Infectious Disease Myths (or are they myths?)
advertisement
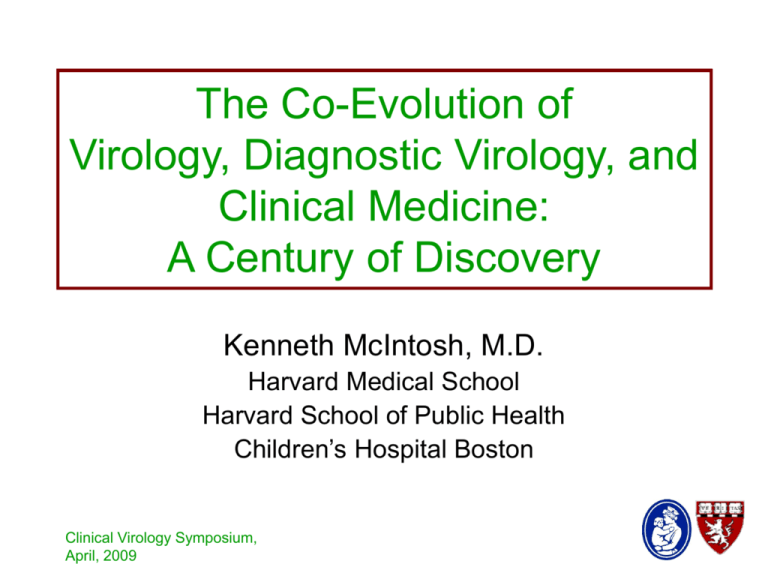
The Co-Evolution of Virology, Diagnostic Virology, and Clinical Medicine: A Century of Discovery Kenneth McIntosh, M.D. Harvard Medical School Harvard School of Public Health Children’s Hospital Boston Clinical Virology Symposium, April, 2009 The Evolution of Virology • There is some question of when “Virology” can be said to have begun. • Many diseases we now know as viral were recognized (smallpox, measles, polio), and even immunized against (smallpox), all of this before viruses were first described. • Dmitry Ivanovsky was the first to show that the infectious agent that caused a disease, in this case tobacco mosaic disease, could be filtered through porcelain filters that would block bacteria. This was in 1892. Clinical Virology Symposium, April, 2009 The Evolution of Virology • I prefer to think that “Virology” began a few years before this, with a Scotsman named John Brown Buist. Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnostic) • The Beginning • John Brown Buist was a Scottish pathologist and medical practitioner who devoted much of his professional life to vaccination. • Published Vaccinia and Variola in 1887 Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnostic) • John Brown Buist’s studies: • He devised a method for staining the material from a cowpox (vaccinia) vesicle Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnostic) • Buist’s conclusions: • The particles he saw were considered to be the spores of micrococci, evolving into the particles seen in pustules during the course of the disease • Smallest particles were associated with most effective smallpox vaccination Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnostic) • Buist’s contribution: • This was the first recorded detection of virus directly in material obtained from a lesion in a disease caused by a virus (even though, since viruses had not been described, the particles were called spores). • This was also the first rapid laboratory diagnosis of a viral disease. • Buist also associated the small (viral) particles with infectivity. • The work was all done 6 years before viruses as filterable, infectious particles, were described. Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnostic) • Inclusion Bodies • Several physicians associated intracellular inclusion bodies with the pathology of diseases that, usually later, were shown to be caused by viruses. • An early example was in smallpox, where histologic studies were done of the base of the lesions, by Guarnieri in 1892 Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnostic) • Inclusion Bodies • Another early example was in rabies, from impression smears made from rabid dogs, by Negri in 1903 Clinical Virology Symposium, April, 2009 The Evolution of Virology • Growth of Virus • Animal inoculation • Animal (or human) inoculation was essentially the only way to grow viruses in the early days (e.g. rabies virus in the CNS of rabbits, by Pasteur in the 1890’s; or maintenance of smallpox vaccine in orphans for transatlantic shipment in the early 19th century). • Embryonated eggs • First successful passage of a virus in eggs was Rous Sarcoma Virus by Rous and Murphy in 1911. Clinical Virology Symposium, April, 2009 The Evolution of Virology • Growth of Virus • Embryonated eggs • The next use of embryonated eggs for virus passage was 20 years later, when smallpox and vaccinia were grown by Woodruff and Goodpasture in 1931. They also showed that the virus could be titrated by counting pox in the allantoic membrane. • Burnet used chick embryos to grow influenza virus for the first time in 1940. This system has been used since that time for production of vaccine. Clinical Virology Symposium, April, 2009 The Evolution of Virology (public health and patient care) • Yellow fever (a flavivirus, transmitted by the bite of several species of mosquito) • Originated in Africa, brought to the Americas by the slave trade. • Devastated the military during the SpanishAmerican War (1898). • Thought to be spread by miasmas, or contaminated fomites. • Killed many important people, including a number of those investigating it, as well as volunteers who were inoculated with infected blood. Clinical Virology Symposium, April, 2009 The Evolution of Virology (public health and patient care) • Yellow fever (earliest studies) • Walter Reed • Undertook experiments during the summer of 1900 in Cuba to prove that mosquito bites were, in fact, the mode of