Neuron Structure and Function
advertisement

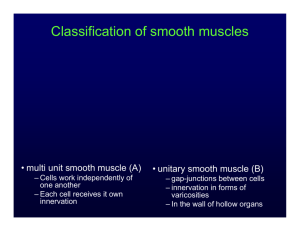
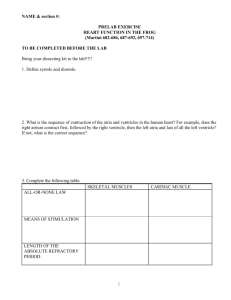
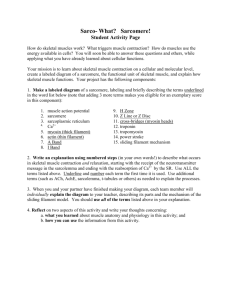
Muscles – general information Vertebrates and many invertebrates have three main classes of muscle • Skeletal muscle • Smooth muscles surround internal organs such as the large and small intestines, the uterus, and large blood vessels • Cardiac muscle: Striated muscle of the heart. Smooth Muscle - introduction • • • • Slow, regular contractions Prolonged contractions Contribute to many systems Key differences from skeletal muscle • Lack sarcomeres (no striations) • No t-tubules • Minimal SR • Gap junctions • Contract in all dimensions • More complex regulation Smooth muscles - introduction • • • • • • Smooth muscle cells have multiple receptors and activation mechanisms Smooth muscle cells can be activated by neurotransmitters, hormones, neighbouring cells Example: Electrical coupling through gap junctions synchronizes the contractions of the smooth muscle cells responsible for the peristaltic movements of the intestine Important: The overall goal is always the same.... change levels of cytosolic Ca2+ to change the degree of contraction. Another example: In a blood vessel there are spontaneously active pacemaker cells which can be conducted across a few or many cells. Some smooth muscle cells have fast contractions while other are slower or maintain muscle tone or sustained contractions for long periods of time Smooth muscles – more introduction • • • • • • • • • The sarcoplasmic reticulum network is sparse Majority of the increase in cytosolic Ca2+ needed for muscle contraction enters the cell via the plasma-membrane Ca2+ channel This means that changes in the cytosolic Ca2+ level occur much more slowly in smooth muscle (seconds to minutes). This has the advantage of allowing the slow, steady response in contractile tension that is required by vertebrate smooth muscle. Contraction in some smooth muscle cells are controlled by changes in membrane potential and some are purely through chemical/hormone processes Nerve innervation of smooth muscle cells is from the autonomic nervous system and similar to cardiac muscle cells works over a wide area of general neurotransmitter release The function of neurotransmitters is usually to modulate contraction rather than initiate contraction Many smooth muscle cells have the ability to spontaneously activate Contractions can occur over minutes rather than milliseconds as was seen with skeletal and hundreds of milliseconds as was seen with cardiac cells. Smooth muscles – more introduction • • • • • • A smooth muscle is composed of elongated spindle-shaped cells, each with a single nucleus Packed with thick and thin filaments but these filaments are not organized into well-ordered sarcomeres and thus smooth muscle is not striated Filaments in smooth muscle are gathered into loose bundles, which are attached to dense bodies in the cytosol Dense bodies apparently serve the same function as Z disks in skeletal muscle The other end of the thin filaments in many smooth muscle cells is connected to attachment plaques, which are similar to dense bodies but are located at the plasma membrane of a muscle cell Like a Z disk, an attachment plaque is rich in the actin-binding protein alpha-actinin; it also contains a second protein, vinculin, which binds to an integral membrane protein in the plaque and to alpha-actinin, thereby attaching actin filaments to membrane adhesion sites. Smooth muscles Smooth muscle contraction • • • • • Smooth muscle contraction is not controlled by the binding of Ca2+ to the troponin complex as it is in cardiac and skeletal muscles Ca2+ control of myosin attachment to the actin is through an intermediate step of Ca2+/calmodulin and it is this that controls contraction in smooth muscle cells Calmodulin = intracellular second messenger that binds Ca2+ Troponin is not found in smooth muscle cells (tropomyosin is) Caldesmon = regulatory protein on smooth muscle actin. Binds to actin and prevents myosin from binding actin Caldesmon and Ca2+/calmodulin • • • • The activation of smooth muscle myosin can be regulated by caldesmon (CD) which in low Ca2+ levels (10-6 M), binds to tropomyosin and actin and blocks myosin binding to actin As Ca2+ levels increase, Ca2+ activated calmodulin binds to caldesmon which releases caldesmon from the tropomyosin/actin complex Now myosin is free to bind and move along the thin filaments to contract the cell Phosphorylation by several kinases, including MAP kinase, and dephosphorylation by phosphatases also regulate caldesmon’s actinbinding activity * * * Myosin light chain kinase (MLCK) and Ca2+/calmodulin • • • In vertebrate smooth muscle, phosphorylation of the myosin regulatory light chains on site X by Ca2+-dependent myosin LC kinase activates contraction At Ca2+ concentrations < 10-6 