Lymphoid System Function of immune system Protection from
advertisement

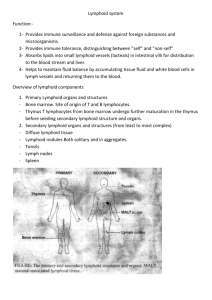
Lymphoid System Function of immune system - Protection from invasion by foreign organisms - Protection from abnormal cells (e.g. neoplasia) or substances Innate immunity - Inflammatory response Occurs at site of infection Rapid and nonspecific response o Responds to certain type of injury o Responds to features shared by certain type of pathogen Mediated by various cell types o Neutrophils, eosinophils, and macrophages o Natural killer (NK) and mast cells Acquired immunity - Slow, precise response - Mediated by lymphocytes and lymphoid tissues Lymphocytes circulate through blood, lymph, and tissue o Involved in immunosurveillance Monitoring body for the presence of foreign substances, cancers and other potentially harmful substances (bacteria, viruses, fungi) o Can circulate for years before activation nucleus to multiply o Has greater potential than mechanism of innate immunity (leukocytes leave blood for tissue and remain in tissue for a limited amount of time) - Primary cells of lymphoid system B and T lymphocytes Support cells o Antigen presenting cells (APCs) o Specialized epithelial cells and stromal cells Facilitate immune response to antigen Provide appropriate environment in which immune reactions occur - Specificity Each lymphocyte has membrane receptors specific for a specific region (epitope) on a foreign macromolecule (antigen) o Antigen Molecule that triggers the production of antibody when introduced into body Can trigger formation of cells designed to kill foreign/infected cells (tumor cells) o Epitope Composed of a series of amino acids (1-6) and/or a sugar moiety Small antigens may have only 1 epitope Large antigens may contain many different epitopes Although T lymphocytes have receptors designed for a specific epitope, they require assistance from cells known as antigen presenting cells (APCs) Slow response time o Slow b/c lymphocytes must travel throughout the body to find specific epitopes. Once they meet, it takes time for the initially-quiescent lymphocytes to become activated and respond to the threat by proliferating and producing either antibodies or regulatory cytokines Reaction takes place in secondary lymphoid organs o Include lymph nodes, spleen, tonsils and mucosal associated lymphoid tissue (MALT) - Adaptation First interaction with antigen triggers blastogenesis and clonal expansion o After antigen activation, B and T cells “turn on” nucleus and synthetic mechanisms Nucleus becomes larger with increased numbers of polyribosomes and other organelles associated with protein synthesis and mitosis Nuclear chromatin becomes lighter in color (euchromatin) Many lymphoblasts (large lymphocytes) have prominent nucleolus In blastogenesis, activated lymphoblasts undergo clonal expansion (proliferation), producing more lymphocytes with the same specific antigen receptor o Lymphocytes formed after antigenic stimulation undergo differentiation Although lymphocyte nuclei are not active all the time, they have the potential to be stimulated. When this happens, the nuclear chromatin will change from heterochromatin to euchromatin. By contrast, granulocytes are terminally differentiated and do not have the ability to reactivate their nuclei Can become memory cells o Long-lived, small, little cytoplasm, inactive heterochromatin Can become effector cells Produces plasma cells (antibody factories) “Army” of memory cells is primed and ready to react o Second infection results in faster and stronger response This is the basis for vaccination: injecting molecules from an infectious agent activates lymphocytes and the production of antibodies and memory cells that can respond quickly to subsequent exposure to that infectious organism. In other words, animals already will have the machinery for fighting the infection - Discrimination (self from non-self) - Memory Cells of Acquired Immunity - Lymphocyte development Lymphocyte precursors arise from pluripotent stems cells in marrow that commit to becoming different types of cells, which are not yet immunocompetent o Commit to becoming B cell, T cell, or NK cell Immunocompetence o Lymphocytes that are able to distinguish self from non-self substances and able to react to the presence of foreign antigens - B lymphocytes Develop in cloacal bursa (birds) Develop in bursa-equivalent