infection. • At the time of these experiments, yellow fever was not known to occur in any animal species, so even animal experiments were not possible. Clinical Virology Symposium, April, 2009 The Evolution of Virology (public health and patient care) • Yellow fever (earliest studies) • Walter Reed • In a facility built specifically for the purpose, Reed subjected consenting young male volunteers to bites by C. fasciatus (now known as Aedes aegyptae) mosquitoes that had, about 2 weeks previously, bitten patients early in the course of natural (often fatal) yellow fever. Clinical Virology Symposium, April, 2009 The Evolution of Virology (public health and patient care) • Yellow fever (earliest studies) • Walter Reed. • The volunteers came down with clinical yellow fever 2-4 days later. Fortunately, all these volunteers survived. • Reed was also able to show that fomites were not responsible for spreading the disease, by having volunteers sleep in grossly contaminated bed linens. • In related experiments, Reed and his team showed that the responsible agent passed through porcelain filters and still produced disease in volunteers, and was therefore a virus. Clinical Virology Symposium, April, 2009 The Evolution of Virology (public health and patient care) • Yellow fever • Walter Reed. • Because of these scrupulously performed experiments, the incidence of Yellow Fever in the military, with proper mosquito control, dropped precipitously. • Reed’s colleagues, Jefferson Kean and William Gorgas, instituted the control measures that allowed the digging of the Panama Canal just a few years later. Clinical Virology Symposium, April, 2009 The Evolution of Virology (public health and patient care) • Yellow fever (tissue culture and vaccine development) • Max Theiler • Theiler was a South African, born in 1899 to Swiss parents, who began work at the Rockefeller Institute in New York City in 1930. • Theiler used a combination of animal inoculation and chick embryo tissue culture to study the dual pathogenicity of yellow fever virus in the liver and the brain. Clinical Virology Symposium, April, 2009 The Evolution of Virology (public health and patient care) • Yellow fever (tissue culture and vaccine development) • Max Theiler • The chick embryo tissue culture methods that Theiler used were developed first by Alexis Carrel. Clinical Virology Symposium, April, 2009 The Evolution of Virology (public health and patient care) • Yellow fever (tissue culture and vaccine development) • Max Theiler • During these pathogenicity studies, and after over 200 passages in chick embryo tissue culture, Theiler gradually attenuated the Yellow Fever virus and developed the 17D vaccine that is used today. Clinical Virology Symposium, April, 2009 The Evolution of Virology (public health and patient care) • Yellow fever (tissue culture and vaccine development) • Max Theiler • The attenuation methods that Theiler pioneered (passage in tissue culture) were the basis for the development of vaccines for essentially all attenuated human viral vaccines before the molecular era: Measles Rubella Mumps Clinical Virology Symposium, April, 2009 Polio Varicella The Evolution of Virology • The studies described so far were all of severe viral diseases where infectious material from patients could be removed from sterile sites (brain, skin pustules, blood, liver). • Influenza is an example of the difficulties inherent in trying to work with viruses in nonsterile sites before the advent of antibiotics. Clinical Virology Symposium, April, 2009 The Evolution of Virology (public health and patient care) • Influenza • From the huge pandemic of 1918 until the early 1930’s controversy raged about what was the cause of the “great influenza.” • The battle came down to two camps: • Haemophilus influenzae • A filterable virus • There were innumerable “demonstrations” of disease, induced in human volunteers or various animal models, from both camps. None of them was convincing. Clinical Virology Symposium, April, 2009 The Evolution of Virology (public health and patient care) • Influenza • Order began to appear in 1931 • Shope, at the Rockefeller Institute, developed an elegant model in pigs: Swine influenza, where mild respiratory disease was produced with the filterable agent, and severe disease with a combination of the virus and H. influenzae suis. • Then in 1933 Smith, Andrewes, and Laidlaw in England transferred a filterable agent from clinical cases to ferrets. • This agent proved serologically close to Shope’s swine influenza. Clinical Virology