M, the myosin LC kinase is inactive A myosin LC phosphatase, which is not dependent on Ca2+ for activity, dephosphorylates the myosin LC, causing muscle relaxation Myosin light chain kinase and Ca2+/calmodulin Two enzymes control this process: • Myosin light chain kinase (MLCK) and myosin light chain phosphotase • One of the two myosin light chain pairs associated with the myosin in smooth muscle inhibits actin stimulation of the myosin ATPase activity at low Ca2+ concentrations • Phosphorylation of the myosin light chain by MLCK removes this inhibition and the smooth muscle contracts • MLCK is activated by Ca2+ through calmodulin • Ca2+ binds to calmodulin, and the Ca2+-calmodulin complex then binds to MLCK and activates it • Because this mode of regulation relies on the diffusion of Ca2+ and the action of protein kinases, muscle contraction is much slower in smooth muscle than in skeletal muscle. • The greater the amount of intracellular Ca2+ the more MLCK is activated and the greater the degree of contraction Contraction – simple • * * • • • * * * * • Intracellular Ca2+ increase and Ca2+ is released from the SR Ca2+ binds to calmodulin (CaM) Ca2+ - calmodulin complex activates MLCK MLCK phosphorylates light chains in myosin heads and increases myosin ATPase activity Active myosin crossbridges slide along actin and create muscle Relaxation - simple • * * • • * • * Free Ca2+ in cytosol decreases when Ca2+ is pumped out of the cell or back into the SR released from the SR Ca2+ unbinds from calmodulin Myosin phosphatase removes phosphate from myosin, which decreases myosin ATPase Less myosin ATPase activity results in decreased muscle tension Regulation of smooth muscle contraction • • • • The major means that control smooth muscle contraction is controlled is through changes in resting membrane potential Depolarization causes a greater increase in cytosolic Ca2+ and thus greater contraction Hyperpolarization causes a reduced amount of cytosolic Ca2+ and thus relaxes the muscle cell However it is important to note that release of Ca2+ from internal stores may also lead to greater contraction through G protein mediated cascades that have nothing to do with changes in membrane depolarization. Norepinephrine and epinephrine • • • • Depending on the type of receptor norepinephrine and epinephrine can have different results on the smooth muscle cell Epinephrine bound to beta-adrenergic receptors on smooth muscle cells of the intestine causes them to relax Epinephrine also binds to the alpha2-adrenergic receptor found on smooth muscle cells lining the blood vessels in the intestinal tract, skin, and kidneys Epinephrine bound to alpha2 receptors causes the arteries to contract (constrict), reducing circulation to these organs Acetylcholine and Nitric Oxide • • • • • • ACH is released by autonomic nerves in the walls of a blood vessel, and it causes smooth muscle cells in the vessel wall to relax ACH acts indirectly by inducing the nearby endothelial cells to make and release NO, which then signals the underlying smooth muscle cells to relax. Regulation of contractility of arterial smooth muscle by NO and cGMP: NO synthesized in endothelial cells diffuses locally through tissue and activates guanylate cyclase in nearby smooth muscle cells The resulting rise in cGMP leads to the relaxation of the muscle and vasodilation. Cont….. Acetylcholine and Nitric Oxide • • Schematic diagram of the structure of soluble guanylate cyclase Binding of NO to the heme group stimulates the enzyme’s catalytic activity, leading to formation of cGMP from GTP. More about Nitric Oxide • • • • • • • • NO gas is catalyzed by the enzyme NO synthase from arginine It passes readily across membranes and rapidly diffuses out of the cell into neighboring cells NO has a very short half life (5-10 seconds) - so acts only locally In many target cells, NO binds to iron in the active site of the enzyme guanylyl cyclase, stimulating this enzyme to produce cyclic GMP. The effects of NO can occur within seconds, because the normal rate of turnover of cyclic GMP is high Increased cGMP activates a kinase that subsequently leads to the inhibition of calcium influx into the smooth muscle cell, and decreased calcium-calmodulin stimulation of myosin light chain kinase (MLCK). This in turn decreases the phosphorylation of myosin light chains, thereby decreasing smooth muscle tension development and causing vasodilation. Other evidence suggests that cGMP works through a kinase (cGMP dependent protein kinase PKG) that in turn phosphorylates a K+ channel to activate and thus hyperpolarize the muscle cell Other regulators Nitroglycerine • Has been used for about 100 years to treat patients with angina (pain resulting from inadequate blood flow to the heart muscle) • Nitroglycerine is converted to NO, which relaxes blood vessels • This reduces the workload on the heart and reduces the oxygen