emphysematous infections of the abdomen and pelvis: a pictorial review. Radiographics. 2002;22:543-561.
Grayson DE et al. Emphysematous infections of the abdomen and pelvis: a pictorial review. Radiographics. 2002;22:543-561.
Grayson DE et al. Emphysematous infections of the abdomen and pelvis: a pictorial review. Radiographics. 2002;22:543-561.
Identify:
White arrow?
Star?
Diagnosis?
Emphysematous pyelonephritis with obstruction by calculus.
Due to your astute diagnosis the patient received appropriate antibiotics, was treated with percutaneous drainage, and was discharged home on day 10 with a new diagnosis of diabetes and chronic renal failure.
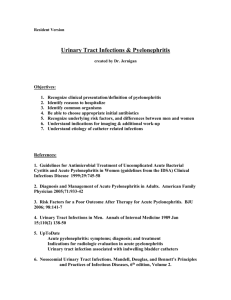
Objectives:
When Pyelonephritis Goes Bad . . .
Emphysematous Pyelonephritis
Definition and Diagnosis
Risk Factors, Clinical Features
Pathogenesis, Pathology
Diagnosis: Imaging and Classification
Treatment and Complications
Renal and Perinephric Abscesses
Pyonephrosis
Xanthogranulomatous Pyelonephritis
Definition:
Emphysematous Pyelonephritis
EPN: Rare, life-threatening necrotizing infection of the kidney characterized by accumulation of gas
May occur anywhere!
Emphysematous pyelonephritis = kidney
Emphysematous pyelitis = collecting duct
Emphysematous ureteritis = ureteral wall
Emphysematous cystitis = bladder wall
Diagnosis
1898 – First case report JAMA.
1 Pt with pneumaturia.
1962 – Term emphysematous pyelonephritis coined.
2
Diagnosis for study purposes: 3
Symptoms of upper UTI or fever with positive urine culture or pyuria without other identified infectious foci
Radiologic evidence of gas in the collecting system, renal parenchyma or perinephric or pararenal space.
No fistula between urinary tract and bowel, no recent trauma, urinary catheter insertion or drainage.
(1) Kelly HA, MacCallum WG. Pneumaturia. JAMA. 1898;31:375.
(2) Schultz EH, Klorfein EH. Emphysematous pyelonephritis. J Urol. 1962;87:762.
(3) Huang JJ, Tseng CC. Emphysematous pyelonephritis: Clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern
Med. 2000;160:797-805
.
Risk Factors
Risk Factors 1
Diabetes: 96% of patients
Female 80% (Female to male ratio 4:1)
Left kidney 56%, bilateral 3%
Urinary tract obstruction 29%, stone 24%
Mean age 55-60 years 2
Poor diabetes control with HbA1c >0.08 in 72% 3
(1) Somani et al. Is percutaneous drainage the new gold standard in the management of emphysematous pyelonephritis? Evidence from a systematic review. J Urol. 2008;179:1844-1849.
(2) Falagas ME, Alexiou VG, Giannopoulou KP, Siempos II. Risk factors for mortality in patients with emphysematous pyelonephritis. J Urol.
2007;178:880-885.
(3) Huang JJ, Tseng CC. Emphysematous pyelonephritis: Clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern
Med. 2000;160:797-805.
Clinical Features
Usual Triad of Upper Urinary Tract Infection 1
Fever 79%
Flank, abdominal or back pain 71%
Pyuria 79%
Symptoms – acute or chronic presentation!
Nausea, vomiting 8%
Dyspnea 6%
Change in level of consciousness 9%
Signs
Shock 29%
Rash?
2
(1) Huang JJ, Tseng CC. Emphysematous pyelonephritis: Clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern
Med. 2000;160:797-805.
(2) Sun JT, Tsai MT. emphysematous pyelonephritis with flank rash. Q J Med [serial online]. 2008;Nov 16. Available at: http://qjmed.oxfordjournals.org/cgi/reprint/hcn145v2 . Accessed January 11, 2009.
