CTV-B (ext. iliac LNs)
advertisement

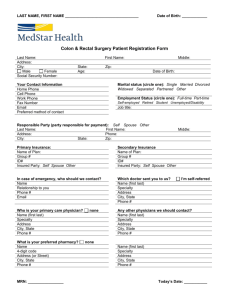
Target volume delineation of rectal and anal carcinoma: what are the differences? By Ola Mousa Elnady Assistant Lecturer of clinical oncology and nuclear medicine, MUH. Anatomy of the rectum • Length ranges from 12-15 cm (Figure 1). • It is divided to upper, middle ,and lower thirds. • Rectum begins at recto-sigmiod junction opposite S3 vertebrae (buttom of sacroiliac joint), ends at anorectal ring 1 inch below coccyx (at the level of ischial tuberosity) (Figure 2). • It forms 3 curvatures: lateral (RT, LT), perineal, and sacral curvatures (Figure 3). • Mesorectum: is adipose tissue around the rectum carrying lymphovascular ,and neurological supply, and encapsulated by fascia. • The peritoneum covers the upper third only then reflects to form the recto-vesical pouch in male, recto-uterine pouch in female. • Historically, tumors below the peritoneal reflection have been treated as rectal cancers, while tumors above treated as colon cancers. • Recently, location of rectal t. is defined by distance from lower edge of t. to anal verge, which is determined accurately by rigid endoscopy. • European and North American trials, have used a cutoff of 16 or 12 cm above the anal verge (respectively) to define rectal tumors. Figure 1 : length, divisions of rectum. Figure 2 : rectal anatomy (coronal view). Figure 3 : rectal anatomy (sagittal view). Spread of rectal cancer Figure 4 : lymph node spread of rectal cancer. Anatomy of the anal canal • The anal canal extends from anorectal ring superiorly to anal verge distally. • With an average length of 4 cm (4.2 cm in male, 3.8 cm in female). It is surrounded by the internal and external anal sphincter muscle. • The superior border is the anorectal ring, which is located ~2 cm superior to the dentate line. The transitional zone of the anus between the dentate line and anorectal ring is where columnar epithelium of the rectum meets the squamous epithelium of the anus. It includes the columns of Morgagni. • The distal end, i.e., anal verge is the junction of the nonkeratinized squamous epithelium of the anal canal and the keratinized hairy skin (Figure 5). Figure 5 : anatomy of anal canal (coronal view). Spread of anal canal cancers Figure 6 : lymph node spread of anal canal cancers (intramural system of lymphatics ). Rectal cancer Staging PRIMARY TUMOR (T) • • • • • • • • Tx: Primary tumor cannot be assessed T0:No evidence of primary tumor Tis: Carcinoma in situ: Intraepithelial or invasion of lamina T1: Invasion of submucosa T2: Invasion of musculosa T3: Invasion into perirectal tissue T4a: Invasion to the surface of visceral peritoneum T4b: Invasion of or adherence to adjacent organs or structures LYMPH NODES (N) • Nx: Regional LNs cannot be assessed • N0: No regional LN metastasis • N1a: Regional LN metastasis in 1 node • N1b: Regional LN metastasis in 2-3 nodes • N1c: tumor deposits in subserosa, mesentry, non-peritonealized perirectal tissue + N0 • N2a: Regional LN metastasis in 4-6 nodes • N2b: Regional LN metastasis in more than 7 DISTANT METASTASIS (M) • Mx: Distant metastasis cannot be assessed • M0: No distant metastasis • M1a: Distant metastasis confined to one organ (liver, lung, bone, non regional LN) • M1b: Distant metastasis in more than organ or the peritoneum Anal cancer staging PRIMARY TUMOR (T) • Tx: Primary tumor cannot be assessed • T0:No evidence of primary tumor • Tis: Carcinoma in situ: Intraepithelial or invasion of lamina • • • • T1:tumor less than 2 cm in greatest dimension T2: tumor 2-5 cm in greatest dimension T3: tumor more than 5 cm in greatest dimension T4: tumor of any size invades adjacent organs LYMPH NODES (N) • Nx: Regional LNs cannot be assessed • N0: No regional LN metastasis • N1: metastasis in perirectal LNs • N2: Metastasis in unilateral internal iliac and/or unilateral inguinal lymph node(s) • N3: Metastasis in perirectal + inguinal lymph nodes and/or bilateral internal iliac and/or bilateral inguinal lymph nodes DISTANT METASTASIS (M) • Mx: Distant metastasis cannot be assessed • M0: No distant metastasis • M1: Distant metastasis (including seeding of the peritoneum and positive peritoneal cytology) Stage grouping of anal carcinoma Treatment guidelines for rectal cancer Stage I (T1-2 N0 M0) Transanal rectal preserving excision if fulfilling criteria If proved to be higher stage should do LAR or APR & receive adjuvant CCRT & CTH Stage II & III (T3-4 or N+) Preop. CCRT surgery Adjuvant CTH Surgery Postop. CCRT Adjuvant CTH Stage IV If amenable to surgical resection : may benefit from aggressive local therapy with preoperative chemoradiation therapy, followed by surgical resection of both primary and metastatic lesions, adjuvant CTH . If not resectable : CTH +\- targeted