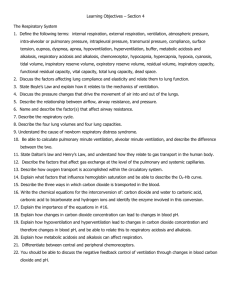
Respiratory Physiology

Ventilation-Perfusion Mismatch
Optimum gas exchange:
Ventilation and perfusion must match each other in all lung regions.
Mean ratio of approximately 1 somewhere in the middle of the lung
Range of ratios from 0.5 in the bottom of the lung to 5.0 in nondependent way of showing the matching : multicompartmental analysis by a multiple inert gas elimination technique : (MIGET)
PAO2 - PaO2 ~ 3 to 5 mm Hg (0.4 to 0.7 kPa)
More V/Q mismatch, the PAO2 - PaO2 difference is further increased
Impaired Diffusion
Reduces PaO2 can occur if the alveolar-capillary membranes are thickened: fibrosis systemic vascular diseases
Right-to-Left Shunt
2% to 3% of cardiac output in normal
In pathologic states, between nearly normal to above
50% of cardiac output
Shunt increases to 25%, the rise in PaO2 will be small by giving O2
With a shunt of 30% or greater, almost no effect of added
O2 can be seen
Respiratory Function During Anesthesia
Anesthesia causes an impairment in pulmonary function either:
Breathing spontaneously or
Ventilated mechanically
FIO2 is maintained at around 0.3 to 0.4.
Despite these measures : Mild to moderate hypoxemia:
O2 Sat 85% to 90% ~half of all patients undergoing elective surgery . Last few seconds to up to 30minutes.
In about 20% of patients O2 Sat below 81% for up to 5 minutes postoperative clinically significant pulmonary complications :
1% to 2% after minor surgery up to 20% after upper abdominal and thoracic surgery
Lung Volume and Respiratory Mechanics During Anesthesia
Lung Volume
FRC, is reduced by 0.8 to 1.0 L from upright to supine
0.4- to 0.5-L decrease when anesthesia has been induced
So,End-expiratory lung volume is reduced from approximately 1.5 to 2 L
Muscle paralysis and mechanical ventilation cause no further decrease in FRC.
Compliance and Resistance of the
Respiratory System
Static compliance(total) is reduced :
From 95 to60 mL/cm H2O during anesthesia.
Static lung compliance :
From a mean of 187 mL/cm H2O awake to 149 mL/cm
H2O during anesthesia
The possibility increased lung resistance :merely reflects reduced FRC during anesthesia
Atelectasis and Airway Closure During Anesthesia
Atelectasis :
Atelectasis could not be shown on conventional chest radiography
On CT with transverse exposure of the chest:
Development of densities in the dependent regions shown during anesthesia
Atelectasis appears in approximately 90% of all patients who are anesthetized.
15% to 20% of the lung is regularly collapsed at the base of the lung during uneventful anesthesia
After thoracic surgery and cardiopulmonary bypass:
More than 50% of the lung can be collapsed even several hours after surgery.
There is good correlation between the amount of atelectasis and pulmonary shunt as measured by MIGET.
A regression equation based on 45 patients studied during anesthesia with inhaled anesthetics :
Shunt = 0.8 × atelectasis + 1.7 ( r = .81, P < .01)
Prevention of Atelectasis During Anesthesia
POSITIVE END-EXPIRATORY PRESSURE:
Application of 10–cm H2O PEEP will consistently reopen collapsed lung tissue.
Prevention of Atelectasis During Anesthesia
MAINTENANCE OF MUSCLE TONE.
RECRUITMENT MANEUVERS:
Prevention of Atelectasis During Anesthesia
MINIMIZING GAS RESORPTION:
Ventilation with pure oxygen after a VC maneuver that reopened collapsed lung:
Resulted in rapid reappearance of the atelectasis.
But 40% O2 in nitrogen is used atelectasis reappears slowly
Prevention of Atelectasis During Anesthesia
POSTANESTHETIC OXYGENATION:
Not only preoxygenation promotes formation of atelectasis but:
Also the so-called postanesthetic oxygenation at the end of the surgery.
This procedure is often combined with suctioning of the airway tree.
A VC maneuver followed by a lower O2 concentration, 40%, kept the lung open after
Recruitment until the end of anesthesia.
Airway Closure
As much as 74% of the impaired arterial oxygenation can be explained by atelectasis and airway closure taken together, according to the following equation.
Distribution of Ventilation and Blood Flow During Anesthesia
Distribution of Ventilation:
Redistribution of inspired gas away from dependent to nondependent has been observed in anesthetized supine humans by isotope techniques.
PEEP increases dependent lung ventilation in anesthetized subjects in lateral position
Restoration of FRC toward awake level returns gas distribution toward awake pattern.
Distribution of Lung Blood Flow:
The lowermost portion of the lung, which was atelectatic as evidenced by simultaneous CT, was still perfused.
PEEP : reduce QT,
Affect PVR
Redistribution of blood flow toward dependent lung regions.