organs like bone marrow and GALT of ileum (mammals) Involved in humoral immunity o Production of antibodies (immunoglobulins) Antibodies on B cell membrane act as receptors for specific antigen epitopes Each naïve B cell has many copies of unique antibody on its surface - Plasma cells (effector B cells) Form from activated B cells Primary function is antibody production Histological appearance o Moderate to large amount of cytoplasm o Eccentric nucleus o Dark, clumped chromatin o +/- pale golgi zone - Antibodies Secreted into blood and tissue fluids by plasma cells Large, Y-shaped protein o Binding sites at the two tips of the “Y” specifically recognize and bind to target antigen Functions o Promote attack by phagocytes o Bind to foreign toxin to promote its clearance from the body o Binding to pathogen may prevent it from infecting cells via neutralization o Activation of complement can lead to lysis of pathogen or infected cell - T lymphocytes Develop in the thymus - - - - - ~70% of circulating lymphocytes Long lifespan (years) Subsets o Helper T cells Activate B cells and promote humoral response o Suppressor T cells Suppress the immune response o Cytotoxic T cells (effector cells) Involved in cell-mediated immunity Kill infected or neoplastic cells Require antigen to be presented on the surface of APCs Antigen-presenting cells (APCs) Includes several cell types o B lymphocytes o Dendritic cells o Macrophages (e.g. Kupffer cells in liver) o Epithelioreticular cells (in thymus and cloacal bursa) Phagocytose and process antigens o Break antigens into small peptides, which are returned to the cell surface in such as way that a specific T lymphocyte will be stimulated Dendritic cells Most efficient APCs o Only present to T-cells (not B-cells) Active in capture, uptake, and processing of antigens Generally found in various tissue throughout the body but return to the secondary lymphoid tissue (e.g. regional lymph node), where they lose the ability to process antigen and gain the capacity to interact with naïve T lymphocytes Not seen in routine H&E stains Langerhans cells Derived from monocyte precursor APCs of skin Special intra-epidermal dendritic cells o Interdigitated between keratinocytes o Mop up invaders that penetrate skin Not readily identified in a routine H&E stained histologic section of skin Macrophages Derived from monocyte precursor Inefficient at antigen presentation Functions o Lymphocyte activation APC function and cytokine secretion o Inflammation Cytokines induce acute phase response, fever, and inflammation o Tissue reorganization Secrete important factors o Elastases, collagenases, FGF, angiogenesis factors o Micobicidal activity o Tumor immunity Secrete toxic factors, free radicals, hydrolases, and TNF- a Stromal cells Fixed cells that act as supportive scaffolding for other cells of the immune system Reticular cells (mesenchymal, CT) o Predominant stromal cells of most lymphoid organs (lymph nodes, spleen, MALT) o Produce type III collagen (reticular fibers) o Express surface molecules and substances that attract lymphocytes and dendritic cells Epithelioreticular cells (epithelial) o Stromal cells of thymus and cloacal bursa o Have long cytoplasmic processes with desmosomal attachments (stellate appearance) o No reticular fiber formation Lymphoid Tissue Organization - Lymphoid tissues are divided into primary and secondary organs Primary lymphoid organs o Populations of lymphocyte precursors from bone marrow o Provide specialized environment where lymphocytes proliferate, develop and are educated Lymphocytes gain machinery for antigen recognition (unique antigen receptors) Self-reactive lymphocytes are eliminated T cell education in thymus B cell education varies with species o Bone marrow (primates, rodents) o Cloacal bursa (birds) o Peyer’s patches of distal ileum (ruminants, carnivores, pigs) o Spleen (maybe reptiles) o Lymphocytes are immunocompetence but naïve (never encountered antigen) o Organs typically involutes after sexual maturity Immunosurveillance o Antigens are carried to the lymph node by dendritic cells as soluble compounds o Naïve, immunocompetent lymphocytes “examine” antigens at node If do not encounter specific antigen, lymphocytes move on If they do encounter antigen, lymphocytes are activated (antigenic stimulation) o Proliferation of a group of cells with identical antigen receptors (clones) o