Clinical Features
Laboratory Data: 1
Leukocytosis: WBC >12 x 10 9 – 67%
Thrombocytopenia: Platelets <120 x 10 9 – 46%
Urinalysis: 1
Pyuria 79%
Macrohematuria (RBC > 100/hpf) – 13%
Severe proteinuria >3g/L – 21%
(1) Huang JJ, Tseng CC. Emphysematous pyelonephritis: Clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern
Med. 2000;160:797-805.
Pathogenesis: Bugs
Urine Culture: 1
Escherichia coli – 67%
Klebsiella 20%
Other: Usually proteus and pseudomonas 10%
No growth 4%
Reported Bugs: 2
Polymicrobial infections: Strep and staph
Rare: Bacteriodes fragilis, Clostriduium, Cryptococcus,
Pneumocystis carinii.
Superinfectcion: Candida
(1) Somani et al. Is percutaneous drainage the new gold standard in the management of emphysematous pyelonephritis? Evidence from a systematic review. J Urol. 2008;179:1844-1849.
(2) Tang HJ et al. Clinical characteristics of emphysematous pyelonephritis. J Microbiol Immunol Infect. 2001;34:125-130.
Pathogenesis
1
(1) High level of tissue glucose
(2) Presence of glucose-fermenting bacteria
(3) Impaired vascular supply and decreased tissue perfusion
(4) Impaired host immunity and / or
(5) Obstruction of the urinary tract in non-DM patients
(1) Tseng CC, Wu JJ, Wang MC, Hor LI, Ko YH, Huang JJ. Host and bacterial virulence factors predisposing to emphysematous pyelonephritis. Am J
Kidney Dis. 2005;46:432-439.
Virulence Factors
Tseng et al. (2005) 1
Host Factors for EPN
Poor glycemic control HbA1c >11%
(OR 4.9 p=0.018)
Less urinary tract instrumentationrelated infection (0% vs 6%) (p=0.09)
Bacterial virulence factors
EPN – increased uropathogenic specific protein (usp) gene (OR 8.4 p=0.057)
EPN – less PapG II Adhesion gene (OR 0.2 p=0.01)
(1) Tseng CC, Wu JJ, Wang MC, Hor LI, Ko YH, Huang JJ. Host and bacterial virulence factors predisposing to emphysematous pyelonephritis. Am J
Kidney Dis. 2005;46:432-439.
Pathology
(1) Cut specimen reveals diffuse parenchymal necrosis.
(2) Cut specimen with many parenchymal abscesses filled with purulent exudate.
(1) Grayson DE et al. Emphysematous infections of the abdomen and pelvis: a pictorial review. Radiographics. 2002;22:543-561.
Diagnosis:
When should you think of EPN?
1
DM
Female
Signs of upper urinary tract infection
Sepsis
Poor of glycemic control
Elevated serum creatinine or low platelets
Poor response to Abx
(1) Chen MT et al. Percutaneous drainage in the treatment of emphysematous pyelonephritis: 10-year experience. J Urol. 1997;157:1569-1573.
Diff Dx of Gas in Urinary Tract
1
Incidental / Iatrogenic – catheter
Recent instrumentation / surgery
Diagnostic procedures: i.e. cystoscopy
Therapeutic procedures: i.e. transuretheral tumour resection, embolization of feeding arteries of a tumour
Ileal Conduit
Post-ureterosigmoidostomy
Fistulous connection with hollow viscus
Penetrating trauma or blunt trauma
(1) Portnoy et al. Gas in the kidney: CT findings. Emerg Radiol. 2007:14:83-87.
Plain Film / KUB
May see crescent-shaped collection of gas over the upper pole of kidney 1
Low-sensitivity – Study by Michaeli et al (1984) 2
Gas on 33% of plain abdominal films
May be difficult to distinguish necrotic gas-filled area from gas in bowel
(1) Lee C, Henderson SO. Emergent surgical complications of genitourinary infections. Emerg Med Clin N Am. 2003;21:1057-1074.
(2) Michaeli J, Mogle P, Perlberg S, Hemiman S, Caine M. Emphysematous pyelonephritis. J Urol. 1984;131:203-208.