Hypoxic Pulmonary Vasoconstriction
Several inhaled anesthetics have been found to inhibit HPV in isolated lung
No such effect has been seen with intravenous anesthetics (barbiturates).
The HPV response may obscured by changes in :
Cardiac output, Myocardial contractility
Vascular tone Blood volume distribution
Blood pH Lung mechanics.
With no gross changes in cardiac output, isoflurane and halothane depress the HPV by 50% at a 2 MAC
Ventilation-Perfusion Matching During Anesthesia
Dead Space, Shunt, and Ventilation-Perfusion
Relationships
Both CO2 elimination and oxygenation of blood are impaired :
Increased dead space ventilation? Or
High V/Q ratios?
Impairment in arterial oxygenation is more severe in:
Higher ages
Obesity
Smokers
Venous admixture increased during anesthesia to approximately 10% of
QT.
Factors That Influence Respiratory Function During Anesthesia
Spontaneous Breathin
1- FRC is reduced
2- Atelectasis
(1&2) Same extent in spontaneously breathing as during muscle paralysis.
3- Cranial shift of the diaphrag lower, dependent portion of the diaphragm moved the most, whereas with muscle paralysis, the upper, nondependent part showed the largest displacement.
4-V/Q mismatch, increased from 0.66 to 0.83 and 0.89 from awake to spontaneous breathing and mechanical ventilation.
5-Shunt increased from 1% awake to 11% and 14% with spontaneous breathing and mechanical ventilation.
Increased Oxygen Fraction
Air (FIO2 of 0.21):
Only small shunts of 1% to 2%,
SDQ increased from 0.77 to 1.13.
FIO2 0.5 :
Increase in shunt of 3% to 4%
FIO2 0.53 to 0.85:
Shunt from 7% to 10%
Thus, a certain dependence on FIO2 exist:
1-Attenuation of the HPV OR
2- further development of atelectasis and shunt in lung units with low V/Q ratios
Body Position
FRC is dramatically reduced by the combined effect of supine position and anesthesia
Upright position preserve FRC. But!
No clear improvement in oxygenation was noticed
Increase V/Q mismatch
In anesthetized, paralyzed , lateral
and improvement in prone
Ventilation distribution is more uniform in anesthetized subjects in
prone position.
Age
Arterial oxygenation is further impeded with increa
1- Larger percentage of atelect
2- Increasing V/Q mismatch
1- Reduced FRC
2- Promotes airway closure
Obesity
Obesity worsens the oxygenation of blood
3- High FIO2 will promote rapid atelectasis
Correlations between BMI and:
1- Size of atelectasis during anesthesia and postoperatvely
2- Pulmonary shunt
Have been presented
Prevention:
PEEP or CPAP or FIO2=1 during induction & maintenance ?
Preexisting Lung Disease
Smokers and patients with lung disease have impairment of gas exchange:
In the awake state
Also during anesthesia
:
Considerable V/Q mismatch + large perfusion fraction to LOW V/Q regions
Interestingly, smokers with moderate airflow limitation!!
May have less shunt as measured by MIGET than healthy subjects
A possible reason( for absence of atelectasis and shunt )
May be chronic hyperinflation.
Regional Anesthesia
Type and extension of motor blockade:
Extensive blocks include all of the thoracic and lumbar segments:
1- Inspiratory capacity is reduced by 20%
2- Expiratory reserve volume approaches zero
Skillfully handled regional anesthesia affects pulmonary gas
exchange only minimally.
SaO2 and CO2 elimination well maintained during spinal and epidural anesthesia?
1-unchanged relationship of CC and FRC[116]
2-unaltered distributions of ventilation-perfusion ratios (MIGET,epidural anesthesia)
Lung Function After Cardiac Surgery
Cardiac surgery produces the largest atelectasis in the postoperative period
1-Both lungs collapsed
2-Patient connected to an extracorporeal pump and oxygenator
3-more than half the lung may be collapsed 1 to 2 days later
4-with a shunt that is around 20% to 30% of cardiac output
A recruitment maneuver with airway pressure of 30 cm H2O for a 20 second is sufficient to reopen the collapsed lung
Dyhr and coworkers studied 30 patients after cardiac:
1- lung recruitment maneuver (LRM = four 10-second ,AWP 45 cm H2O)then ZEEP
2- 12–cm H2O PEEP
3- LRM plus PEEP
Recruitment maneuver resulted in true opening of collapsed lung
PEEP alone caused hyperinflation of already open alveoli
Respiratory Function During One-Lung Ventilation
Oxygenation may be a challenge even during anesthesia.
One lung is nonventilated but still perfused,
Postoperative period: restoration of lung integrity & V/Q matching may take time
Measures in one lung ventilation
Tusman and colleagues tested an “alveolar recruitment strategy” (ARS):
1-Increasing PAP min by min from 25 to 30, 35, finally 40 cm H2O
2- Simultaneously increasing PEEP from 5 to 10, 15, finally 20 cm H2O
3-PAP then reduced of 25 and PEEP to 5 cm H2O
This resulted :increase in PaO2 from 217 to 470 mm Hg after ARS:
More of the shunt is located in the dependent lung than is generally considered.
