NUTRITIONAL STATUS (NS)
advertisement

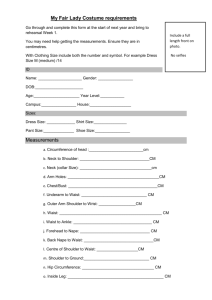
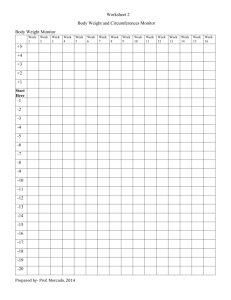
ASSESSMENT OF NUTRITIONAL STATUS Mgr. Dana Hrnčířová, Ph.D. Dpt. of Nutrition, 3rd Faculty of Medicine, Charles University NUTRITIONAL STATUS (NS) A part of general health status Adequate = good balance between the body's needs and the intake of nutrients Malnutrition imbalance between the body's needs and the intake of nutrients MALNUTRITION (broadly) undernutrition, overnutrition specific deficiencies develops in stages: nutrient levels in blood and/or tissues change intracellular changes in biochemical functions and structure symptoms and signs appear (morbidity and mortality can result) clinically intoxicated person well-nourished person clinically under-nourished person irreversible changes UNDERNUTRITION - PEM Marasmus Energy deficiency Severe deficiency of nearly all nutrients, esp. protein and carbohydrates Extreme weight loss, thinness Kwashiorkor protein deficiency (oedema, large fatty liver, swollen abdomen) Sufficient calorie intake (carbohydrates mainly) Marasmic kwashiorkor combined form Causes of malnutrition Loss of appetite, anorexia Digestion and absorption disorders Catabolic state – surgery, injuries, endocrine disorders Loss of proteins and liquids by fistulas, injuries … Pain Stress Infection … Consequences of Undernutrition PRIMARY: Protracted wound healing Increased tendency to infections (impaired immune functions) Hypoproteinosis (oedema) Decreased gut motility Myosthenia (muscle failing) Tendency to thrombosis, embolism Urinary tract infections Consequences of Undernutrition SECONDARY: increased morbidity prolonged hospitalization time prolonged recovery time increased mortality ASSESSMENT OF NUTRITIONAL STATUS 1) Clinical assessment nutritional and medical history, dietary assessment physical examination 2) Biochemical Laboratory Tests 3) Anthropometric Measurements NUTRITIONAL HISTORY Inevitably intertwined with the medical history Nutritional disorders Basic illnesses Nutrition related illnesses Digestion (diarrhoea, constipation) Weight (stable, variable) Weight loss / gain Loss of liquids? Increased energy demand? DIETARY ASSESSMENT Past intake Current intake 24-hour recall (week and weekend day) Food-frequency questionaire Diet history / dietary patterns in last 6 months Estimated food records Weighed food records Smoking habits Alcohol consumption Cooking techniques (boiling, frying, grilling, roasting, …) 24 – Hour Record Sex: _________ Date of birth: _____________ Weight: _____ kg Height: _____ cm Today’s date: ___________ List all foods and beverages you consumed in past 24 hours: night meal late evening meal evening meal snack 2 noon meal snack 1 morning meal food/drink quantity eaten food/drink quantity eaten PHYSICAL EXAMINATION Blood pressure (HT>140/90) Fragility of gum capillaries (paradontosis, vit. C def.) Somatoscopy PHYSICAL EXAMINATION - somatoscopy Skin – petechia, dermatitis, hyperkeratosis, seborea, hyperpigmentation, dry skin, oedema Head – hair quality, xerophthalmia, lips-angular cheilitis, tongueglositis, papilla atrophy, gums-bleeding, teeth-caries, spots Neck – examination of thyroid gland Chest – rib abnormalities, exudate Abdomen – acsites, liver size Limbs – oedemas, reflexes, sensation Skeleton – deformities, fractures, pain Skeletal muscle – atrophy BIOCHEMICAL LABORATORY TESTS Plasma proteins Total protein: 65-85 g/l Albumin: > 35 g/l (malnutrition < 28 g/l) Prealbumin Transferin Retinol binding protein BIOCHEMICAL LABORATORY TESTS Complete blood count (haematocrit, haemoglobin, RBC,WBC, lymphocytes, and differential count) Lymphocyte count: Normal values Mildly reduced > 1800/μl 1800 - 1500 Moderately reduced 1500 - 900 Severely reduced < 900 BIOCHEMICAL LABORATORY TESTS Plasma lipids Triacylglycerides < 1,7 mmol/l Total cholesterol < 5,0 mmol/l LDL-cholesterol < 3,0 mmol/l HDL-cholesterol > 1,0 mmol/l men > 1,2 mmol/l women ANTHROPOMETRIC MEASUREMENTS Indexes (to assess body weight) Body