levels needed by the heart muscle. Viagra • The drug sildenafil [Viagra] inhibits this cyclic GMP phosphodiesterase and increases the amount of time that cyclic GMP levels remain elevated. • The cyclic GMP keeps blood vessels relaxed and in certain parts of the male anatomy blood pools and the resulting effect has sales of Viagra soaring. It is interesting to note however that Viagra is not specific to the penis it will affect cGMP levels throughout the body and can have some interesting side effects. More about ACH Tissue Vasculature (endothelial cells) Eye iris (pupillae sphincter muscle) Ciliary muscle Salivary glands and lacrimal glands Bronchi Heart Gastrointestinal tract Urinary bladder Sweat glands Reproductive tract, male Uterus Effects of ACh Release of endothelium-derived relaxing factor (nitric oxide) and vasodilation Contraction and miosis Contraction and accommodation of lens to near vision Secretion—thin and watery Constriction, increased secretions Bradycardia, decreased conduction (atrioventricular block at high doses), small negative inotropic action Increased tone, increased gastrointestinal secretions, relaxation at sphincters Contraction of detrusor muscle, relaxation of the sphincter Diaphoresis Erection Variable, dependent on hormone influence Smooth muscles End of smooth muscle Cardiac muscle – general info Many similar properties to skeletal muscles but there are some important differences Hearts of course vary greatly in size, shape and complexity from animal to animal - ranging from insects with a simple tube that pumps blood or hemolymph around an open circulatory system to our closed circulatory system and a four chambered heart Cardiac muscle Cardiac muscle – general info 1) The heart contains pace-maker cells that produce the depolarization and action potentials to drive cardiac cell contraction Heart contraction is not neuronally driven but self-driven or myogenically. Some vertebrates hearts are innervated by neurons from the sympathetic and parasympathetic nervous systems but these neurons act in a modulatory function only 2) Each muscle cell is a single cell not multinucleate like skeletal muscle Like skeletal muscle cells each cell contains multiple myofibrils and in the cases of higher vertebrates an extensive sarcoplasmic reticulum Depending on the size of the cardiac muscle cells contraction can depend on Ca2+ release from the SR and/or Ca2+ influx from external sources outside the cell 3) Cardiac muscle cells are linked to each other with gap junctions Allows an action potentials to rapidly travel from cell to cell and makes the heart work as a unit. Allows the pacemaker cells, the sinoatrial node cells, to generate the action potential which is in turn relayed via the gap junctions throughout the heart to generate contraction through out the heart. Cardiac muscle – general info cont. 4) There are different types of cardiac muscle cells ranging from the pacemaker cells in the sinoatrial node to the atrial and ventricular cells that produce the contraction of the heart chambers 5) The action potential in cardiac cells is quite different from skeletal muscle and neuronal action potentials in that voltage-gated Ca2+ channels play a much larger role 6) The mechanism of triggering the Ca2+ release channel in the sarcoplasmic reticulum is not the same as in vertebrate skeletal muscle cells Pacemaker Cells Derived from cardiac muscle cells Differences from most cardiac muscle Small with few myofibrils, mitochondria or other organelles Do not contract Have unstable resting membrane potential (pacemaker potential) that slowly drifts upwards until it reaches a threshold and activates and action potential Cardiac muscle channels and action potentials Pumps and transporters 1) Na+/K+ ATPase pump - to establish the electrochemical gradients of Na+ and K+ 2) Ca2+ ATPase pump - uses energy from ATP to remove 2 Ca2+ from the inside to the outside of the cell or into the sarcoplasmic reticulum to ensure that internal Ca2+ concentrations remain low (10-7 mM internal) Some cardiac cells (i.e. lower vertebrates, invertebrates) do not have an extensive sarcoplasmic reticulum and thus most of the Ca2+ that is used to trigger contraction is from extracellular sources 3) Na+/Ca2+ cotransporter - to also remove Ca2+ from the inside of the cell and uses the energy from the cotransport of 3 Na+ molecules to export 1 Ca2+. Excitation-contraction coupling Cardiac muscle channels and action potentials Channels 1) leak channels - leak K+channel 2) voltage-gated Na+ channels There is a skeletal muscle voltage-gated Na+ channel which properties very much like the neuronal voltage-gated Na+ channel Responsible for the production of the action potential 3) voltage-gated K+ channel - the delayed rectifier K+ channel 4) voltage gated Ca2+ channels In cardiac cells the Ca2+ channel plays a much greater role during the action potential