(3) Grayson DE et al. Emphysematous infections of the abdomen and pelvis: a pictorial review. Radiographics. 2002;22:543-561.
Intravenous Pyelogram
Most cost-effective
Can demonstrate calculus or papillary necrosis
Low sensitivity for emphysema
Inappropriate for most patients: dehydrated, ill diabetic patients with poor renal function.
(1) Lee C, Henderson SO. Emergent surgical complications of genitourinary infections. Emerg Med Clin N Am. 2003;21:1057-1074.
(2) Nayeemuddin M et al. Emphysematous pyelonephritis. Nat Clin Pract Urol. 2005;2:108–112.
Ultrasound
Accessible and cost-effective without radiation.
Useful for evaluating hydronephrosis or pyonephrosis.
Limited by body habitus.
Less sensitive than CT.
1
(1) Demertzis J, Menias CO. State of the art: imaging of renal infections. Emerg Radiol. 2007;14:13-22.
(2) Grayson DE et al. Emphysematous infections of the abdomen and pelvis: a pictorial review. Radiographics. 2002;22:543-561.
CT Scan
Increased cost, radiation, contrast.
Preferred modality: 1, 2
Assesses extent of involvement
IV contrast can provide information about function
100% sensitive in largest systematic review 3
(1) Lee C, Henderson SO. Emergent surgical complications of genitourinary infections. Emerg Med Clin N Am. 2003;21:1057-1074.
(2) Demertzis J, Menias CO. State of the art: imaging of renal infections. Emerg Radiol. 2007;14:13-22.
(3) Somani et al. Is percutaneous drainage the new gold standard in the management of emphysematous pyelonephritis? Evidence from a systematic review. J Urol. 2008;179:1844-1849.
Day 1: Admission Day
Portnoy et al. Gas in the kidney: CT findings. Emerg Radiol. 2007:14:83-87.
Day 2: Post-Admission
Portnoy et al. Gas in the kidney: CT findings. Emerg Radiol. 2007:14:83-87.
Day 3
Portnoy et al. Gas in the kidney: CT findings. Emerg Radiol. 2007:14:83-87.
Classification
Wan (1996) 1 – Classification based on findings on plain film,
US or CT
Type 1
Parenchymal destruction with either an absence of fluid collection or a presence of streaky or mottled gas
Associated with increased mortality (OR 2.53), a more fulminant course, and shorter interval from onset to death 1,2
Type 2
Either renal or perinephric fluid collection with bubbly or loculated gas or gas in the collecting system
(1) Wan YL, Lee TY, Bullard MJ, Tsai CC. Acute gas-producing bacterial renal infection: correlation between imaging findings and clinical outcome.
Radiology. 1996;198:433-438.
(2) Somani et al. Is percutaneous drainage the new gold standard in the management of emphysematous pyelonephritis? Evidence from a systematic review. J Urol. 2008;179:1844-1849.
Type 1
(A) (B)
(1) Wan YL, Lee TY, Bullard MJ, Tsai CC. Acute gas-producing bacterial renal infection: correlation between imaging findings and clinical outcome.
Radiology. 1996;198:433-438.
CT Scan of Type 1
(1) Wan YL, Lee TY, Bullard MJ, Tsai CC. Acute gas-producing bacterial renal infection: correlation between imaging findings and clinical outcome.
Radiology. 1996;198:433-438.
Type 2
(1) Crescent-shaped and loculated gas.
(2) Shows low-attenuation areas and subcapsular abscess with bubbly fluid.
(1) Wan YL, Lee TY, Bullard MJ, Tsai CC. Acute gas-producing bacterial renal infection: correlation between imaging findings and clinical outcome.
Radiology. 1996;198:433-438.
Classification
Huang and Tseng (2000) 1 – Classification based on
CT findings of extent of gas invasion.
Class 1: Gas in collecting system
Mortality
0%
Class 2: Gas in renal parenchyma.
Class 3A: Gas in perinephric space.
Class 3B: Gas in pararenal space.
Class 4: Bilateral or solitary kidney.
