Incidence and Risk Factors of Rash from Efavirenz in HIV
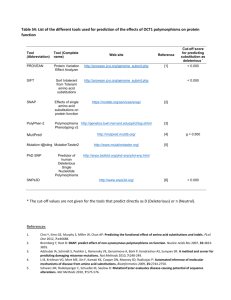
advertisement

Poster M-105 Protease Polymorphisms in HIV-1 Subtype CRF01_AE Represent Selection by Antiretroviral Therapy and Host Immune Pressure Weerawat Manosuthi1,2, David M. Butler2, Josué Perez2, Art F. Y. Poon2, Sergei Kosakovsky Pond2, Satish K. Pillai3, Sanjay R. Mehta2, Mary E. Pacold2, Douglas D. Richman2,4, Davey M. Smith2,4 (Contact: drweerawat@hotmail.com) 1Bamrasnaradura Infectious Diseases Institute, Ministry of Public Health, Thailand 2University of California San Diego, CA 3University of California San Francisco, CA 4Veterans Affairs San Diego Healthcare System, San Diego, CA, USA INTRODUCTION RESULTS ▪ Resistance to protease inhibitors (PIs) develops with the acquisition of mutations in the protease gene (pro). These resistance-associated mutations can be classified as either major or accessory (Hammer 2008). ▪ 1,322 sequences between 1990 - 2007 were retrieved. 328 duplicated sequences and 6 nonCRF01_AE sequences were excluded. Analysis demonstrated that all remaining 988 sequences were not hypermutated. ▪ 846 (86%) sequences were from Asian countries and 142 (14%) sequences came from non-Asian countries. Asian countries included Thailand (22%), Vietnam (18%), China (17%), Cambodia (13%), Singapore (10%), Japan (5%) and others (1%). ▪ Phylogenetic analysis demonstrated that the branch length between CRF01_AE pro sequences revealed relatively low genetic diversity and overall percentage of pairwise similarity was 96%. ▪ The frequencies of major PRAMs and polymorphisms for the time periods of before and after the introduction of PIs in the Asia region were also investigated (Figure 1). ▪ The correlation between each pair of polymorphisms was investigated (Table 1). There were eight positive correlations and three negative correlations (all with P <0.05). ▪ Intersubtype genetic differences and the genetic background of the infected host population can also influence PI susceptibility and viral replication capacity (Hirsch 2008). OBJECTIVE ▪ To investigate how CRF01_AE protease polymorphisms and protease resistanceassociated mutations (PRAMs) have been affected by the introduction of antiretroviral therapy and the frequency of HLA haplotypes in studied populations (Thai and Chinese). METHODS ▪ All HIV-1 CRF01_AE pro sequences were downloaded from the Los Alamos National Laboratory database on April 28, 2008. ▪ The recombinant identification program, RIP 3.0 (available at http://lanl.gov/), was used to identify and confirm subtype and presence of recombination in retrieved sequences. ▪ The dataset was checked for uniqueness using the UNIX command “uniq” and sequences were aligned using Multiple Sequence Comparison (Edgar 2004). ▪ Geneious Basic version 3.7.1 software (Biomatters Ltd., Auckland, NZ) was used to construct a neighbor-joining tree using the Jukes-Cantor 69 method for phylogenetic analysis. ▪ HYPERMUT 2.0 and Epitope Location Finder (available at http://lanl.gov/) were used to detect APOBEC-induced hypermutation and searched CTL recognized epitopes from viral amino acid sequences by using sequence code 01_AE.AU.X.CT1 as a reference sequence (Rose and Korber 2000). Figure 2. Logistic regression analysis of major PRAMs and each polymorphism Figure 1. Frequencies of major PRAMs and polymorphisms by time period 1990-2000 (n=188) L76V 2001-2007 V77I No data (n=263) D30N P olymorphis ms 1990-2000 L33V 2001-2007 (n=537) OR No data I62V N88S 10.955 P = 0.031 2.6% 0.5% I84V V82I I54VA I93L 4.263 2. 585-7. 032 6.460 3. 972-10. 505 L10V M46IL 4.8% 2.0% P = 0.067 K20RMI V82AFMS I13V 85.6% L90M M36I 95.2% 0 10 20 30 40 Number Frequencies of PRAMs 0 76.3% 87.1% P = 0.007 -10 A dju s t e d o dd s r a t io s U n a dju s t e d o d ds r a t io s * 0 10 20 30 P < 0.001 40 50 60 O d d s ra t io a n d 9 5 % c o n f id e n c e in t e rv a l (C I) Number Figure 3. Associations between HLA haplotypes and polymorphisms Figure 4. Predicted fold changes of HLA class I binding affinities from the eptiope of subtype B consensus to CRF01_AE B: E EM NLPGRW AE: E DINLPGKW Protease Epitope position: 34-42 HLA Allele: B*4001 0 34-42 B*4430 34-42 34-42 30-38 30-38 11-20 12-20 B*4402 B*1801 A*6802 A*6801 A*0301 A*0301 3.0 2.4 4.9 4.1 -20 18.9 