3679grading3663
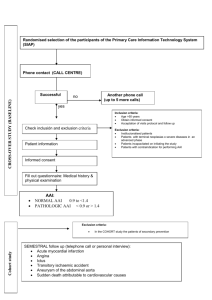
advertisement

BIOST 536 HW #3 Due: October 28, 2014, 21:30pm Code: 3663 1. Methods: The minimum of the observation time among patients still alive was compared to 4 years. Results: Te minimal time of follow up for the patients alive is 4.05 years meaning that they have at least 4 years of follow. So we can analyze this data using a binary outcome (death) and apply logistic regression. 2. a) Methods: univariate statistical techniques are employed to describe the binary variable death (proportion) and the continuous positive variable ankle-arm index (mean, standard deviation, minimum, maximum and variation coefficient). Results: There were 1121 (22.4%) deaths within the first 4 years of follow up as shown on table 1; the ankle-arm index (aai) ranged from 0.28 to 2.38 with mean 1.06 and small variation (16.5%). Table 1 – Descriptives of ankle-arm index Deaths with 4 year follow up No Yes 3879 (77.6%) Total, N (%) 1121 (22.4%) Ankle-arm index Min - Max Mean (SD) Missings, N (%) 0.28 - 2.38 1.08 (0.157) 81 (2.1%) 0.30 - 1.89 0.99 (0.211) 40 (3.6%) Total 5000 (100%) 0.28 - 2.38 1.06 (0.175) 121 (2.4%) 2.b) Methods: the association between death within the first 4 years and the baseline ankle-arm index (aai) is assed through a linear regression with robust standard error. Only 4879 records are used due to misingness on aai. P-values from Wald test are reported. Results: As shown on table 2 there is half reduction in mortality for 1 unity increase on ankle-arm index i.e for each 1/10 increase of aai the mortality decreases in 5% (95%CI: 4.2 - 5.8%). Table 2 – Risk difference modeled through linear regression Variable Ankle-arm index Constant Linear Coefficient (95% CI) p-value -0.50 (-0.58 – -0.42) 0.76 (0.67 – 0.84) < 0.001 < 0.001 2.c) Methods: the association between death within the first 4 years and the natural logarithm of the baseline anklearm index is assed through a linear regression with robust standard error. Only 4879 records are used due to missingness on aai. P-values from Wald test are reported. Results: As shown on table 3 there is almost half (0.47) reduction in mortality for 1 unity increase on natural logarithm of ankle-arm index. Table 3 – Risk difference modeled through linear regression Variable Log ankle-arm index Constant Linear Coefficient (95% CI) p-value -0.47 (-0.55 – -0.40) 0.24 (0.23 – 0.26) < 0.001 < 0.001 2.d) Methods: the association between death within the first 4 years and the baseline ankle-arm index is assed through a linear regression with robust standard error. A quadratic term of baseline ankle-arm index is included on the model. Only 4879 records are used due to missingness on aai. P-values from Wald test and from Fisher test are reported. Results: As shown on table 4 the quadratic aai is statistically significant indicating an U shaped relation between aai and risk difference. Because of this the risk difference has not the same slope on different segments of aai; the slope is linear -1.45 + 0.47aai. This indicates a reduction of risk mortality not more than 14.5% for each 1/10 increase on aai up to an aai of 1.54 from where there is an increased risk of death. Table 4 – Risk difference modeled through linear regression Variable Ankle-arm index Squared ankle-arm index Constant Linear Coefficient (95% CI) p-value -1.45 (-1.87 – -1.02) 0.47 (0.27 – 0.67) 1.21 (0.99 – 1.44) < 0.001 < 0.001 < 0.001 Overall p < 0.0001 through Fisher Test. 2.e) Methods: the association between death within the first 4 years and the baseline ankle-arm index is assed through a linear regression with robust standard error. The baseline ankle-arm index is transformed into an ordinal variable using these cut-points 0.25, 0.55, 0.75, 0.95, 1.15, 1.35, 1.55, 2.4. Only 4879 records are used due to misingness on aai. Pvalues from Wald test and from Fisher test are reported. also simultaneous testing of all parameters equal to 0 Results: As shown on table 5 there is a trend on risk mortality difference at different levels of baseline aai, varying from 3% increase up to 35% decrease in cumulative mortality on values of aai with 1.15 to 1.35. Table 5 – Risk difference modeled through linear regression using an ordinal categorized aai Variable Ordinal ankle-arm index < 0.55 