10%
29%
19%
50%
(1) Huang JJ, Tseng CC. Emphysematous pyelonephritis: Clinicoradiological classification, management, prognosis, and pathogenesis. Arch
Intern
Med. 2000;160:797-805.
Class 1
(1) Huang JJ, Tseng CC. Emphysematous pyelonephritis: Clinicoradiological classification, management, prognosis, and pathogenesis. Arch
Intern
Med. 2000;160:797-805.
Class 2
(1) Huang JJ, Tseng CC. Emphysematous pyelonephritis: Clinicoradiological classification, management, prognosis, and pathogenesis. Arch
Intern
Med. 2000;160:797-805.
Class 3
Class 3A: Class 3B:
Perinephric Involvement Pararenal Involvement
(1) Huang JJ, Tseng CC. Emphysematous pyelonephritis: Clinicoradiological classification, management, prognosis, and pathogenesis. Arch
Intern
Med. 2000;160:797-805.
Class 4
Bilateral emphysematous pyelonephritis in a patient with autosomal dominant polycystic kidney disease.
(1) Huang JJ, Tseng CC. Emphysematous pyelonephritis: Clinicoradiological classification, management, prognosis, and pathogenesis. Arch
Intern
Med. 2000;160:797-805.
Treatment: Mortality
Falagas (2007): Meta-analysis
Mortality 25% (Range 11-42%)
Increased Mortality:
Conservative treatment
Bilateral EPN
Type 1
Thrombocytopenia
Not Associated:
Diabetes
OR 2.85 (1.19-6.81)
OR 5.36 (1.41-20.33)
OR 2.53 (1.13-5.65)
OR 22.68 (4.4-116.32)
OR 0.32 (0.05-1.99)
(1) Falagas ME, Alexiou VG, Giannopoulou KP, Siempos II. Risk factors for mortality in patients with emphysematous pyelonephritis. J Urol.
2007;178:880-885.
Treatment: Basics
Hospitalization, ICU admission?
Fluid and electrolyte correction
Appropriate antimicrobials
Treatment of diabetes: Blood sugar control
Relieve obstruction of affected kidney if present
Establish function of other kidney
(1) Somani et al. Is percutaneous drainage the new gold standard in the management of emphysematous pyelonephritis? Evidence from a systematic review. J Urol. 2008;179:1844-1849.
Treatment: Antimicrobials
Canadian Guideline 1:
Individualization of treatment
Reported high rates of clinical and microbiologic cure for complicated UTI with:
Aminoglycosides
Fluoroquinolones
Piperacillin/tazobactam
Ceftazidime
Carbapenems
Length: 7 days for lower tract infection and longer course for patients with severe presentations manifested by fever, bacteremia or hypotension of
10-14 days
Length: Severe presentation – 10-14 days of antibiotics
Replace chronic indwelling catheter before initiating Abx
(1) Nicolle LE, AMMI Canada Guidelines Committee. Complicated urinary tract infection. Can J Infect Dis Med Microbiol. 2005;16:349-360.
Treatment: Surgical
Somani (2008): Systematic review
Mortality
Medical management alone
Medical management + emergency nephrectomy
50%
25%
Medical management with percutaneous drainage 13.5% (p<0.001)
Medical management + PCD + elective nephrectomy 6.6%
Conclusion: Fluid resuscitation, aggressive antibiotics, correction of precipitating factors and early percutaneous drainage +/- elective nephrectomy when indicated gives best outcomes.
(1) Somani et al. Is percutaneous drainage the new gold standard in the management of emphysematous pyelonephritis? Evidence from a systematic review. J Urol. 2008;179:1844-1849.
Complications
Sequelae
Sepsis, Death
Failure to respond to medical treatment or PCD
Relapse 1
Extension of Infection
Lung: Pneumonia, Empyema, Pneumomediastinum
Bone: Osteomyelitis of thoracic spine
Vessels: Pseudoaneurysm of abdominal aorta
Liver: Gas in the hepatic veins
Spleen: Splenic infarction
Skin: Necrotizing fasciitis
(1) Tang HJ et al. Clinical characteristics of emphysematous pyelonephritis. J Microbiol Immunol Infect. 2001;34:125-130.