26.7 -30 -40 36.5 39.7 ▪ There were no substantial differences in hydrophobicity or chemical classifications of these residues between subtype B and CRF01_AE consensus sequences (Table 2). CONCLUSION Polymorphisms in CRF01_AE protease gene are common with M36I being the most frequent. Polymorphisms at residue 10, 20 and 62 were associated with major PRAMs and therefore PI use, while R41K and H69K variants are more likely attributable to recognition of epitopes by the HLA haplotypes in the population. Additionally, protease function most likely requires maintaining the same biochemical properties at these residues. Negative correlation Polymorphic mutation Correlation coefficient P value Polymorphic mutation Correlation coefficient P value 10 and 62 0.154 <0.001 20 and 36 -1.333 <0.001 20 and 62 0.140 <0.001 13 and 93 -0.400 <0.001 20 and 93 0.125 <0.001 10 and 93 -0.089 0.005 60 and 93 0.104 0.001 10 and 20 0.095 0.003 77 and 93 0.094 0.003 10 and 13 0.004 0.093 13 and 82 0.069 0.030 Table 2. Hydrophobicity and chemical classifications of six different residues Residue Subtype B Hydrophobicity* Chemical classifications Subtype AE Hydrophobicity* Chemical classifications 13 I 1 Aliphatic group V 1 Aliphatic group 35 E 4 Negative charge D 4 Negative charge A*0101 36 M 2 Sulphur containing group I 1 Aliphatic group 1.1 41 R 5 Positive charge K 4 Positive charge 69 H 4 Positive charge K 4 Positive charge 89 L 1 Aliphatic group M 2 Sulphur containing group B: DTVLEE M NL AE: DTVLEE INL -10 A positive HLA-polymorphism association was defined as expression of a subtype B consensus residue that would be expected during CTL escape with the HLA allele expression in the study population. A negative HLA-polymorphism association was defined when expression of the CRF01_AE consensus residue was associated with HLA expression and CTL escape. ▪ The nine HLA-polymorphism associations with the largest changes in predicted binding affinity are presented in Figure 4. Positive correlation 100 200 300 400 500 600 700 800 900 Frequencies of polymorphisms ▪ At five residue sites, 30 HLA-polymorphism associations were found, distributed among 11 (37%) HLA-A, 17 (56%) HLA-B and 2 (7%) HLA-C haplotypes (Figure 3). Of these associations, 24 (80%) were positive correlations (i.e. the subtype B consensus amino acid was favored) and 6 (20%) were negative correlations. Table 1. Correlations among each pair of polymorphisms P = 0.002 ▪ The prevalence of specific HLA alleles in the populations studied (Thai and Chinese) were obtained from the dbMHC database of the National Center for Biotechnology Information (http://www.ncbi.nlm.nih.gov/projects/gv/mhc). ▪ Spearman correlations and logistic regression models were used for further analyses. 3. 236-37. 092 D60E ▪ PRAMs and polymorphisms were identified based on data derived from clade B virus using the Stanford Resistance Database (http://hivdb.stanford.edu/). ▪ HLA binding affinities were determined using the Immune Epitope Database and Analysis resource (IEDB, www.immuneepitope.org) by stabilized matrix method. I9 3 L V 82I V 77I *I6 2 V I6 2 V D 60E M 36I M 36I L33V *K 2 0 R M I K 20R M I I1 3 V *L 1 0 V L10V 95%CI Fold changes ▪ Continued viral replication in the setting of PIs allows for the development and accumulation of accessory mutations in HIV pro, which can compensate for impaired fitness conferred by other mutations or can increase the level of phenotypic resistance (Hirsch 2008; Johnson 2008). ▪ 4 polymorphisms had an association with a PRAM with P values <0.2 in Fisher’s exact test univariate analysis. In multivariate analysis, three of four polymorphisms were associated with the presence of a major PRAM (P <0.05) (Figure 2). 7-15 * Hydrophobicity 1 to 5 = from the highest hydrophobicity to the least hydrophobicity Acknowledgement: The authors would like to thank The University of California, San Diego Center for AIDS Research (UCSD CFAR) for their support. This work was supported by grants AI69432 (ACTG), AI043638 (AIEDRP), MH62512 (HNRC), MH083552 (Clade), AI077304 (Dual Infection), AI36214 (the Viral Pathogenesis Core of the UCSD Center for AIDS Research), AI047745 (Dynamics), AI74621 (Transmission) from the National Institutes of Health and the California HIV/AIDS Research Program RN07-SD-702.