Chartpack - The Commonwealth Fund
advertisement
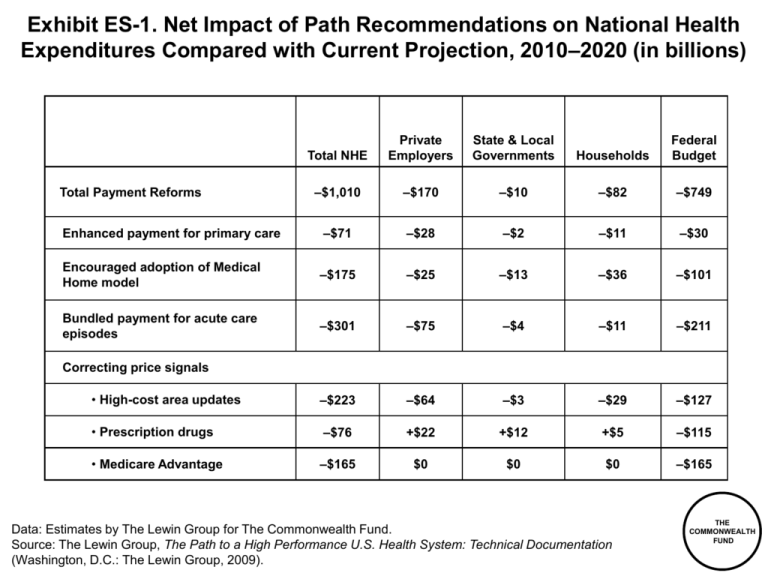
Exhibit ES-1. Net Impact of Path Recommendations on National Health Expenditures Compared with Current Projection, 2010–2020 (in billions) Total NHE Private Employers State & Local Governments Households Federal Budget –$1,010 –$170 –$10 –$82 –$749 Enhanced payment for primary care –$71 –$28 –$2 –$11 –$30 Encouraged adoption of Medical Home model –$175 –$25 –$13 –$36 –$101 Bundled payment for acute care episodes –$301 –$75 –$4 –$11 –$211 • High-cost area updates –$223 –$64 –$3 –$29 –$127 • Prescription drugs –$76 +$22 +$12 +$5 –$115 • Medicare Advantage –$165 $0 $0 $0 –$165 Total Payment Reforms Correcting price signals Data: Estimates by The Lewin Group for The Commonwealth Fund. Source: The Lewin Group, The Path to a High Performance U.S. Health System: Technical Documentation (Washington, D.C.: The Lewin Group, 2009). THE COMMONWEALTH FUND Exhibit ES-2. Total National Health Expenditure Growth for Hospitals and Physicians, Current Projections and with Policy Changes, 2009–2020 Hospital Expenditures (trillions) Physician Expenditures (trillions) $1.8 $1.8 Current Projection $1.6 Path Policy Current Projection Path Policy $1.6 $1.6 $1.4 $1.4 $1.4 $1.3 $1.2 $1.2 $1.0 $1.0 $1.1 $0.8 $0.8 $0.8 $0.6 $0.6 $0.4 $0.4 $0.2 $0.2 $0.0 $0.7 $0.0 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 Data: Estimates by The Lewin Group for The Commonwealth Fund. Source: The Lewin Group, The Path to a High Performance U.S. Health System: Technical Documentation (Washington, D.C.: The Lewin Group, 2009). THE COMMONWEALTH FUND Integrated system capitation Global DRG fee: hospital, post- acute, and physician inpatient Outcome measures; large % of total payment Less Feasible Care coordination and intermediate outcome measures; moderate % of total payment Global DRG fee: hospital only Global ambulatory care fees More Feasible Global primary care fees Preventive care; management of chronic conditions measures; small % of total payment Blended FFS and medical home fees Continuum of P4P Design Continuum of Payment Bundling Exhibit 1. Interrelation of Organization and Payment FFS and DRGs Small MD practice; unrelated hospitals Primary care MD group practice Multispecialty MD group practice Hospital system Integrated delivery system Source: A. Shih, K. Davis, S. Schoenbaum, A. Gauthier, R. Nuzum, and D. McCarthy, Organizing the U.S. Health Care Delivery System for High Performance (New York: The Commonwealth Fund, Aug. 2008). THE COMMONWEALTH FUND Exhibit 2. If Insurer Premium Trend Continues, Public Health Insurance Plan Enrollment Will Grow: Distribution of Coverage by Primary Source Under Current Law (2010) and Path Framework (Small Firms in 2010, All Firms in 2014) Path Framework, Small Firms (2010) Current Law (2010) Path Framework, All Firms (2014) Uninsured 4m 1% Uninsured 4m 1% Medicaid 49m 16% Medicare 41m 13% Private 170m 55% Uninsured 49m 16% Medicaid 42m 14% Medicaid 49m 16% Private 178m 58% Medicare 41m 13% Private 109m 35% Medicare 39m 13% Public Health Insurance Plan 43m 14% Public Health Insurance Plan 105m 34% THE Source: The Lewin Group, The Path to a High Performance U.S. Health System: Technical Documentation (Washington, D.C.: The Lewin Group, 2009). COMMONWEALTH FUND Exhibit 3. Adults with an Accessible Primary Care Provider Percent of adults ages 19–64 with an accessible primary care provider* U.S. Average 66 2002 65 2005 U.S. Variation 2005 69 White 59 Black 49 Hispanic 73 400% + of poverty 200–399% of poverty 63 53 <200% of poverty 74 Insured all year 51 Uninsured part year 37 Uninsured all year 0 20 40 60 * An accessible primary care provider is defined as a usual source of care who provides preventive care, care for new and ongoing health problems, and referrals, and who is easy to get to. Data: B. Mahato, Columbia University analysis of Medical Expenditure Panel Survey. Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2008. 