MALE GENITOURINARY ASSESSMENT
advertisement
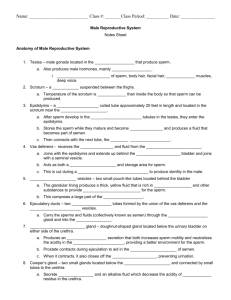
ASSESSING THE MALE GENITOURINARY SYSTEM Outcomes Identify pertinent male genitourinary history questions. Obtain a male genitourinary history. Perform a male genitourinary physical assessment. (Continued) Outcomes Document pertinent male genitourinary assessment findings. Identify actual/potential health problems stated as nursing diagnosis. Differentiate between normal and abnormal findings. (Continued) Structures Scrotum Spermatic cord Vas deferens Epididymis Ureter Penis & glans Bulbourethral gland Testes Seminal vesicle Prostate Kidney Bladder Inguinal Area Urethra & meatus (Continued) Functions What are the functions of… Scrotum: Sac that contains testes Testes: Produces sperm and testosterone Vas deferens: Duct from epididymis to ejaculatory duct (Continued) Functions What are the functions of… Spermatic cord: Protective sheath around the vas deferens Seminal vesicles: Produce 70% of semen Bulbourethral gland: Secretes alkaline substance to neutralize vaginal secretions (Continued) Functions What are the functions of… Prostate: Produces 20% of semen Epididymis: Stores sperm until it is mature Kidney: Filters blood and removes wastes (Continued) Functions What are the functions of… Ureter: Tube connecting kidney to bladder Bladder: Hollow, muscular structure, holds urine Urethra: Passageway for urine (Continued) Functions What are the functions of… Penis: Male sex organ and urine elimination Glans penis: Important for sexual arousal (Continued) Functions What are the functions of… Inguinal area: Canal for vas deferens from scrotum through the abdominal muscles, inguinal lymph nodes Male Reproductive Organs Male Development History What can the history tell you about the male genitourinary system? Biographical data Current health status Past health history Family history Review of systems Psychosocial history Symptoms What symptoms would signal a problem with the male genitourinary system? Genital pain Lesions Genital swelling Penile discharge Urinary symptoms Physical Assessment Anatomical landmarks: external--note position of structures; internal-visualize underlying structures Approach: inspection, palpation Position: standing or supine, leaning over table or Sim’s position (Continued) Physical Assessment Tools: gloves, lubricant, pen light, slides & swabs for specimen collection, and stethoscope General survey and head-to-toe scan Inspection Penis: condition of skin, color, lesions, discharge, size, position of urinary meatus, foreskin Scrotum: size and position, color, hair distribution, lesions, swelling, pediculosis Inguinal area: condition of skin, bulges Rectal area: condition of skin, lesions, hemorrhoids, polyps, fissures, bleeding Palpation Penis: consistency, tenderness, masses, discharge Scrotum & testes: size, shape, symmetry, mobility, tenderness, masses Epididymis: swelling, tenderness, nodules Palpation Inguinal area: hernias, lymph nodes, tenderness Anus & rectum: sphincter tone, tenderness, lesions, masses, hemorrhoids, polyps, test any stool for occult blood Prostate: size, shape, symmetry, mobility, consistency, nodules, tenderness, grade size Auscultation Inguinal area: bowel sounds Nursing Diagnosis What actual or potential problems can you identify for Mr. Richards?