Questions?
. . . Continuing to other surgical complications.
Renal Abscess
Renal Cortical Abscesses
Hematogenous spread of bacteria from primary infectious foci elsewhere (i.e. skin)
S. aureus 90% 1
Risk Factors: DM, IVDU 1
Renal Corticomedullary Abscess
Complication of an ascending UTI 1
E. coli, Klebsiella, Proteus 1
Most commonly lead to perinephric abscesses 1
(1) Lee C, Henderson SO. Emergent surgical complications of genitourinary infections. Emerg Med Clin N Am. 2003;21:1057-1074.
Renal Cortical Abscesses
Clinical Features 1
Classic features: fever, flank pain
Women:Men 3:1
Mean age: 20-40
Laboratory:
Elevated WBC
Urinalysis: normal
Blood culture: negative
(1) Lee C, Henderson SO. Emergent surgical complications of genitourinary infections. Emerg Med Clin N Am. 2003;21:1057-1074.
Renal Corticomedullary Abscess
Clinical Features 1
Classic features: fever, flank pain
Recurrent UTIs (65%)
Renal calculi (30%)
Prior instrumentation (26%)
Laboratory:
Elevated WBC
Urinalysis abnormal: bacteriuria, pyuria, proteinuria, hematuria
(1) Lee C, Henderson SO. Emergent surgical complications of genitourinary infections. Emerg Med Clin N Am. 2003;21:1057-1074.
Diagnosis: Ultrasound
Characterizes a lesion as cystic, tumorous or suppurative
(1) Lee C, Henderson SO. Emergent surgical complications of genitourinary infections. Emerg Med Clin N Am. 2003;21:1057-1074.
Diagnosis: Ultrasound
(1) Myrier A. Renal and perinephric abscesses. 2008. Upto Date.
Diagnosis: CT Scan
CT scan provides the most anatomic information
Can detect abscesses <2cm 1
(1) Lee C, Henderson SO. Emergent surgical complications of genitourinary infections. Emerg Med Clin N Am. 2003;21:1057-1074.
Diagnosis: Imaging
Cortical Abscess
Diagnosis: Imaging
Corticomedullary Abscess
Treatment
Primary treatment – medical
Renal cortical abscesses:
Antistaphylococcal antibiotics
Surgery is rarely required
Renal corticomedullary abscesses:
Medical therapy often successful
Abscesses >5cm require surgical or interventional drainage
Indications for surgery;
Failure of Abx, >5cm abscess, multifocal abscess, obstructive uropathy, advanced age, deteriorating patient, immunocompromise
(1) Lee C, Henderson SO. Emergent surgical complications of genitourinary infections. Emerg Med Clin N Am. 2003;21:1057-1074.
Perinephric Abscess
Life-threatening condition when suppurative material occupies the perinephric space
E. coli, staph aureus, proteus 1
Mechanism: 2
Extension of renal abscess
Hematogenous spread
Extension from extrarenal inflammatory processes:
Diverticulitis, pyelosinus extravasation of urine
(1) Lee C, Henderson SO. Emergent surgical complications of genitourinary infections. Emerg Med Clin N Am. 2003;21:1057-1074.
(2) Demertzis J, Menias CO. State of the art: imaging of renal infections. Emerg Radiol. 2007;14:13-22.
Perinephric Abscess
Clinical Features
Fever, flank pain, vomiting
Referred pain: hip, thigh, knee
Laboratory:
Elevated WBC – non-specific
Urine – may be normal in up to 1/3 of patients
(1) Lee C, Henderson SO. Emergent surgical complications of genitourinary infections. Emerg Med Clin N Am. 2003;21:1057-1074.
Imaging: Perinephric Abscess
Ultrasound:
Mass with thickened, uneven walls with heterogenous echoes
False negatives in 36% compared to CT 1
CT:
Diagnostic test of choice 1,2
(1) Lee C, Henderson SO. Emergent surgical complications of genitourinary infections. Emerg Med Clin N Am. 2003;21:1057-1074.