These channels are the high threshold Ca2+ channels, called L channel or DHP (dihydropyridine channel) The cardiac DHP channel is very similar to the skeletal muscle DHP Ca2+ channel and are found concentrated in the T-tubules in those cardiac cells with extensive T-tubules and SR. Action potential in ventricular (and atrial) cardiac cells 4) Resting potentials in these cells is set by a large K+ permeability due to a combination of the leak K+ channel and a voltage-gated K+ channel (called the inward rectifier K+ channel) that is open at rest This means that rest is very close to EK+ 0) The rising phase of the action potential is set by the cardiac voltagegated Na+ channel Action potential in ventricular (and atrial) cardiac cells 1-2) As the voltage-gated Na+ channels produce the rising phase and then start to inactivate two channels will now be opening, the delayed rectifier K+ channel and the voltage-gated Ca2+ channel (L or DHP channel) There are many Ca2+ channels in these cells and thus this channel dominates the membrane potential producing a long plateau of depolarization This plateau is a balance between the open Ca2+ channels and the open K+ channels Ca2+ channel only slowly inactivates and thus this plateau can persist for 100-200 msec. Action potential in ventricular (and atrial) cardiac cells 3) Finally the voltage-gated Ca2+ channel inactivates and the voltagegated K+ channels will now dominate and the membrane potential will repolarize to rest (EK+ in these cells). Then the voltage-gated K+ channels will close, the voltage-gated Na+ channels will switch from the inactive to the closed state and the membrane is set back at 4) ready to fire again. The long Ca2+ plateau allows Ca2+ inside the cell to elevate enough to generate contraction in the case of those cardiac cells that rely on external Ca2+ sources. Action potential in sinoatrial cardiac cells Sinoatrical cells have the ability to spontaneously fire action potentials in a repeated fashion without any external influence. These cells are the pacemaker cells of the heart and once an action potential fires in these cells it is propagated via gap junctions to other regions of the heart first to the atrial cells and then eventually making it to the ventricular cells. Action potential in sinoatrial cardiac cells The generation of the action potential in these cells is very similar to the ventricular cardiac cells with a few major exceptions 1) These cells do not have a stable rest. There is a spontaneous slow depolarization that brings the membrane from -60 mV to threshold for the action potential (about -40 mV) 2) The action potential is driven by the voltage-gated Ca2+ channel in most SA cells 3) The rising phase is due the opening of the voltage-gated Ca2+ channel (L or DHP channel again) and thus is slower than in other excitable cells As the Ca2+ channel inactivates the membrane is repolarized by the delayed rectifier K+channel as in other excitable cells 4) What makes these cells then spontaneously depolarize once the delayed K+ channel has closed is the presence of an ion channel that is activated by hyperpolarization. A channel that opens when the membrane becomes repolarized and allows Na+ to flow into the cell Called the funny channel in some literature Na+ influx will depolarize the membrane to open the voltage-gated Ca2+ channels and at the same time close the funny channel. The funny channel This unusual cation channel is activated by hyperpolarization As the membrane repolarizes after the action potential the threshold for opening of the funny channel is reached at about -50 mV The channel opens and allows Na+ to preferentially flow into the cell The funny channel is also called the HCN channel or hyperpolarization, cyclic nucleotide gated ion channel cAMP can have dramatic influences on this channel and shift its threshold of activation from -50 mV to -40 mV. The funny channel actually looks very much like a voltage-gated K+ channel but has differences in its pore to allow Na+ influx and in the voltage sensing/opening mechanism. Putting it all together…… Located in the right atrium at the superior vena cava is the sinus node (sinoatrial or SA node) which consists of specialized muscle cells The SA nodal cells are self-excitatory, pacemaker cells They generate an action potential at the rate of about 70 per minute in humans (your heart beat) From the sinus node, activation propagates throughout the atria, but cannot propagate directly across the boundary between atria and ventricles This boundary serves to ensure a delay between the activation of the atria and the ventricles The atrioventricular node (AV node) is located at the boundary between the atria and ventricles In a normal heart, the AV node provides the only conducting path from the atria to the ventricles Putting it all together…… Propagation from the AV node to the ventricles is provided by a