0.55 – 0.75 0.75 – 0.95 0.95 – 1.15 1.15 – 1.35 1.35 – 1.55 ≥1.55 Constant Linear Coefficient (95% CI) p-value (reference) 0.03 (-0.10 – 0.16) -0.13 (-0.25 – -0.01) -0.29 (-0.41 - -0.18) -0.35 (-0.46 - -0.23) -0.26 (-0.40 - -0.12) -0.13 (-0.39 – 0.12) 0.620 0.037 < 0.001 < 0.001 < 0.001 0.303 0.49 (0.37 – 0.60) < 0.001 Overall p < 0.0001 through Fisher Test. 2.f) Methods: the association between death within the first 4 years and the baseline ankle-arm index is assed through a linear regression with robust standard error. The baseline ankle-arm index is transformed into an ordinal variable using these cut-points based on 7 equidistant quantiles (septile) of the cumulative distribution of ankle-arm index . Only 4879 records are used due to misingness on aai. P-values from Wald test and from Fisher test are reported. Testing of all parameters equal to 0… Results: As shown on table 6 there is a trend on risk mortality difference at different septile levels of baseline aai, varying from 21% up to 32% decrease in cumulative mortality. All reductions are statistically significant. Table 6 – Risk difference modeled through linear regression using an ordinal categorized aai Variable Ordinal ankle-arm index 1st septile 2nd septile 3rd septile 4th septile 5th septile 6th septile 7th septile Constant Linear Coefficient (95% CI) p-value (reference) -0.21 (-0.26 – -0.16) -0.25 (-0.30 – -0.21) -0.27 (-0.32 - -0.22) -0.28 (-0.33 - -0.24) -0.32 (-0.36 - -0.28) -0.29 (-0.33 – -0.24) < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 0.45 (0.42 – 0.49) < 0.001 Overall p < 0.0001 through Fisher Test. 2.g) Methods: the association between death within the first 4 years and the baseline ankle-arm index is assed through a linear regression with robust standard error. The baseline ankle-arm index is transformed into an ordinal variable using these cut-points based on 7 equidistant quantiles (septile) of the cumulative distribution of ankle-arm index . The resulting variable is incorporate on the regression as a continuous variable. Only 4879 records are used due to misingness on aai. P-values from Wald test are reported. Results: As shown on table 7 for each septile of AAI there is a statistically significant reduction in cumulative mortality of 4%. Table 7 – Risk difference modeled trough linear regression using septiles of AAI Variable Ankle-arm index Constant Linear Coefficient (95% CI) p-value -0.04 (-0.05 – -0.03) 0.38 (0.35 – 0.41) < 0.001 < 0.001 2.h) Methods: line plots are used to show different linear regressions fitting the proportion of death within first 4 years of follow up on untransformed AAI, logarithmesed AAI, untransformed AAI and quadratic term, AAI clinical relevant cutpoints and septiles of AAI. Results: All predicted values from the different risk difference regressions are shown on figure 1. The simple linear model without transformation suggests a constant reduction of the risk difference to a point where the proportion below 0 (which is inadmissible). But other models indicate an U or at least a reduction on the impact of AAI on risk difference between 1 and 1.5. It is to note that on models with categorical or ordered predictors the more levels or using of continuous small interval increment details on the nature of the relationship between AAI and risk-difference. Figure 1 – Different linear regression fitting of proportion of deaths over AAI 3.a) Methods: To assess the association between AAI and death within first 4 years of follow up odds-ratio (OR) is calculated for 1 unity increase on AAI. OR is shown also for 1/10 increase on AAI which is more clinical usefull. A logistic regression of death on AAI is used to obtain the OR. P-values from Wald test are reported. Results: The odd of dying in the first 4 years of follow up is 0.06 times per 1 unity increase of AAI (table 8); this is equivalent to an increase of the odds-ratio in 6.77x10-13 (95% CI: 1.45x10-14 - 3.17x10-11) per 1/10 increase of AAI. Should be noted this OR is close to zero (below 1) so it has the effect of protection on increase of AAI. Table 8 – Odds-ratio modeled trough logistic regression Variable Ankle-arm index Odds-Ratio (95% CI) p-value 0.06 (0.04 – 0.09) < 0.001 3.b) The answer to this question is the same as on 3a. 3.c) Methods: the association