In another (Tusman ) study,ARS :
Improved oxygenation
Dead space decreased
Slope of the CO2 curve during expiratory VT (phase III) was flatter
Measures in one lung ventilation(cont)
PEEP versus ZEEP
Thoracic epidural anesthesia
Inhaled nitric oxide (NO) alone or in combination with intravenous almitrine
Positioning of the patient
Pneumoperitoneum(CO2)
1-Hypercapnia and acidosis
2-Decreased cardiaccontractility
3-Sensitization of the myocardium to the arrhythmogenic effects of catecholamines
4-Systemic vasodilation
5-Even long-lasting postoperative effects on breathing control
6-Decreased FRC and VC 7-Formation of atelectasis
8-Reduced respiratory compliance 9-Increased peak airway pressure
Nonetheless, shunt is reduced and Sao2 is mostly improved ?
Paradox: more atelectasis and less shunt !!
CO2 may enhance HPV,may be the mechanism of the paradox
Physiotherapy
Physiotherapy may do more harm than good
As large an inspiration as possible and
As early in the postoperative period as possible are :
Two important factors in preventing postoperative lung complications.
Deep inspiration is done with or without a device for forced breathing
Normal Sleep
Ventilation is affected by sleep
Significant reduction in VT and inspiratory drive
Minute ventilation falls by 5% to 16% most marked during
REM .
Decrease FRC (REM)
Breathing pure oxygen would also lead to the formation of atelectasis.
CO
2
Transport
Carbon dioxide transport:
– ~9% dissolved in plasma
– ~13% as carbamino compounds
Most combined with Hb
– ~78% converted to HC0
3
-
CO
2
+ H
2
O H
2
CO
3
H + + HCO
3
-
Haldane effect
– Inverse relationship between amount of Hb-O
2 capacity of blood and CO
2 carrying
Hb binds and transports more CO
2 than O
2
Hb buffers more H + than Hb-O
2
– Promotes conversion of CO
2 to HCO
3
via carbonic anhydrase reaction
Key Concepts
O
2 mostly transported in blood bound to hemoglobin
If the P
O2
If P
O2 increases Hb binds O decreases Hb releases O
2
2
CO
2 mostly transported in blood as HCO
3
-
Lesser amounts of CO dissolved in plasma
2 are bound to Hb or
Respiratory centers (p. 848)
Basic rhythm of ventilation controlled by medullary rhythmicity area (medulla oblongata)
Inspiratory area (Dorsal Resp.Group)
– determines basic rhythm of breathing
– causes contraction of diaphragm and external intercostals
Expiratory area (Ventral Resp. Group)
– Inactive during normal quiet breathing
– Activated by inspiratory area during forceful breathing
– Causes contraction of internal intercostals and abdominal muscles
Respiratory centers
Transition between inhalation and exhalation controlled by:
– Pneumotaxic area
located in pons
inhibits inspiratory area of medulla to stop inhalation
– Breathing more rapid when pneumotaxic area active
– Apneustic area
located in pons
stimulates inspiratory area of medulla to prolong inhalation
Regulation of Respiratory centers
Basic rhythm of ventilation coordinated by inspiratory area of respiratory centre, but modified by:
– Cortical influences
Voluntary control over breathing
– Hypothalamus and limbic system
Emotional stimuli
– Proprioceptors
Upper motor neurons of primary motor cortex also stimulate inspiratory area
– Inflation (Hering-Breuer) reflex
Stretch receptors in walls of bronchi and bronchioles
– Inhibit inspiratory and apneustic areas
causes exhalation to begin to protect against overinflation
– Chemoreceptors
Increased PCO
2
, or reduced pH or PO inspiratory area of respiratory centre
2 causes chemoreceptors to stimulate
Problem solving
Josh hyperventilates for several minutes before diving into a pool. Shortly after he enters the water he blacks out and almost drowns. What caused this to happen?
Regulation of Respiratory centers
Rhythm of ventilation also modified by:
– Temperature
temp = ventilation (and vice versa)
sudden cold stimulus may cause apnea
– Pain
Sudden severe pain can cause apnea
Prolonged somatic pain increases respiratory rate
Visceral pain may slow respiratory rate
– Irritation of airways
– Blood pressure
BP = ventilation (and vice versa)
– Attempt to reduce venous return via respiratory pump?
Effects of smoking
Smoking reduces respiratory efficiency
– Deposits tar & other chemicals
– swelling of mucosal lining and increased production of mucus
Impedes airflow
– destroys cilia and inhibits their movement
Reduces removal of excess mucus and debris
Smokers lungs
Bodies The exhibition March 2006
Smoking
– Nicotine constricts terminal bronchioles
Reduces airflow into and out of lung
– CO binds irreversibly to Hb
Reduces blood oxygen carrying capacity
– Destruction of elastic fibers (prime cause of emphysema)
Reduced lung compliance
Collapse of small bronchioles during exhalation
– traps air in alveoli during exhalation
Reduces efficiency of gas exchange