circumferences SkinFolds Rohrer’s index (RI) RI = body weight (gr) / height (cm)3 x 100 standards: men women 1,2 – 1,4 1,25 – 1,5 Body Mass Index (BMI) BMI is often used as a predictor of future disease risk. BMI = BODY WEIGHT (kg) / HEIGHT (m)2 WHO Classification Underweight BMI < 18,5 Desirable 18,5 - 24,9 Overweight 25,0 - 29,9 Grade 1 Obesity 30,0 - 34,9 Grade 2 Obesity 35,0 - 39,9 Grade 3 Obesity >40 BMI as the sole criterion indicating overweight and obesity is only informative up to a certain point! BODY FAT DISTRIBUTION Not whole body fat but its distribution determines risk of mortality and morbidity ABDOMINAL FAT Hyperinsulinemia, dyslipidaemia, hypertension, glucose intolerance Increases risk of DM II., cardiovascular diseases Waist circumference (WC) Waist/hip ratio /WHR) Waist Circumference Perhaps better indicator of cardiovascular and metabolic risks of obesity compared with WHR Classification Moderately high risk High risk Men > 94 cm > 102 cm Women > 80 cm > 88 cm Classification of overweight and obesity according to BMI and WC In connection with the risk of some diseases RISK OF DISEASES (relative to normal body weight Classification of body weight BMI (kg/m2) Classification and waist circumference) of obesity WAIST CIRCUMFERENCE men ≤ 102 cm men > 102 cm women ≤ 88 cm women > 88 cm underweight < 18,5 – – norm 18,5 - 24,9 – – overweight 25,0 - 29,9 increased high obesity 30,0 - 34,9 I high very high 35,0 - 39,9 II very high very high ≥ 40 III extremely high extremely high extreme obesity Waist to Hip Ratio (WHR) Indicator of cardiovascular disease risk Fat distributed mostly in the abdominal area is associated with higher morbidity and mortality due to cardiovascular disease. Waist – with abdomen relaxed, horizontal measure taken at the level of the narrowest part of waist below bottom of rib cage and above umbilicus Hips – while standing erect, horizontal measure taken at a level of maximum circumference of hips WHR = waist circumference / hip circumference Classification Moderately high risk High risk Men 0,9 - 1,0 > 1,0 Women 0,8 - 0,85 > 0,85 Mid–arm muscle area Used to estimate lean body muscle mass Derived from the TSF and the mid-arm circumference Mid-arm circumference - midway between the olecranon process and the acromium, right arm in a relaxed position Triceps skin fold - midway between the olecranon process and the acromium, on the posterior of the arm over the long head of the triceps brachii. Mid–Arm Circumference (cm) – 0,314 x Triceps Skinfold (mm) Muscle Mass Adequate Marginal Depleted Wasted Men 25,3 - 22,8 22,8 - 20,8 20,8 - 17,7 < 17,7 Women 23,2 - 20,9 20,9 - 18,6 18,6 - 16,2 < 16,2 Measurement of skinfolds Cheek – horizontal fold on a join tragus – nostrils, right bellow the temple Jowl – vertical fold between chin and laryngeal prominence Chest – anterior axillary fold (oblique). Diagonal fold taken ½ the distance between the anterior axillary line and the nipple (1/3 distance women). Axilla – at the intersection of a horizontal line level with the 10th rib and the anterior axillary line. Triceps – vertical fold on posterior midline of upper arm, midway between the acromion (bony tip of shoulder) and olecranon processes (elbow joint). Biceps – the pinch position is at the same level as for triceps, though on the anterior (front) surface of arm. Subscapula - 2 cm below the lower angle of the scapula (bottom point of shoulder blade) on a line running laterally and downwards (at about 45 degrees). Abdominal – vertical fold, is made 5 cm adjacent to the umbilicus (belly-button) taken on a line running laterally to the spina iliaca anterior Suprailiac – taken in the anterior axillary line immediately superior to the iliac crest Thigh – vertical fold above patella Calf – 5 cm below popliteal fossa Practical training Body circumferences 1. 2. 3. Mid-Arm Circumference Mid-Arm Muscle Area Waist Circumference Hip Circumference WHR Skinfolds 1. 2. 10 skinfolds 4 skinfolds % of body fat % of body fat Bioelectric impedance (BIA) Thank you for your attention.