between death within the first 4 years and the natural logarithm of the baseline anklearm index is assed through a logistic regression. Only 4879 records are used due to missingness on aai. P-values from Wald test are reported. Results: As shown on table 9 the odds of dying within first 4 years is 0.087 for each 1 unity increase in the logarithm of the AAI. Table 9 – Odds-ratio modeled trough logistic regression on AAI logarithm Variable Log ankle-arm index Odds-Ratio (95% CI) p-value 0.087 (0.060 – 0.123) < 0.001 3.d) Methods: the association between death within the first 4 years and the baseline ankle-arm index is assed through a logistic regression. A quadratic term of baseline ankle-arm index is included on the model. Only 4879 records are used due to missingness on AAI. P-values from Wald test and from likelihood-ratio chi-squared test are reported. Results: As shown on table 10 the quadratic AAI is statistically significant indicating an U shaped relation between AAI and Odds-Ratio. It is to note that the Squared ankle-arm index has a smaller influence on the OR compared to the untransformed term (1/0.0026 = 384.6) suggesting predominance of the influence of non-transformed component of AAI within the range of the AAI on this dataset. Meaning that the odd of dying on first 4 years of follow up is reduced at maximum 385 times per one unity increase of AAI. There is an association b/w death and aai… Table 10 – Odds-Ratios modeled trough logistic regression Variable Ankle-arm index Squared ankle-arm index Odds-Ratio (95% CI) p-value 0.0026 (0.0003 – 0.0217) 5.3196 (1.7875 – 15.8308) < 0.001 < 0.001 Overall p < 0.0001 through likelihood-ratio chi-squared test. 3.e) Methods: the association between death within the first 4 years and the baseline ankle-arm index is assed through a logistic regression. The baseline ankle-arm index is transformed into an ordinal variable using these cut-points 0.25, 0.55, 0.75, 0.95, 1.15, 1.35, 1.55, 2.4. Only 4879 records are used due to misingness on aai. P-values from Wald test and from Fisher test are reported. Testing of all parameters… Results: As shown on table 11 there is a decreasing trend on the odds to dye within first 4 years at different levels of baseline AAI, decreasing from 1.14 to 0.17 on AAI within 1.15 to 1.35 and then ascending again. Is there an association? Table 11 – Odds-Ratios modeled through logistic regression using an ordinal categorized AAI Variable Ordinal ankle-arm index < 0.55 0.55 – 0.75 0.75 – 0.95 0.95 – 1.15 1.15 – 1.35 1.35 – 1.55 ≥1.55 Odds-Ratio (95% CI) p-value (reference) 1.14 (0.68 – 1.93) 0.59 (0.36 – 0.96) 0.26 (0.16 – 0.41) 0.17 (0.11 – 0.28) 0.31 (0.16 – 0.60) 0.58 (0.19 – 1.72) 0.620 0.033 < 0.001 < 0.001 < 0.001 0.323 Overall p < 0.0001 through likelihood-ratio chi-squared test. 3.f) Methods: the association between death within the first 4 years and the baseline ankle-arm index is assed through a logistic regression. The baseline ankle-arm index is transformed into an ordinal variable using these cut-points based on 7 equidistant quantiles (septile) of the cumulative distribution of ankle-arm index . Only 4879 records are used due to misingness on aai. P-values from Wald test and from likelihood-ratio chi-squared test are reported. Results: As shown on table 12 there is a reducing trend on odds to die within first 4 years risk at increasing septile levels of baseline AAI, varying from 0.39 up to 0.19 and increasing on last septile to 0.24. Table 12 – Odds-Ratios modeled through logistic regression using an ordinal categorized AAI Variable Ordinal ankle-arm index 1st septile 2nd septile 3rd septile 4th septile 5th septile 6th septile 7th septile Odds-Ratio (95% CI) p-value (reference) 0.39 (0.31 – 0.49) 0.31 (0.24 – 0.38) 0.27 (0.21 – 0.35) 0.25 (0.19 – 0.32) 0.19 (0.14 – 0.24) 0.24 (0.19 – 0.31) < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 Overall p < 0.0001 through likelihood-ratio chi-squared test. 3.g) Methods: the association between death within the first 4 years and the baseline ankle-arm index is assed through a logistic regression. The baseline ankle-arm index is transformed into an ordinal variable using these cut-points based on 7 equidistant quantiles (septile) of the cumulative distribution of ankle-arm index . The resulting variable