specialized muscle cells called the bundle of His conduct the signal system Further down the bundle separates into two bundle branches which travel along each side of the septum, constituting the right and left bundle branches. Even more distally the bundles split into Purkinje fibers that branch and contact the inner sides of the ventricular walls. From the inner side of the ventricular wall, these activation sites cause the formation of a wave of depolarization which propagates through gap junctions between the ventricular cells toward the outer wall After each ventricular muscle region has depolarized, repolarization occurs. Electrocardiogram - ECG The different potential generated in the heart can be measured using an electrocardiogram. An ECG is a recording of the electric potentials being generated during heart activity The potentials ("waves") are registered by electrodes placed on certain parts of the body and measure changes in potential (mV) P wave - an impulse is generated at the sinoatrial node and spreads across both atria, causing them to contract Delay: The Fibro-fatty atrioventricular groove insulates the ventricles from the atrial impulse The AV node is the only normal gateway of conduction to the ventricles QRS wave - The impulse travels down the AV bundle and it's branches and reaches the Purkinje fibers The ventricles are stimulated to contract T wave - correlates with repolarization of the ventricles. Electrocardiogram - ECG Electrocardiogram - ECG Increasing the heart rate Epinephrine and norepinephrine Released from the sympathetic nervous system Epinephrine and norepinephrine are synthesized and released into the blood by the adrenal medulla, an endocrine organ Epinephrine and the related norepinephrine are all synthesized from tyrosine and contain the catechol moiety; hence they are referred to as catecholamines Nerves that synthesize and use epinephrine or norepinephrine are termed adrenergic Adrenergic receptors: bind epinephrine and norepinephrine. Because different receptors are linked to different G proteins, the activation leads to different signal transduction cascades More Na+ and Ca2+ channels open Rate of depolarization and action potentials increase Increasing the heart rate cont. Epinephrine and norepinephrine cont…. In sinoatrial cells: norepinephrine binds to the b-adrenergic receptor which is a G protein associated membrane receptor This triggers a signal transduction cascade outlined below that activates the G protein (Gs - stimulates) that activates adenylate cyclase to produce cAMP. Beta-blockers: Drugs which are used to slow heart contractions in the treatment of cardiac arrhythmia and angina, are beta1-adrenergic receptor antagonists They bind the beta1-adrenergic receptor to block the receptor and thus slow heart contraction Cardiac muscle cells possess beta1 adenergic receptors Decreasing the heart rate Acetylcholine: released from parasympathetic nervous system Muscarinic acetylcholine receptor: a G protein associated receptor. The G protein activated in this case is a Gi subunit that inhibits adenylate cyclase More K+ channels open Pacemaker cells hyperpolarize Time for depolarization takes longer Modulating the funny channel Through G protein coupled receptors various hormones/neurotransmitters or drugs can increase or decrease the heart rate by simply increasing or decreasing the ability of the funny channel to open. Modulating the funny channel Activation of adenylyl cyclase following binding of an appropriate hormone (e.g., epinephrine, glucagon) to a Gs protein coupled receptor Following ligand binding to the receptor, the Gs protein relays the hormone signal to the effector protein, in this case adenylyl cyclase Gs cycles between an inactive form with bound GDP and an active form with bound GTP Dissociation of the active form yields the Gsalpha · GTP complex, which directly activates adenylyl cyclase Activation is short-lived because GTP is rapidly hydrolyzed The increase in cAMP physically binds to the funny channel and makes the channel open more easily In other words the threshold for opening shifts from around -50 mV to around -40 mV Therefore the funny channel will open sooner during the repolarization stage of the sinoatrial action potential and a second action potential will be triggered sooner This means that a second wave of action potential and thus contraction will travel through the heart sooner ie. a faster heart rate. Modulating the funny channel Modulation of Ca2+ channel Epinephrine also causes an increase in cAMP that stimulates PKA (protein kinase A) which in turn phosphorylates the voltage-gated Ca2+ channel (L channel) This phosphorylation results in a protein conformational change that enhances the channels activity This new conformation of Ca2+ channel opens more readily (i.e. less time between action potentials) and opens for longer (i.e. more Ca2+ flow into