therapy . Locally recurrent disease : mainly in low pelvis & presacral Resectable As new primary Unresectable CRT or CTH surgery if become resectable Treatment guidelines for anal cancer Stage I (T1 N0 M0) Wide local excision if fulfilling criteria If R+ resection should receive RTH, with or without CTH. Stage II & III (T2-4 or N+) definitive CCRT is main ttt, equal to APR in terms of OS but with sphincter preservation. Surgery after CCRT adds no benefits as proved by RTOG. Locally recurrent or resistant T after CCRT : Salvage APR ( with groin dissection in inguinal LN metastasis) provides 5 ys OS 50%. Radiation technique of rectal cancer Patient position: prone on belly board for anterior displacement of bowel or Supine. Comfortably full bladder may also reduce the dose to small bowel, will be reproducible (by emptying the bladder then drinking 200 ml of water 20 min before planning). Immobilization : by laser lines. CT simulation: • With I.V. contrast . • With or without oral contrast 2 hours before CT scanning which may be helpful to identify the small bowel. •With a radiopaque anal mark at anal verge or below rectal tumor in neoadjuvant RTH. • Or with wire over perineal scar in adjuvant RTH after APR. CT cuts every 3 mm thickness from 1st lumbar vertebrae till below anal verge. Target Definition and Delineation: • 3DCRT to deliver proper dose to the target volume with the least dose to the risk structures • IMRT not routinely used • MRI or PET/CT can help in delineation by showing the extent of the primary tumor and the regional LNs metastasis Target volume (neoadjuvant RTH): The RTOG anorectal contouring atlas provides contouring descriptions of three elective CTVs . CTV-A: includes rectum, mesorectum carrying primary tumor with the perirectal, presacral, and internal iliac LNs and should be covered in all patients with rectal cancer. CTV-B: includes the external iliac nodes (covered only in rectal cancer cases with T4 disease involving anterior pelvic structure ). CTV-C: includes the inguinal LNs (should be considered in rectal cancer cases that extend into the distal anal canal or lower third vagina). CTV-A (upper pelvis): • starts at L5-S1 to include presacral space, internal iliac LNs just after bifurcation of common iliac Vs. • Ant. extends 1-2 cm ant. to sacrum to include presacral space, 7 mm at least around int. iliac Vs. • Post. just in front of sacral bone. • Lat. till sacroiliac joints, stop at medial borders of psoas major ms. CTV-A (mid pelvis): • It includes rectum with mesorectum, int. iliac LNs. • Ant. CTV includes 1 cm from ant. organ as internal margin (bladder, SV, prostate, uterus). • Posterolateraly ,it includes till pelvic side wall ms, bone. • It includes 7 mm at least around internal iliac Vs to encompass int. iliac LNs. CTV-A (lower pelvis): • Should include entire mesorectum down to pelvic floor ms (beginning of anal canal if not involved) OR at least 2 cm below gross disease. • Lateraly, only few mm beyond levator ani ms is enough unless there is invasion of ischiorectal fossae, then we should cover all invaded area with 1-2 cm safety margin. CTV-B (ext. iliac LNs) • Delineated only in T4 tumors involving anterior pelvic organ (bladder, prostate, SV, uterus, cervix). • Cranially, it is delineated with int. iliac LNs after bifurcation of common iliac Vs then it starts to migrate anteriorly , covered by 7 mm at least around ext iliac Vs. • Caudally, it ends at level of femoral heads. CTV-C (inguinal LNs) • Included only in T4 tumors with distal anal canal or lower vaginal extension. • It starts cranially at femoral heads or superior pubic ramus just below level of end of ext. iliac LNs. • Caudally, till below ischial tuberosity. • Covered by margin 1-2 cm around femoral Vs. Target volume (adjuvant RTH): • It is just the same as neoadjuvant RTH , divided to CTV-A, CTV-B, CTV-C but observe: • Cranially start at L5-S1 or 1 cm cranial to anastomosis whichever is most cephalid. • Caudally, should include whole mesorectal bed till pelvic floor or 1 cm below anastomosis whichever is most caudal. • If post APR, should cover whole perineum till perineal scar. PTV • Each CTV should be expanded by 0.5–1 cm, depending on the physician’s comfort level with setup accuracy, frequency of imaging. OAR : • The organs at risk include the small bowel, large bowel (OR bowel bag), bladder, femoral heads. • Uniform consensus guidelines for contouring the small and large bowel, bladder, and femoral heads are available from an RTOG consensus panel. • Suggested dose tolerence from QUANTEC and RTOG 0822 : Dose and Fractionation: • For neoadjuvant RTH: • Conventional fractionation to a total dose of 45 Gy to the entire pelvis, followed by a boost of 5.4 Gy to the tumor is recommended, using high-energy (≥6 