The liver
advertisement

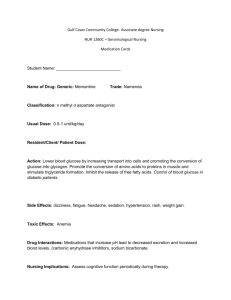
The Integration of Metabolism Week 13 & 14 Tissue-Specific Metabolism Each tissue of the human body has a specialized function, reflected in its anatomy and metabolic activity The liver is the central distributing and processing organ for nutrients. Sugars produced in digestion cross the intestinal epithelium and enter the blood, which carries them to the liver Glucose 6-phosphate is the key intermediate in carbohydrate metabolism. It may be polymerized into glycogen, dephosphorylated to blood glucose, or converted to fatty acids via acetyl-CoA. It may undergo oxidation by glycolysis, the citric acid cycle, and respiratory chain to yield ATP. or enter the pentose phosphate pathway to yield pentoses and NADPH. Amino acids produced in digestion cross the intestinal epithelium and enter the blood, which carries them to the liver Amino acids are used to synthesize liver and plasma proteins, or their carbon skeletons are converted to glucose and glycogen by gluconeogenesis; the ammonia formed by deamination is converted to urea. Some triacylglycerols derived from ingested lipids also make their way to the liver, where the constituent fatty acids are used in a variety of processes The liver converts fatty acids to triacylglycerols, phospholipids, or cholesterol and its esters, for transport as plasma lipoproteins to adipose tissue for storage. Fatty acids can also be oxidized to yield ATP or to form ketone bodies, which are circulated to other tissues. Skeletal muscle is specialized to produce and use ATP for mechanical work. During strenuous muscular activity, glycogen is the ultimate fuel, supplying ATP through lactic acid fermentation. During recovery, the lactate is reconverted (through gluconeogenesis) to glycogen and glucose in the liver. Phosphocreatine is an immediate source of ATP during active contraction Heart muscle obtains nearly all its ATP from oxidative phosphorylation Extremely active muscles use glycogen as energy source, generating lactate via glycolysis. During recovery, some of this lactate is transported to the liver and converted to glucose via gluconeogenesis. This glucose is released to the blood and returned to the muscles to replenish their glycogen stores. The overall pathway (glucose → lactate → glucose) constitutes the Cori cycle The neurons of the brain use only glucose and β-hydroxybutyrate as fuels, the latter being important during fasting or starvation. The brain uses most of its ATP for the active transport of Na and K and maintenance of the electrical potential across the neuronal membrane. The blood carries nutrients, waste products, and hormonal signals among the organs. Food intake and starvation induce metabolic changes Starved-fed cycle Nightly starved-fed cycle has 3 stages: • Postabsorbtive state • Early fasting during the night • The refed state after breakfast Main goal is to maintain glc homeostasis! The well-fed state After the consumption Glc, aa’s and lipids are transported to the blood The fed state The secretion of insulin increases. Insulin increases the uptake of Glc into the liver by GLUT2 Insulin also increases the uptake of Glc by muscle and adipose tissue The electron micrograph shows the release of insulin from a pancreatic b cell. One secretory granule is on the verge of fusing with the plasma membrane and releasing insulin into the extracellular space, and the other has already released the hormone Early fasting state The blood Glc decreases several hors after a meal Insulin decreases and glucagon increases So, glucagon signals the starved state It mobilizes the glycogen by cAMP pathway Target liver Net result: Increase glucose in blood The refed state Fat process same as fed state The liver does not initially absorb glc from the blood, but rather leaves it for the peripheral tissues Liver stays in gluconeogenic mode Newly made Glc is used to make glycogen As blood Glc increases the liver completes the replenishment of its glycogen stores Metabolic adaptation in prolonged starvation minimize protein degradation What are the adaptations if fasting is prolonged to the point of starvation? – 70 kg man has fuel reserve ~ 161,000 kcal – The energy need for a 24 hr cycle 1600-6000 kcal – So, fuels are ok for 1-3 months! The very first priority of metabolism in starvation – Providing Glc to the brain and other tissues The second priority of metabolism in starvation is to preserve protein, which is accomplished by shifting from glc to fa’s Fuel metabolism in the liver during prolonged starvation Fuel Choice During Starvation. The plasma levels of fatty acids and ketone bodies increase in starvation, whereas that of glucose decreases. • Plasma concentrations of fatty acids, glucose, and ketone bodies during the first week of starvation. • Despite the hormonal mechanisms for maintaining the level of glucose in blood, glucose begins to diminish after 2 days of fasting. • The level of ketone bodies, almost unmeasurable before the fast, rises dramatically after 2 to 4 days of fasting. These water-soluble ketones, acetoacetate and β-hydroxybutyrate, supplement glucose as an energy source during a long fast. Fatty acids cannot serve as a fuel for the brain; they do not cross the blood-brain barrier. After 3 days of starvation Liver forms keton bodies Their synthesis from AcetylCoA is increased because TCA is not running(gluconeogenesis depletes the supply of oxaloacetate) So, liver makes lots of KBs The brain begins to use acetoacetate After 3 days, 1/3 of the energy comes from KBs for the brain The heart also uses KBs Regulation of blood glucose by insulin and glucagon