the cell = greater [Ca2+] intracellular = greater contraction). Epinephrine also stimulates glycogen breakdown in skeletal muscles During periods of concentrated activity the glycogen energy stores of muscles can be mobilized Caffeine (mmmmhhh): blocks the activty of phosphodiesterases. Phosphodiesterases break down cyclic nucleotides Therefore in the presence of caffeine cAMP levels remain elevated and thus the funny channel continues to open more readily Therefore the sinoatrial action potential fires more frequently and heart rate is increased. Also affects the Ca2+ release channel or ryanodine receptor such that more Ca2+ is released through the channel. Therefore heart contractions are stronger in the presence of caffeine as well Modulating the funny channel Acetylcholine works to block any rise in cAMP and reduces cAMP levels in the cell Therefore the funny channel will now not open so readily and the slow depolarziation of the membrane will occur later thus resulting in a longer time to generate a second action potential. Modulating the voltage-gated K+ channels Acetylcholine-induced opening of K+ channels in the heart muscle plasma membrane Binding of ACH by muscarinic ACH receptors triggers activation of a transducing G protein by catalyzing exchange of GTP for GDP on the alpha subunit The released beta/gamma subunit then binds to and opens a K+ channel The increase in K+ permeability hyperpolarizes the membrane, which reduces the frequency of heart muscle contraction Activation is terminated when the GTP bound alpha subunit is hydrolyzed to GDP and Galpha · GDP recombines with Gbeta/gamma. Modulating the voltage-gated K+ channels Application of acetylcholine (or muscarine) to frog heart muscle produces, after a lag period of about 40 ms (not visible in graph), a hyperpolarization of 2 3 mV, which lasts several seconds From receptor to control of muscle cell contraction From receptor to control of muscle cell contraction • • • • The cardiovascular system is highly regulated so that there is always an adequate supply of oxygenated blood to the body tissues under a wide range of circumstances There are receptors that respond to the degree of blood pressure and provide mechanical (barosensory) information about pressure in the arteries system There are receptors that provide information about the level of oxygen and carbon dioxide in the blood These sensory systems provide input to the respiratory control centers of the brain which in turn control the parasympathetic and sympathetic nerves that will control the heart, blood vessels and diaphragm muscles for breathing. From receptor to control of muscle cell contraction • • • • • • We will concentrate only on the chemoreceptors which are located primarily in the carotid bodies These are small, specialized organs located at the bifurcation of the common carotid arteries (some chemosensory tissue is also found in the aorta) The chemoreceptors in the carotid bodies and aorta provide information about the partial pressure of oxygen (pO2) and carbon dioxide (pCO2) in the blood This information is relayed by second order neurons to the hypothalamus and other regions in the brainstem This information about blood gas levels works in a reflex to modulate the autonomic nervous system to control smooth and cardiac muscles It is a balance between regulation of the sympathetic versus parasympathetic system to up or down regulate cardiac or smooth muscle contraction. From receptor to control of muscle cell contraction • • • • The carotid chemosensory cells detect levels of pO2 in the blood by simply depolarizing in response to decreased levels of oxygen The mechanism appears to be an O2 sensitive K+ channel, that in the presence of normal levels of pO2 is open Therefore the Vm is close to EK+ As oxygen levels drop the K+ channel closes and Vm depolarizes allowing the voltage-gated Ca2+ channel to open and to trigger vesicle fusion and neurotransmitter release From receptor to control of muscle cell contraction • • • • • • • • PO2 levels can have a direct effect on smooth muscles around blood vessels Many of these cells have K+ channel that is inhibited by ATP As PO2 drops so does respiration and ATP production This reduction in ATP results in the opening of K + channels and the inhibition of smooth muscle contraction This results in the relaxation of the smooth muscles the relaxation of the blood vessels and the increase blood flow into the tissue that is experiencing reduced PO2 Conversely an increase in PO2 results in greater inhibition of the ATP sensitive K + channels and thus a greater degree of depolarization More Ca 2+channels are open and thus there is greater cytosolic Ca2+ levels, greater degree of smooth muscle contraction This causes the blood vessel to constrict (vasoconstriction) and less PO2 transfer to the surrounding tissues. From receptor to control of muscle cell contraction