Activated B cells will produce plasma cells and memory cells o Activated T cells can strengthen or suppress B cell response o Lymphocyte production takes place in lymphoid tissues where antigenic stimulation occurs Secondary lymphoid organs o Populations of immunocompetent lymphocytes that form organs Tonsils Lymph nodes Spleen Mucosal associated lymphatic tissue (MALT) o Peyer’s patches of the ileum (gut-associated lymphoid tissue – GALT), o Lymphoid tissue of respiratory tract (bronchiolar-associated lymphatic tissue – BALT) o Can produce both humoral and cell-mediated responses to antigens o General architecture Diffuse lymphoid tissue portion (interfollicular tissue) o Unorganized collection of lymphocytes and other free cells Lymphoblasts, macrophages, plasma cells o Primarily T cell zone o Supported by stroma composed of dendritic cells and CT o Found in the lamina propria of many organs where it is often transient o Permanent in lymphatic organs o After contact with an antigen, activated lymphocytes travel regional lymph nodes where it undergoes blast transformation and proliferates. Its progeny return to the lamina propria as effector B and T lymphocytes Nodular lymphoid tissue portion (organized) o Primarily B cell zone o Always surrounded by diffuse tissue (T cells) o o o o o o Dispersed dendritic cells Supported by reticular cells Primary nodules (follicles) Tightly-packed, small lymphocytes Primarily naïve B cells Secondary nodules Sign of antigenic stimulation – lymphocytes that recognize an antigen return to a primary nodule and undergo proliferation Germinal center containing lymphoblasts Blastogenesis and clonal expansion occur Lighter appearance due to euchromatin of blasts Mitotic figures common Mantle zone (corona) Dark, outer ring of naïve lymphocytes that failed to encounter their antigen Usually oriented toward the source of antigen (e.g. the tonsilar mantle zone is pronounces near the oral cavity) Encapsulated Thymus (primary lymphoid organ) Lymph nodes Spleen Tonsils (partially) Non-encapsulated Other MALT GALT BALT Primary Lymphoid Organs - Thymus Primary organ responsible for the education of T lymphocytes Architecture o Epithelioreticular cells form the framework of the organ that is then seeded with developing lymphocytes from the bone marrow o Divided into lobes by thin, CT capsule o Lobes divided into lobules by CT trabeculae o Capsule and trabeculae contain blood vessels, nerves, and only efferent lymphatics o Each lobule has 2 parts Cortex (outer layer) o Darkly-stained due to more developing T cells (thymocytes) Medulla (inner layer) o Pale-colored because has fewer thymocytes and more stromal cells Vascular supply o Trabeculae carry blood vessels, nerves, and efferent lymphatics o Arteries enter at the corticomedullary junction and divide into arterioles that course along the junction and give rise to a capillary network in the cortex o Capillary network in cortex forms blood-thymus barrier May prevent foreign antigens from entering the thymus in an uncontrolled fashion o Capillaries drain into postcapillary venules in the medulla o Postcapillary venules joins veins to carry blood out of the thymus T Lymphocyte education o T cell precursors enter cortex from bloodstream (bone marrow) o T cells are “tested” twice by epithelioreticular cells in the cortex and medulla If pass cortex test, cells migrate from cortex to medulla If pass medulla test, cells migrate to 2° lymphoid organs If fail medulla test, cells apoptose (~98%) and are phagocytosed by macrophages o May fail if bind self-antigens or are poorly-reactive Epithelioreticular cells o Only found in thymus and cloacal bursa (presence can help identify organ) o Sheets of cytoplasm surround and support T lymphocytes Large, light-staining nuclei o Several types, each with a different function o Thymic (Hassall’s) corpuscles (type VI cells) Closely-packed, flat keratinized cells Thymic corpuscle in concentric arrangement May produce interleukins that facilitate differentiation and education of T lymphocytes Thymic involution o After sexual maturity, most of the thymus is replaced with adipose and CT tissue o Level of involution is species specific o Residual epithelioreticular cell proliferation can give rise to a thymoma in geriatric adults Tumors often contain large numbers of T lymphocytes that are not neoplastic - Cloacal bursa – “bursa of