Symposium, April, 2009 The Evolution of Virology (public health and patient care) • Influenza: Consistency • In 1934, from a separate outbreak of influenza, Thomas Rivers at the Rockefeller Institute duplicated exactly the ferret experiments of Smith, Andrewes and Laidlaw. • In 1940, Macfarlane Burnet in Australia isolated influenza virus in embryonated eggs using samples from an earlier local outbreak. • Suddenly, everything became much clearer. Clinical Virology Symposium, April, 2009 Smith, Andrewes, Laidlaw. Lancet 1933;2:66-68. The Evolution of Virology (diagnosis) • Growth of Virus • Tissue culture • Early efforts: vaccinia was grown in 1913 in explants of rabbit cornea. • First recognition of cytologic changes in culture was in 1929 (early concepts of cytopathic effect, or CPE): • Andrewes in England, with Virus III (a herpesvirus of rabbits) • Rivers and colleagues, with vaccinia Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnosis) • Growth of Virus • Tissue culture • Rolling of cultures • Alexis Carrel, 1913, suggested the idea • Gey, 1933, actually did it, on a large scale, at the Johns Hopkins Hospital, and then, with Frederick Bang, grew and studied LGV, including demonstration of the inclusion bodies in unstained monolayers. Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnosis, public health and patient care) • Growth of Virus • Tissue culture • After World War II, antibiotics began to be used in tissue culture. This made it possible to inoculate clinical specimens directly into culture. • Advances came at a rapid pace: • Vaccinia (Feller, Enders and Weller, 1940) • Poliovirus (Enders, Weller and Robbins, 1949) Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnosis, public health and patient care) • Growth of Poliovirus in Tissue Culture • The situation before 1949: • Poliovirus was grown dependably only in monkeys, passaging by inoculation of neural tissue into the CNS. • Simon Flexner, in 1910, had tried and failed to grow poliovirus in non-neural tissue culture. • Sabin had tried the same thing and failed in the 1930’s. Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnosis, public health and patient care) • Growth of Poliovirus in Tissue Culture • Thomas Weller’s first tissue culture experiments: • The Enders lab had a strain of poliovirus (the Lansing strain – a Type 2 strain) that had been adapted to growth in mouse central nervous system. • Weller was trying to grow varicella virus in “Maitland” tissue cultures: mixtures of human embryonic skin and muscle cells kept alive in 25 ml Erlenmeyer flasks with frequent changes of the fluid medium. Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnosis, public health and patient care) • Growth of Poliovirus in Tissue Culture • Weller’s first tissue culture experiments: • During an experiment on varicella in April, 1948, there were four unused flasks. On a whim Weller inoculated them with mouse brain containing the Lansing strain of poliovirus. Nine days later, attempts to find residual varicella failed. However,when mice were inoculated intracerebrally with the tissue culture fluid from the polio cultures, they became paralyzed. Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnosis, public health and patient care) • This preliminary experiment was followed by others and published in a series of papers by Weller, Enders, and Robbins. Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnosis, public health and patient care) • Growth of Poliovirus in Tissue Culture • With the work on poliovirus, the word “cytopathogenic effect” was first used by Enders. • It was also recognized that CPE could be used to quantitate virus • In 1949, with the addition of penicillin and streptomycin to culture fluid, poliovirus was recovered in tissue culture from the stools of patients with poliomyelitis. Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnosis) • Immunology in the service of viral diagnosis • Agglutination • Early 20th Century, agglutination of smallpox particles from vesicular fluid with animal sera • Development of complement fixation (Bedson and Bland, 1929) • Application to the fluid of smallpox vesicles by Parker and Muckenfuss, 1932. Clinical Virology Symposium, April, 2009 The Evolution of Virology (Parker and Muckenfuss, PSEBM 1932;29;483-5) Disease No. of samples Timing No. positive Vaccinia 7 7 Variola 16 6-10 days after primary vaccination 1-14 days after eruption Control 10 Clinical Virology Symposium, April, 2009 Remarks 14 Negative on 12th and 14th days. 0 Varicella, impetigo, pemphigus, exfoliative dermatitis The Evolution of Virology (diagnosis, patient care) • Immunofluorescence • Coons and colleagues, in 1942, conjugated antibodies with fluorescein for the first time, and used them to identify pneumococcal antigens in tissue. • In conjunction with tissue culture, immunofluorescence became a potent tool: • In 1953, Weller, after finally producing CPE with varicella virus in roller tube cultures, used the FA technique to prove that the virus reacted with convalescent serum, thereby demonstrating the antibody response, as well as the location of the virus intracellularly. Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnosis, patient care) • Immunofluorescence for rapid diagnosis • Ch’ien Liu (1956) identified influenza directly in the secretions of Harvard undergraduates in the winter of 1952-53. Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnosis, patient care) • Solid phase assays for viral diagnosis • RIA as a technique • Yalow and Berson, 1960, developed RIA for measurement of insulin in serum • Use of a “solid” support was first described by Jacob and Monod in 1961 • Plastic tubes, beads or wells were first used in 1967. Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnosis, patient care) • The quality, specificity, speed of all immune-based tests designed to detect viral antigens in clinical materials was vastly improved with the development of monoclonal antibodies in the early 1970’s by Kohler and Milstein Clinical Virology Symposium, April, 2009 The Evolution of Virology • Nobel Prizes for Physiology and Medicine • • • • • • • • Alexis Carrel (1912) Max Theiler (1951) Enders, Weller and Robbins (1954) Macfarlane Burnet (1960) Monod and Jacob (1965) Peyton Rous (1966) Rosalyn Yalow (1977) Jerne, Kohler and Milstein (1984) Clinical Virology Symposium, April, 2009 The Evolution of Virology (diagnosis, public health and patient care) • The molecular virology era • Of course progress has not slowed in the last few decades: • PCR and other molecular methods for diagnosis • Virus discovery and progress using purely molecular methods (hepatitis C virus; human papillomavirus; coronaviruses, bocavirus, many others) • Designer antiviral drugs (protease and integrase inhibitors for HIV) • Molecular epidemiology Clinical Virology Symposium, April, 2009 The Evolution of Virology • The molecular virology era • Nor have Nobel Prizes stopped coming: • 1975 - David Baltimore, Renato Dulbecco, Howard Temin • 1989 - Michael Bishop, Harold Varmus • 1997 - Stanley Prusiner • 2008 - Harald zur Hausen, Françoise BarréSinoussi, Luc Montagnier Clinical Virology Symposium, April, 2009 The Evolution of Virology • The Impact on Medicine (review) • Public Health • Diagnosis • Patient Care Clinical Virology Symposium, April, 2009 The Evolution of Virology • The Impact on Medicine • Public Health • The ability to understand pathophysiology, and therefore control diseases (e.g. yellow fever) • The ability to describe the epidemiology, and therefore control diseases (e.g. influenza) • The development of vaccines Clinical Virology Symposium, April, 2009 The Evolution of Virology • The Impact on Medicine • Diagnosis • We have gone from purely clinical diagnosis, through retrospective diagnosis by acute and convalescent antibody measurement, to rapid diagnosis. • • • • Buist Immunofluorescence Solid phase, point-of-care assays PCR and other molecular methods Clinical Virology Symposium, April, 2009 The Evolution of Virology • The Impact on Medicine • Patient care • More rapid, specific, and point-of-care diagnostics • Antiviral treatment and prophylaxis • Amantadine, acyclovir • Ganciclovir, neuraminidase inhibitors • Drugs for HIV, including NRTI’s, NNRTI’s, Protease Inhibitors, Integrase Inhibitors, and more. Clinical Virology Symposium, April, 2009 Mortality Rates (% per year) among HIV infected subjects enrolled in PACTG 219 prior to Jan 1, 1996 6 5 4 3 2 1 0 1996 1997 1998 1999 Mortality (%) 5.25 2.07 0.94 0.7 Logrank test for trend significant P<0.0001 Clinical Virology Symposium, April, 2009 Clinical Virology Symposium, April, 2009 Cooper ER et al: JAIDS 2002;29:484-94 U.S. Is Close to Eliminating AIDS in Infants, Officials Say By MARC SANTORA Published: January 30, 2005 AIDS among infants, which only a decade ago took the lives of hundreds of babies a year and left doctors in despair, may be on the verge of being eliminated in the United States, public health officials say. Clinical Virology Symposium, April, 2009 Thank you! Clinical Virology Symposium, April, 2009