MV) photons. Patients with T4 disease or low-lying tumors may be boosted to a total dose of 54 Gy. • For adjuvant RTH: • Conventional fractionation to a total dose of 45 Gy to the entire pelvis, followed by a boost of 5.4 Gy to the tumor bed is recommended, using high-energy (≥6 MV) photons. Boost to a total of 54 Gy if positive margin or persistant T4 tumors after neoadjuvant TTT. Treatment Planning: A Box technique or better three-field arrangement (two laterals and a posterior– anterior [PA]) allows some sparing of the anterior pelvic structures such as small bowel, bladder, and the external genitalia. Wedges or other beam modifiers are used on the lateral beams to improve dose homogeneity Plan Assessment • Ideally, at least 95 % of each PTV should receive 100 % of the prescription dose. In addition, the maximum dose in the PTV should be <110 %. • When evaluating plans with a sequential boost to the gross disease, each individual plan should be evaluated before the “plan sum” to assess for areas that may be over- or under-dosed. Radiation technique of anal cancer Patient position: Supine with immobilization devices OR prone on belly board (but ttt of inguinal LN by electron, bolus can’t be done). CT simulation: The same as rectal ca (anal or perineal mark / IV with or without oral contrast / comfortably full bladder). • Target volume: The RTOG anorectal contouring atlas provides the same three elective CTVs as rectal ca. but the difference is that all 3 CTVs included in all cases of anal ca. but with different doses depending on stage (early or late). CTV-A :includes rectum, mesorectum, perirectal LNs, anal canal carrying primary tumor with the perianal, presacral, and internal iliac LNs. CTV-B: includes the external iliac nodes. CTV-C: includes the inguinal LNs. • Doses and Fractionation of different phases: usually it’s given on 3 phases (differs from early& advanced stage). • Early stage (T1,2 N0): • PHASE 1: 36 Gy/4ws (Low risk CTV) include presacral, int. iliac LNs till buttom of sacroiliac joint, whole ext. iliac LNs, inguinal LNs. PHASE 2: till 45 Gy/1.8/ fraction (high risk CTV) include mesorectum, rectum, anal canal, int. iliac LNs from below sacroiliac joint. PHASE 3: boost on gross anal tumor (GTV-P) could be given for T2 tumors till 50.4 Gy. • advanced stage (T3,4 / N+): PHASE 1: 36 Gy/4ws (low risk CTV) include presacral, int. iliac, ext. iliac LNs till buttom of sacro-iliac joint. PHASE 2: till 45 Gy/1.8 / fraction (high risk CTV) include mesorectum, rectum, anal canal with perirectal LNs, uninvolved int., ext. iliac LNs from below sacroiliac joint, uninvolved inguinal LNs. PHASE 3: boost on gross anal tumor and any involved LNs (GTV-P/ GTV-N) should be given till 50.4 - 54 Gy . • CTV-P / CTV-N: • CTV-P should cover the GTV-P with 1.5–2.5 cm margin expansion but excluding uninvolved bone, muscle, or air. The CTV-N should cover the GTV-N with a 1.0–1.5 cm margin but excluding uninvolved bone, muscle or air. • PTV: • Each CTV should be expanded by 0.5–1 cm, depending on the physician’s comfort level with setup accuracy, frequency of imaging. • NB: • RTOG 0529 (IMRT of locally advanced anal ca., 2013) does not differentiate between highand low-risk regions so late stage anal ca. treated by only 2 phases: • The first phase till 45 Gy / 5 ws. • The boost on gross disease till 50 or 54 Gy. • OAR : • The same as rectal ca but pelvic BM could be added to minimize acute hematologic toxicity in patients receiving concurrent chemoradiotherapy for anal cancer. Delineation of the pelvic bone marrow structure is described by Mell et al. ( 2006). The pelvic bone marrow consists of 3 subsites: the ilium, the lower pelvis, and the lumbosacral spine which is the most important site to be protected, mean dose should be <28 Gy. • Femoral heads: should be outlined from its top down to the interface between the greater and lesser trochanters, including notch of nutrient artery. • Bowel bag: including all small, large intestinal loops within the peritoneal space starting from 5-6 cm above PTV till its caudal end. • Treatment Planning: • Plan Assessment: The same as rectal cancer. • NB: slow regression of gross primary anal tumor is common, complete response of anal ca. may take 12 ms after end of CCRT to happen. Pelvic irradiation complications: Toxicities and complications depend on the site, volume irradiated ,and concomitant CTH. Acute effects include diarrhea, abdominal discomfort/pain, increased frequency of urination, dysuria, and skin irritation. Chronic or late toxicities include loose stools, rectal urgency, infertility, ovarian dysfunction for premenopausal women, vaginal stenosis, pelvic hair loss, dry ejaculation for men, femoral head fracture, and a small risk of late, secondary radiation-related malignancy. THANK YOU