fabricius” (birds) Primary lymphoid organ for maturation and education of B cells in birds Blind sac in dorsal wall of cloaca with invaginations of simple, columnar epithelium Architecture similar to thymus o Lobes separated into lobules by surface epithelium (not capsule) o Lobules separated by trabeculae Have both cortex and medulla Epithelioreticular cells promote lymphopoiesis (differentiation of B cells) Bursa atrophies after about six months - Peyer’s patches (young ruminants, pigs, and carnivores) Large aggregate of submucosal lymphatic nodules in the distal ileum o Each nodule has cortex and medulla o Rich in B cells Responsible for diversification of pre-immune antigen-receptor repertoire Removal of this lymphoid tissue before birth causes immunodeficiency o Decreased number of mature B cells Involutes after sexual maturity - Bone marrow Primary source of B and T cell precursors Primary organ for differentiation and education of B cells in primates and rodents B-cell precursors start out near endosteum of bone Differentiation and selection proceeds as cells migrate toward venous sinuses Secondary Lymphoid Organs - Tonsils Aggregates of lymphoid nodules at entrance to oropharynx Covered various types of epithelium depending on the location o Palatine (either side of pharynx) Non-keratinized stratified squamous Surface epithelium is often smooth (in dog) Surface epithelium can form deep invaginations (tonsilar crypts) that increase the SA and maximized antigen-lymphocyte interactions (horses, ruminants, pigs) Organ separated by distinct CT capsule Lack afferent lymphatics Lingual (base of tongue) Non-keratinized stratified squamous o Pharyngeal (wall of nasopharynx) Pseudostratified ciliated columnar Mantle of each nodule is more prominent on side closest to epithelium (on side that faces where the antigen is coming in. In the case of tonsil, it will face the oral cavity) Lymphocytes migrate into epithelium to sample antigen at mucosal surface (dark nuclei here) Peyer’s patch 30-50 aggregated nodules along length of intestinal mucosa (digestive tract) Most numerous in caudal ileum Cause gross elevation in mucosa Different function and morphologic appearance compared to the primary organs o Germinal center of B cells o Mantle zone facing intestinal mucosa o Interfollicular area rich in T cells o Dome area Dense region of dendritic cells immediately beneath the epithelium o Epithelium over dome Less well-developed microvilli No goblet cells Scattered M (microfold) cells o Modified enterocytes designed for antigen-transport and presentation Microfolds rather than microvilli on apical (luminal) surface Pinocytose particulates in lumen Antigen presented to lymphocytes in pockets on basolateral side o - Primary lymphoid organ Secondary lymphoid organ - Lymph node Increased number of lymph nodes found in certain areas of body (e.g. axilla, groin) Architecture o Bean-shaped o Surrounded by dense CT capsule that sends trabeculae (carries vessels and nn.) into cortex o Afferent lymphatics pierce capsule o Efferent lymphatics leave at hilus o Blood vessels enter and leave at hilus o Cortex Superficial (nodular) cortex (outer) 1° and 2° lymphatic nodules with germinal centers (B cell rich) separated by diffuse lymphatic tissue (T cell rich) Paracortex (deep, inner) o Diffuse lymphatic tissue (primarily T cells) o Medulla Has distinct cords and sinuses o Represented by large spaces (will not see this in other lymphoid organs) Lymph flow o Afferent lymphatics pierce capsule and drain into subcapsular sinuses, which lead to trabecular sinuses, which lead to medullary sinuses, which form a network of anastomosing channels that converge at hilus and open into the efferent lymph vessels Sinuses o Lined by flattened endothelial cells that form continuous lining adjacent to CT capsule o Discontinuous endothelium adjacent to lymphatic parenchyma Allows lymphocytes and macrophages to access sinus Allows lymph to pass into parenchyma o Macrophages hunt for antigen o Reticular cell processes and fibers slow movement of lymph and facilitate interactions between antigen and cells as well as the phagocytic activities of macrophages Metastatic cancer may be trapped in these sinuses and destroyed However, large numbers of cancer cells may overwhelm the immune system, establishing a new metastatic site in the lymph node Blood and lymph flow o Arteries enter at hilus, travel