(2) Demertzis J, Menias CO. State of the art: imaging of renal infections. Emerg Radiol. 2007;14:13-22.
CT: Perinephric Abscess
(1) Myrier A. Renal and perinephric abscesses. 2008. Upto Date.
Treatment
Mortality rates up to 50% 1
Treatment: 1
Appropriate aggressive antibiotics
Percutaneous drainage
Surgical drainage if percutaneous drainage contraindicated
Complications: 1
Distant extension -> empyema, colonic perforation
Direction extension -> Flank or psoas muscle
(1) Lee C, Henderson SO. Emergent surgical complications of genitourinary infections. Emerg Med Clin N Am. 2003;21:1057-1074.
Pyonephrosis
Infected Hydronephrosis: “Pus under pressure”
Obstruction: 1
Renal and ureteral calculi
Tumours
Iatrogenic stricture
Retroperitoneal fibrosis
Medical emergency!
Untreated pyonephrosis results in rapid destruction of renal parenchyma and sepsis
(1) Demertzis J, Menias CO. State of the art: imaging of renal infections. Emerg Radiol. 2007;14:13-22.
Diagnostic Imaging:
Pyonephrosis
Ultrasound: 1
Hydronephrosis with shifting urine-debris level
Test of choice
CT: 1
Difficult to differentiate simple hydronephrosis from pyonephrosis on CT
(1) Demertzis J, Menias CO. State of the art: imaging of renal infections. Emerg Radiol. 2007;14:13-22.
Pyonephrosis: Ultrasound
(1) Demertzis J, Menias CO. State of the art: imaging of renal infections. Emerg Radiol. 2007;14:13-22.
Xanthogranulomatous
Pyelonephritis
An uncommon reaction of the kidney to chronic infection in the setting of chronic obstruction
E. coli and proteus most common 1
Staghorn calculus most common obstruction 1
Lipid-laden macrophages on histology – xanthoma cells
(1) Demertzis J, Menias CO. State of the art: imaging of renal infections. Emerg Radiol. 2007;14:13-22.
Xanthogranulomatous
Pyelonephritis
Clinical Features
Adults
Middle-aged women
History of recurrent UTIs
Flank pain, fever, malaise, anorexia, weight loss
Signs: Unilateral renal mass
Laboratory:
Anemia, increased ESR, mild LFT abnormalities indicating mild biliary rentention
Urine: pyuria, bacteriuria – but may be sterile in 25% of cases
(1) Myrier A. Xanthogranulomatous pyelonephritis. Up to Date. 2008; Oct.
Imaging: CT Scan
Enlarged non-functioning kidney 1
Decreased contrast enhancement
Dilated calyces
Evidence of obstruction
(1) Demertzis J, Menias CO. State of the art: imaging of renal infections. Emerg Radiol. 2007;14:13-22.
CT Scan: Xanthogranulomatous Pyelonephritis
(1) Myrier A. Xanthogranulomatous pyelonephritis. Up to Date. 2008; Oct.
Treatment
1
Antibiotics to control infection
Nephrectomy often required due to virtually complete destruction of the kidney
Partial Nephrectomy – May be considered for localized form (usually children) or patients with bilateral disease
Nephrectomy or laparoscopic nephrectomy is an option for experienced practitioners 2
(1) Demertzis J, Menias CO. State of the art: imaging of renal infections. Emerg Radiol. 2007;14:13-22.
(2) Nicolle LE. Complicated pyelonephritis: unresolved issues. Current Infect Dis Reports. 2007;9:501-507.
Summary
Surgical Complications of Pyelonephritis
Emphysematous Pyelonephritis
Renal and perinephric Abscesses
Pyonephritis
Xanthogranulomatous Pyelonephritis
All require a high degree of suspicion, early appropriate imaging investigations, and surgical / interventional consultation.
Beware of the female patient with DM who doesn’t respond to antibiotics!
Don’t be fooled by a negative urinalysis.
Repeat imaging in a day if still maintain high suspicion.