is incorporate on the regression as a continuous variable. Only 4879 records are used due to misingness on aai. P-values from Wald test are reported. Results: As shown on table 13 for each septile of AAI there is a statistically significant reduction in odds to die within first 4 years by 1.27 (1/0.79) times. Table 13 – Odds-Ratios modeled through logistic regression using septiles of AAI Variable Ankle-arm index Risk-Ratio (95% CI) p-value 0.79 (0.76 – 0.82) < 0.001 3.h) Methods: line plots are used to show different logistic regressions fitting the proportion of death within first 4 years of follow up on untransformed AAI, logarithmesed AAI, untransformed AAI and quadratic term, AAI clinical relevant cutpoints and septiles of AAI. Results: All predicted values from the different logistic regressions are shown on figure 2. All models agree that the risk of death has a decreasing trend before somewhere 1.2 to 1.4 on AAI. Then different models show marked pattern. It is for note that the quadratic and the ordered clinical relevant cut points show increase in risk, while the continuous septiles show an unchangeable risk. All models show plausible proportion i.e between 0 and 1. Choice of model for confounder vs poi vs precision? Figure 2 – Different logistic regression fitting of proportion of deaths over AAI 4.a) Methods: To assess the association between AAI and death within first 4 years of follow up incidence rate ratios (or risk ratio, RR) is calculated for 1 unity increase on AAI. RR is shown also for 1/10 increase on AAI which is more clinical useful. A poisson regression of death on AAI is used to obtain the RR. P-values from Wald test are reported. Results: The risk in the first 4 years of follow up is 0.09 times per 1 unity increase of AAI (table 14); this is equivalent to an increase of the risk-relative in 5.08x10-11 (95% CI: 2.79x10-12 – 9.23x10-10) per 1/10 increase of AAI. Should be noted this OR is close to zero (below 1) so it has the effect of protection on increase of AAI. Table 14 – Risk-ratio modeled trough poisson regression Variable Ankle-arm index Risk-Ratio (95% CI) p-value 0.09 (0.07 – 0.12) < 0.001 4.b) The answer to this question is the same as on 4a. 4.c) Methods: the association between death within the first 4 years and the natural logarithm of the baseline anklearm index is assed through a poisson regression. Only 4879 records are used due to missingness on aai. P-values from Wald test are reported. Results: As shown on table 15 the risk of dying within first 4 years is 0.156 for each 1 unity increase in the logarithm of the AAI. Table 15 – Risk-ratio modeled trough poisson regression on AAI logarithm Variable Log ankle-arm index Risk-Ratio (95% CI) p-value 0.156 (0.125 – 0.195) < 0.001 4.d) Methods: the association between death within the first 4 years and the baseline ankle-arm index is assed through a poisson regression. A quadratic term of baseline ankle-arm index is included on the model. Only 4879 records are used due to missingness on AAI. P-values from Wald test and from likelihood-ratio chi-squared test are reported. Results: As shown on table 16 the quadratic AAI is not statistically significant though the model is. There is not much change on the log-likelihood (less than 1 from the simple model to the quadratic term). Anyway it is to note that the Squared ankle-arm index has a smaller influence on the RR compared to the untransformed term (1/0.093448 = 10.7) suggesting predominance of the influence of non-transformed component of AAI within the range of the AAI on this dataset. Meaning that the risk of dying within first 4 years of follow up is reduced at maximum 11 times per one unity increase of AAI. Table 16 – Risk-Ratios modeled trough poisson regression Variable Ankle-arm index Squared ankle-arm index Risk-Ratio (95% CI) p-value 0.0345 (0.0063 – 0.1895) 1.7526 (0.6805 – 4.5135) < 0.001 0.245 Overall p < 0.0001 through likelihood-ratio chi-squared test. 4.e) Methods: the association between death within the first 4 years and the baseline ankle-arm index is assed through a poisson regression. The baseline ankle-arm index is transformed into an ordinal variable using these cut-points 0.25, 0.55, 0.75, 0.95, 1.15, 1.35, 1.55, 2.4. Only 4879 records are used due to misingness on aai. P-values