through medullary cords, and form capillary beds in cortex o Capillaries extend into paracortex and they form unique postcapillary venules High endothelial venules (HEVs) o Lined by tall, simple cuboidal endothelium o Join veins in medullary cords (trabeculae) o Drain into veins that exit at hilus o Express receptors for naïve lymphocytes or memory cells HEVs bind lymphocytes, inducing them to leave circulation and migrate into the lymph node o Most lymphocytes enter node via the HEV of the deep cortex (~90%) Only small numbers enter via lymphatics Lymphocyte traffic pattern o Lymphocytes percolate through sinuses o Those entering through HEVs first migrate to superficial cortex o During this process, they engage in immunosurveillance Immune response o B cell response Lymphoblasts migrate from germinal center to medullary cords and differentiate Differentiated plasma cells secrete antibodies into medullary sinuses o T cell response T cells proliferate and differentiate in paracortex Cytotoxic T cells leave via efferent lymphatics o - Spleen Functions o Protection against blood borne infectious agents and other antigens Production of lymphocytes Filters pathogens and antigens o Storage of RBCs and platelets (can be very useful in emergency injury and blood loss) o Destruction of senescent and abnormal RBCs o Recycles iron Hematopoiesis Especially important in fetus Can back up bone marrow General architecture o Capsule (thick CT) Amount of smooth muscle varies with species (large amounts in dog and horse) o Splenic blood flow Splenic artery enters at hilus and branches into trabecular arteries (run within trabeculae CT), which then branch into individual central arteries (really arteriole) Central artery sends branches to the lymphatic nodules and marginal sinuses The marginal sinus is where blood borne antigens will first contact lymphoid cells Some capillaries are surrounded by macrophages and reticular cells o Sheathed capillaries (ellipsoids), periarterial macrophage sheaths (PAMS) Important for clearing blood-borne infections Large and abundant in cat and pig spleens o Parenchyma of spleen is known as “splenic pulp” White pulp o Lymphoid cells that appear “white” upon gross examination Histologically stains blue o Organized to maximize interaction b/w antigens and immune cells o Nodular and diffuse lymphoid tissue organized around arteries o Periarteriolar lymphatic sheath (PALS) Sleeve of lymphocytes surrounding central artery T cells predominate near vessel Red pulp o Bulk of spleen volume o Organized to promote RBC and macrophage interactions o Pulp cords, sinuses, and venules Network of reticular fibers that slows blood flow Variety of cells present Reticular cells, RBCs, macrophages, lymphocytes, plasma cells, other leukocytes Capillaries extending into red pulp lack lymphoid sheath Marginal zone o Zone between white and red pulp o Contains marginal sinus o Supplied by capillaries from white and red pulp o Because the spleen lacks HEVs and afferent lymphatics, lymphocytes migrate into the spleen from capillaries in the marginal zone Sinusoidal spleen (dogs, primates, rodents) Central artery branches into venous sinusoids lined by discontinuous endothelium Red pulp contains sinuses lined by longitudinal endothelial cells with bands of basal lamina Two mechanisms for removing abnormal RBCs o Endothelial cells effectively trap defective RBCs and act as a mechanical filter Can pinch off RBC membrane defects (RBC pitting) Can prevent their re-entry into circulation o When remove spleen from dogs, often see increased number of defective RBCs o Macrophages within reticular meshwork red pulp Act as a biological filter, recognizing and removing old or damaged RBCs Can possibly change from open to closed circulation (depends on situation) o Terminal capillaries connect directly to sinuses (closed) o Terminal capillaries empty into and must cross a network of splenic reticular meshwork before entering sinues (open) o - - Non-sinusoidal spleen (cat, horse, ox, pigs) Pulp venules (nonanastomosing, short, thin-walled) are open-ended vessels that originate in the reticular meshwork near trabeculae and drained into trabecular veins Wider splenic cords that lack splenic sinuses Strictly open circulation One mechanism for removing abnormal RBCs (macrophages) o Without endothelial cell barrier, this spleen is less effective at removing abnormal RBCs