Nursing Assistant
advertisement

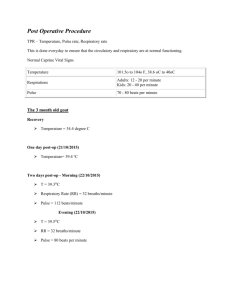
Nursing Assistant Vital Signs Vital Signs Temperature Pulse Respiration Blood pressure Oxygen saturation Pain Vital Signs Indicators of body function – Assess body systems – Signify changes taking place in body Observations should also include – Skin color & temp – Behaviors – Statements from resident (subjective) Temperature Balance of heat gained & heat lost Hypothalamus is temp regulation center Heat produced by – Cellular activity • Infection elevates temp • Brain injury can increase or decrease temp – Food metabolism – Muscle activity • Exercise elevates temp – Hormones – External factors – heat, hot drinks, warm clothing – Internal factors - dehydration Temperature Heat lost from body by – Skin • Sweating • Increased blood flow to skin surface – Lungs • Increased resp rate – Elimination • Urine or feces Temperature Heat conserved by body through – Reducing perspiration – Decreasing flow of blood to skin – Shivering • Increases muscle activity & produces heat Temperature Norms Adult 97 – 99 degrees Fahrenheit – Oral – 98.6 – Rectal – 99.6 – Axillary – 97.6 – Tympanic – 98.6 Temperature procedure Wear gloves Shake mercury down below 96 If smoked or had something to drink, wait 10 min Insert thermometer, wait…. – Oral – under tongue, 5 minutes – Axillary – in armpit, 10 minutes – Rectal – in rectum, 3 minutes Contraindications for oral temps Confused, disoriented Restless Unconscious Coughing, unable to breathe through nose Seizures Oral/nasal oxygen NG Contraindications for rectal temps Diarrhea Fecal impaction Rectal bleeding Hemorrhoids Surgical rectal closure When doing rectal temps, remember – – – – Lubricant before inserting thermometer Insert 1 – 1 ½ inches Hold thermometer in place NEVER leave resident Nursing measures Raise temperature – – – – Increase thermostat in room Add blankets or clothing Give hot or warm liquids to drink Give warm baths or soaks Lower temperature – – – – Lower thermostat in room Remove clothing or blankets Offer cool liquids to drink Provide cool or tepid bath or sponge Pulse Force against the arterial walls that cause them to expand with each heartbeat Count for one minute Norm adult pulse is 60 –100 beats/min – < 60 beats/min = bradycardia – > 100 beats/min = tachycardia Major pulse sites Carotid – neck Apical – left chest below nipple (need stethescope) Brachial – inner aspect of elbow Radial – thumb side of wrist Femoral – groin Popliteal – behind knee Posterior tibialis – behind inner ankle Dorsalis pedis – on top of foot Factors that increase pulse Exercise Strong emotions – fear, anger, laughter, excitement Fever Pain Shock Hemorrhage Factors that decrease pulse Sleep/rest Depression Drugs – digitalis, morphine Athletes in good physical condition may have a lower pulse, probably <60 beats/min. This is normal Qualities of pulse Rate – number of beats/min Rhythm – regularity of pulse Strength – force – Weak or thready – Bounding – Strong Respiration Exchange of oxygen & carbon dioxide in lungs 1 respiration = 1 inhalation + 1 exhalation Regulated by the medulla Normal adult rate is 16 – 20 breaths/min Normal breathing is quiet, effortless, & regular in rhythm Qualities to observe for Resp Rate Rhythm Depth – shallow, norm, deep Effort involved to breathe Discomfort it causes Position resident adopts Sounds that accompany it Color of skin, mucous membranes, nailbeds – check for cyanosis Abnormal breathing Labored – struggles to breathe Orthopnea- can breathe only when sitting or standing Stertorous – snoring sounds when breathing (partial airway obstruction) Abdominal – uses abd muscles Shallow – uses only upper part of lungs Dyspnea – painful or difficult breathing Tachypnea – resp rate > 24 per min Bradypnea – resp rate < 10 per min Apnea – absence of breathing Cheyne-Stokes – resp gradually increase in rate & depth & then become shallow & slow Process of taking TPR Take temperature first Pulse second Respirations last When taking resp, keep fingers on pulse so that resident does not know you are counting resp Document all together Blood pressure Pressure exerted against walls of blood vessels – Systolic – highest reading • Pressure when heart contracting – Diastolic – lower reading • Pressure when heart is at rest Hear thumping sounds as blood flows through arteries – Sounds correspond to numbers representing mm Hg on sphygmomanometer – First sound heard is systolic – Last sound heard is diastolic Blood pressure Normal adult reading 120/80 Normal systolic = 100 – 140 Normal diastolic = 60 – 90 Abnormal readings – Hypertension – BP > 140/90 – Hypotension – BP < 90/60 Factors increasing BP Strong emotion Exercise Sitting or standing Excitement Pain Decrease of vessel size Digestion Improperly placed or sized cuff Factors decreasing BP Rest/sleep Lying down Depression Shock Hemorrhage Improperly sized cuff Equipment for BP Sphygmomanometer Cuff Stethescope Cuff too narrow gives false high Cuff below heart level will give false high Cuff too large or improperly placed can give false low Procedure for BP Guidelines – – – – – – – Measure BP at brachial artery Do not use injured arm, arm with IV, or casted Resident should be at rest Position arm level with heart Apply cuff to bare arm NOT over clothing Use appropriate size cuff Position sphygmomanometer at eye level Pain Ask resident if they have pain Observe facial expression, movement, respiration Ask level of pain using facility method (Usually number 0 – 10) Report c/o pain to licensed nurse Charting VS Report norm & abn to licensed nurse Record on flow sheets, graphic records, & NA notes according to facility Record in TPR order Chart rectal temps with “R” Chart axillary temps with “Ax” Pulse readings other than radial are noted If BP in a place other than arm,note location Write BP on chart as a fraction