from Wald test and from Fisher test are reported. Testing all parameters=0 Results: As shown on table 17 there is a decreasing trend on the risk to dye within first 4 years at different levels of baseline AAI, decreasing from 0.95 to 0.20 on AAI within 1.15 to 1.35 and then ascending again. Is there an association? Table 17 – Risk-Ratios modeled trough poisson regression using an ordinal categorized AAI Variable Ordinal ankle-arm index < 0.55 0.55 – 0.75 0.75 – 0.95 0.95 – 1.15 1.15 – 1.35 1.35 – 1.55 ≥1.55 Risk-Ratio (95% CI) p-value (reference) 0.95 (0.66 – 1.38) 0.60 (0.42 – 0.85) 0.29 (0.21 – 0.40) 0.20 (0.14 – 0.29) 0.34 (0.20 – 0.58) 0.52 (0.22 – 1.24) 0.801 0.004 < 0.001 < 0.001 < 0.001 0.141 Overall p < 0.0001 through likelihood-ratio chi-squared test. 4.f) Methods: the association between death within the first 4 years and the baseline ankle-arm index is assed through a poisson regression. The baseline ankle-arm index is transformed into an ordinal variable using these cut-points based on 7 equidistant quantiles (septile) of the cumulative distribution of ankle-arm index . Only 4879 records are used due to misingness on aai. P-values from Wald test and from likelihood-ratio chi-squared test are reported. Results: As shown on table 16 there is a reducing trend on risk to die within first 4 years risk at increasing septile levels of baseline AAI, varying from 0.45 up to 0.23 and increasing on last septile to 0.29. Table 18 – Risk-Ratios modeled through poisson regression using an ordinal categorized AAI Variable Ordinal ankle-arm index 1st septile 2nd septile 3rd septile 4th septile 5th septile 6th septile 7th septile Risk-Ratio (95% CI) p-value (reference) 0.45 (0.38 – 0.55) 0.36 (0.30 – 0.44) 0.33 (0.27 – 0.41) 0.30 (0.25 – 0.38) 0.23 (0.19 – 0.30) 0.29 (0.24 – 0.37) < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 < 0.001 Overall p < 0.0001 through likelihood-ratio chi-squared test. 4.g) Methods: the association between death within the first 4 years and the baseline ankle-arm index is assed through a poisson regression. The baseline ankle-arm index is transformed into an ordinal variable using these cut-points based on 7 equidistant quantiles (septile) of the cumulative distribution of ankle-arm index . The resulting variable is incorporate on the regression as a continuous variable. Only 4879 records are used due to misingness on aai. P-values from Wald test are reported. Results: As shown on table 19 for each septile of AAI there is a statistically significant reduction in risk to die within first 4 years by 1.25 (1/0.80) times. Table 19 – Risk-Ratios modeled through poisson regression using septiles of AAI Variable Ankle-arm index Risk-Ratio (95% CI) p-value 0.80 (0.78 – 0.83) < 0.001 4.h) Methods: line plots are used to show different poisson regressions fitting the incidence of death within first 4 years (per year) of follow up on untransformed AAI, logarithmesed AAI, untransformed AAI and quadratic term, AAI clinical relevant cutpoints and septiles of AAI. All plots have been smoothed trough the use of lowess. Results: All predicted values from the different poisson regressions are shown on figure 3. All models generally show decrease on the risk of death except the ordered and relevant cutpoints, the dummy septiles and continuous septiles which suggest a U like curve. Dummy variables should not look connected as below Figure 3 – Different poisson regression fitting of incidence of deaths over AAI 5. Methods: Different risk associations (risk difference, odds-ratio and risk-ratios) are compared. Diverse tables and plots produced on previous questions are reused. Results: generally all analysis suggests a decreasing in risk of death before when AAI moves from 0 to 1. The linear regression untransformed and logarithmzed potentially produce implausible proportions (negative). Other models show some concavity (with different degrees on each model) on the interval 1.2 – 1.4 and ascending risk for larger AAI values. Anyway the extreme values of AAI (below 0.2 or above 2) have few people and that affects estimates, specially those from categorized (non continuous predictors) producing very different fitting. -dummy variables are saturate linear splines better than linear/log/quadratic fits at more extreme values