80 100 THE COMMONWEALTH FUND Exhibit 4. Receipt of Recommended Screening and Preventive Care for Adults Percent of adults (ages 18+) who received all recommended screening and preventive care within a specific time frame given their age and sex* U.S. Average 49 2002 50 2005 U.S. Variation 2005 58 400% + of poverty 200–399% of poverty 47 39 <200% of poverty 53 Insured all year 46 Uninsured part year 32 Uninsured all year 0 20 40 60 * Recommended care includes seven key screening and preventive services: blood pressure, cholesterol, Pap, mammogram, fecal occult blood test or sigmoidoscopy/colonoscopy, and flu shot. Data: B. Mahato, Columbia University analysis of Medical Expenditure Panel Survey. Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2008. 80 100 THE COMMONWEALTH FUND Exhibit 5. Chronic Disease Under Control: Diabetes and Hypertension National Average By Insurance, 1999–2004 Percent Percent 1999–2000 100 2003–2004 Insured 100 Uninsured 88 80 81 79 80 63 60 60 41 41 40 40 31 21 20 20 0 0 Diabetes under control* High blood pressure under control** Diabetes under control* * Refers to diabetic adults whose HbA1c is <9.0. ** Refers to hypertensive adults whose blood pressure is <140/90 mmHg. Data: J. McWilliams, Harvard University analysis of National Health and Nutrition Examination Survey. Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2008. High blood pressure under control** THE COMMONWEALTH FUND Exhibit 6. Costs of Care for Medicare Beneficiaries with Multiple Chronic Conditions, by Hospital Referral Regions, 2001 and 2005 Ratio of percentile groups Average annual reimbursement Average 10th percentile 25th percentile 75th percentile 90th percentile 90th to 10th 75th to 25th 2001 2005 $31,792 $38,004 $20,960 $25,732 $23,973 $29,936 $37,879 $44,216 $43,973 $53,019 2.10 2.06 1.58 1.48 2001 2005 $18,461 $23,056 $12,747 $16,144 $14,355 $18,649 $20,592 $26,035 $27,310 $32,199 2.14 1.99 1.43 1.40 2001 2005 $13,188 $15,367 $8,872 $11,317 $10,304 $12,665 $15,246 $17,180 $18,024 $20,062 2.03 1.77 1.48 1.36 2001 2004 $22,415 $27,498 $15,355 $19,787 $17,312 $22,044 $25,023 $31,709 $32,732 $37,450 2.13 1.89 1.45 1.44 All 3 conditions (Diabetes + CHF + COPD) Diabetes + CHF Diabetes + COPD CHF + COPD CHF = Congestive heart failure; COPD = Chronic obstructive pulmonary disease. Data: G. Anderson and R. Herbert, Johns Hopkins University analysis of Medicare Standard Analytical Files (SAF) 5% Inpatient Data. Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2008. THE COMMONWEALTH FUND Exhibit 7. Medicare Reimbursement and 30-Day Readmissions by State THE COMMONWEALTH FUND Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2008. Exhibit 8. Medicare Hospital 30-Day Readmission Rates Percent of Medicare beneficiaries admitted for one of 31 select conditions who are readmitted within 30 days following discharge* 30 20 18 21 20 18 16 20 75th 90th 16 15 14 19 10 0 2003 2005 U.S. Mean 10th 25th 75th 90th Hospital Percentiles, 2005 10th 25th State Percentiles, 2005 * See report Appendix B for list of conditions used in the analysis. Data: G. Anderson and R. Herbert, Johns Hopkins University analysis of Medicare Standard Analytical Files (SAF) 5% Inpatient Data. Source: Commonwealth Fund National Scorecard on U.S. Health System Performance, 2008. THE COMMONWEALTH FUND Exhibit 9. Average Risk-Adjusted Standardized Spending for Hospital Readmissions and Post-Acute Care After Coronary Artery Bypass, 2001–2003 Bottom 25th Percentile Average Spending (Mean) Upper 75th Percentile $3,500 $2,911 $3,000 $2,822 $2,500 $1,887 $2,000 $1,651 $1,500 $1,000 $947 $800 $500 $0 Hospital Readmissions Post-Acute Care Source: G. Hackbarth, R. Reischauer, and A. Mutti, “Collective Accountability for Medical Care— Toward Bundled Medicare Payments,” New England Journal of Medicine, July 3, 2008 359(1):3–5. THE COMMONWEALTH FUND Exhibit 10. Net Impact of Path Recommendations on National Health Expenditures Compared with Current Projection, 2010–2020 (in billions) Total NHE Private Employers State & Local Governments Households Federal Budget –$1,010 –$170 –$10 –$82 –$749 Enhanced payment for primary care –$71 –$28 –$2 –$11 –$30 Encouraged adoption of Medical Home model –$175 –$25 –$13 –$36 –$101 Bundled payment for acute care episodes –$301 –$75 –$4 –$11 –$211 • High-cost area updates –$223 –$64 –$3 –$29 –$127 • Prescription drugs –$76 +$22 +$12 +$5 –$115 • Medicare Advantage –$165 $0 $0 $0 –$165 Total Payment Reforms Correcting price signals Data: Estimates by The Lewin Group for The Commonwealth Fund. Source: The Lewin Group, The Path to a High Performance U.S. Health System: Technical Documentation (Washington, D.C.: The Lewin Group, 2009). THE COMMONWEALTH FUND Exhibit 11. Total National Health Expenditures (NHE), 2009–2020 Current Projection and Alternative Scenarios NHE in trillions $6 Current projection 6.7% annual growth Reform proposals $5 $5.2 Constant (2009) proportion of GDP $4.6 $4.2 $4 5.5% annual growth $3 4.7% annual growth $2.6 $2 Cumulative reduction in NHE through 2020: $3 trillion $1 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 Note: GDP = Gross Domestic Product. Data: Estimates by The Lewin Group for The Commonwealth Fund. Source: The Commonwealth Fund Commission on a High Performance Health System, The Path to a High Performance U.S. Health System: A 2020 Vision and the Policies to Pave the Way (New York: The Commonwealth Fund, Feb. 2009). THE COMMONWEALTH FUND Exhibit 12. Total National Health Expenditure (NHE) Growth by Provider Group, Current Projections and with Policy Changes, 2009–2020 Total NHE All other Physician & other professional Hospital Projected Growth, Current Policy Revenue Growth with Path Policies Expenditure (trillions) Expenditure (trillions) $6.0 $6.0 $5.2 $5.0 $5.0 $2.3 $4.0 $4.6 $4.0 $2.1 $3.0 $2.0 $2.5 $1.0 $3.0 $1.3 $2.0 $0.7 $1.0 $1.6 $0.8 $0.0 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 $1.0 $2.5 $1.0 $1.1 $0.7 $1.4 $0.8 $0.0 2009 2010 2011 2012 2013 2014 Data: Estimates by The Lewin Group for The Commonwealth Fund. Source: The Commonwealth Fund Commission on a High Performance Health System, The Path to a High Performance U.S. Health System: A 2020 Vision and the Policies to Pave the Way (New York: The Commonwealth Fund, Feb. 2009). 2015 2016 2017 2018 2019 2020 THE COMMONWEALTH FUND Exhibit 13. Total National Health Expenditure Growth for Hospitals and Physicians, Current Projections and with Policy Changes, 2009–2020 Hospital Expenditures (trillions) Physician Expenditures (trillions) $1.8 $1.8 Current Projection $1.6 Path Policy Current Projection Path Policy $1.6 $1.6 $1.4 $1.4 $1.4 $1.3 $1.2 $1.2 $1.0 $1.0 $1.1 $0.8 $0.8 $0.8 $0.6 $0.6 $0.4 $0.4 $0.2 $0.2 $0.0 $0.7 $0.0 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 2009 2010 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 Data: Estimates by The Lewin Group for The Commonwealth Fund. Source: The Lewin Group, The Path to a High Performance U.S. Health System: Technical Documentation (Washington, D.C.: The Lewin Group, 2009). THE COMMONWEALTH FUND Exhibit 14. Provider Payments as a Percent of Medicare Payments for Similar Services 160% 141% 140% 123% 120% 94% 100% 80% 69% 60% 40% 20% 0% Private Insurance Medicaid Hospital Care Private Insurance Medicaid Physician Care Data: American Hospital Association, MedPAC, Kaiser Family Foundation. Source: The Lewin Group, The Path to a High Performance U.S. Health System: Technical Documentation (Washington, D.C.: The Lewin Group, 2009). THE COMMONWEALTH FUND Exhibit 15. Expenditures for Health Services by Type of Service and Source of Funds, 2007 (billions) Out-of-pocket $23b 3% Medicaid $120b 17% Medicaid $33b 7% Other public $68b 10% Private $257b 37% Medicare $196b 28% Hospital Care Total: $697b Out-of-pocket $50b 10% Other public $32b 7% Medicare $96b 20% Private $237b 49% Physician and Clinical Services Total: $479b Source: M. Hartman, A. Martin, P. McDonnell et al., “National Health Spending in 2007: Slower Drug Spending Contributes to Lowest Rate of Overall Growth Since 1998,” Health Affairs, Jan./Feb. 2009 28(1):246–61. THE COMMONWEALTH FUND