Chapter 5 Coronary Heart Disease

Chapter 5
Coronary Heart Disease
P-96
CHD is usually a disease of high-income countries, but also in low and middle-income countries.
Recorded history of CHD dates to AD 150.
Children, mummies, etc. CHD #1 cause of mortality of mankind.
Angina Pectoris---chest pain due to lack of O2 (in blood).
Heart disease (CHD, hypertensive heart disease, rheumatic heart disease is the # 1 cause of mortality in the USA since the
1920’s.
Rheumatic heart disease is the most dreaded complication of rheumatic fever . The term "rheumatic heart disease" refers to the chronic heart valve damage that can occur after a person has had an episode of acute rheumatic fever. This valve damage can eventually lead to heart failure .
Reduced smoking by adults, better hypertension meds, greater public awareness about a healthy diet and better medical treatment have all helped lower the % of mortality from heart disease.
Currently, about 17.6 million people from age 20 to older in the USA have CHD.
The annual # of CHD deaths is about 425,000. About every 25 seconds an American will have a cardiac event and about every 60 seconds one American will die from it.
CHD Risk Factors
Major risk factors for CHD: genetic susceptibility, male sex, elevated serum cholesterol, low levels of HDL, smoking, high BP, obesity, diabetes and being sedentary.
Contributing factors include: inflammation abnormalities in regulatory proteins of the hemostatic system (blood clotting) & possibly elevated homocysteine (associated with vascular injury).
CHD Etiology
Starts with atherosclerosis which is a form or arteriosclerosis—characterized by atheromas (fatty deposits)—which contribute to narrowing of med to large arteries.
Thrombosis—clot formation.
Ischemia—blockage/shortage of blood and O2.
All this begins in childhood---due to level of cholesterol (& type). LDL increases this where HDL retards it. Smoking, high BP and high intake of sat fat and cholesterol increase the chance. In contrast, physical activity decreases risk via its positive effects on LDL through HDL and reducing BP.
Atherogenesis
Begins with lesion of the intima (innermost lining) of coronary artery. This injury is from damage to endothelium—could be physical or from smoking.
Atherogenesis
: “
Formation of atheromatous deposits, especially on the innermost layer of arterial walls.” “The formation of subintimal plaques in the lining of arteries.”
atheroma /ath·er·o·ma/ (ath″er-o´mah) a mass or plaque of degenerated thickened arterial intima, occurring in atherosclerosis.
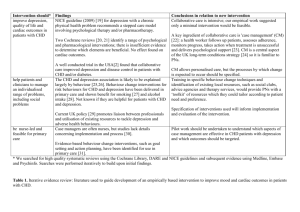
Picture on P-98.
Renegade LDL contributes to atheromas are free radicals. (P-97).
Inflammation (P-98): Atherosclerotic disease involves inflammatory processes. Major risk forctors for CVd including dyslipidemia, hypertension, diabetes and obesity all have pro-inflammatory features, as do bacterial and viral infection.
The anti-inflammatory effect of physical activity may be mediated through beneficial changes in body weight.
C-reactive protein ( CRP ) is a protein found in the blood, the levels of which rise in response to inflammation (i.e. C-reactive protein is an acute-phase protein ). Its physiological role is to bind to phosphocholine expressed on the surface of dead or dying cells (and some types of bacteria) in order to activate the complement system via the C1Q complex .
C-reactive protein , or CRP , a sign of inflammation and potential risk factor for heart disease .
Hemostasis : (factors that regulate blood clotting) are risk factors for CVD.
Hematocrit : (the % of blood volume occupied by cells) is a risk factor for CVD. High hematocrit is associated with increased blood thickness and coagulability ( characteristics which increase the contacts between platelets and endothelial cells which can promote aggregation.
Blood clotting factors are associated with increased risk of ischemic heart attack and stroke— people who are active tend to have lower levels of clotting factors.
Homocysteine : Homocysteine is a common amino acid (one of the building blocks that make up proteins) found in the blood and is acquired mostly from eating meat. High levels of homocysteine are related to the early development of heart and blood vessel disease. In fact, it is considered an independent risk factor for heart disease. High homocysteine is associated with low levels of vitamin B6, B12, and folate and renal disease. Research has shown, however, that reducing your homocysteine levels with vitamins does not reduce the risk of heart disease.
Physical Activity and CHD
P-100
On average, physical activity cuts risk of CHD by 30% to 40% for both men and women.
Occupational Activity and CHD Risk: Studies include—San Francisco Longshoremen; Railroad switchmen and Israeli workers.
Leisure-Time Physical Activity and CHD Risk: In general, findings have been consistent in showing an inverse relationship between physical activity and CHD risk.
Sedentary Behavior and CHD Risk
Sedentary behavior may be an independent risk factor for CHD, --separate from physical activity.
In other words, you may exercise (even vigorously) but if you spend a lot of the rest of the day sitting, being inactive—you still carry the risk for getting CHD! You might exercise 2hrs a day but that still leaves 22 to be sedentary!
Even among people active enough to meet exercise guidelines those spending more time sitting were at increased risk of CVD mortality compared with those sitting less.
Physical inactivity contributes substantially ti the public health burden. Eliminating inactivity would have an impact on reducing excess mortality as great as, or greater than, eliminating other major CHD risk factors.
Physical Fitness and CHD Risk
While physical fitness has a genetic basis—regular physical activity also contributes to higher levels of physical fitness.
Low physical fitness is associated with increased risk of CVD & CHD. Cardio-vascular is the heart and the veins and arteries it pumps blood to. Coronary heart disease is a problem with the veins and arteries that distribute blood to the heart itself to keep it working properly.
The true size of the protective effect of physical activity against CHD is probably underestimated by the current methods used to measure physical activity, which undoubtedly misclassify some inactive people as active and some active people as inactive.
Although cardiorespiratory fitness is partly explainable by genetics, a high proportion of the variation in cardio fitness is explained by physical activity habits. The agreement of studies is that: Either physical activity or physical fitness supports the hypothesis of a causal relationship between regular physical activity and reduced risk of CHD.