epistaxis - Barnsley VTS
advertisement

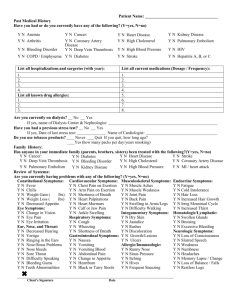
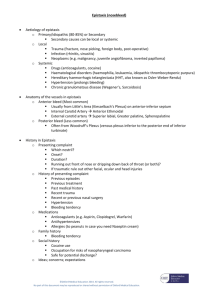
EPISTAXIS VTS presentations April 2013 Elisabeth Maskrey EPISTAXIS CAN BE SERIOUS …… Epistaxis – the facts • ~ 60 % of the general population has had at least one episode of epistaxis • only 6% sought medical help • 1.6 in 10,000 required hospitalisation • the incidence peaks < 10 and >50 years • rare in children < 2 years, if present is often associated with injury or serious illness • Types: • anterior bleeding • posterior bleeding • may present as hematemesis,nausea, anemia, hemoptysis,melena Epistaxis - risk factors • climate • deviated nasal septum • Trauma • inflammation • irritant chemical exposure • Disorders of platelet function • Drugs • Abnormalities of blood vessles - elderly arteriosclerotic vessels, hereditary haemorrhagic telangiectasia (Osler-Rendu-Weber syndrome) • Malignancy of the nose - juvenile angiofibroma • Wegener's granulomatosis and pyogenic granuloma Epistaxis – Hx, examination and Investigations ABC to confirm haemodynamic stability Hx • laterality, duration, frequency, and severity • PMHx including any conditions predisposing to bleeding - coagulopathies • current medication - aspirin or warfarin • FHx of bleeding disorders • history of recent trauma or surgery • presence of unilateral symptoms like nasal obstruction, rhinorrhea, facial pain, or evidence of cranial neuropathies (facial numbness, double vision) indicating benign or malignant sinonasal neoplasms Examination • Ideally Thudicum nasal speculum under adequate lighting to identify bleeding points • if a blood clot is present, advice the patient to blow their nose (with caution) or suction • topical sprays containing a combination of anesthetics and vasoconstrictors can be used to control bleeding Investigations • Sever hemorrhage – FBC, coag, G&S and CXM • On warfarin - FBC, coag • Systemic conditions – LFT and U&E Management Direct pressure • Sit patient upright, leaning slightly forward • Patient squeezes the bottom part of the nose (NOT the bridge of the nose) for 10-20 minute • Monitor HR and BP • If bleeding has stopped after this time inspect the nose using a nasal speculum and consider cautery. Cauterisation • Apply a silver nitrate cautery stick for 10 seconds • working from the edge and moving radially • Never both sides of the septum at the same session. Cream (Naseptin) • Cautery and cream are equally effective for the treatment of epistaxis. • Application of a cream-based treatment may initially be easier and more practical, particularly in children Management Anterior packing • nasal tampon • absorbs blood, swells and the tight fit reduces flow. • Lubricate the tampon with K-Y Jelly or Naseptin cream • secure the tampon thread to the cheek • Pack the other side as well. • Packs are generally left in place for 24 hours. • Can also use 1 cm ribbon gauze impregnated with petroleum jelly . Both ends of the gauze should protrude from the nostril. Posterior bleeds • May require ENT input • packing and a balloon catheter can be useful • Opiate analgesics to relieve discomfort and reduce elevated blood pressure due to posterior pack. • Ligation of the sphenopalatine artery endoscopically. Management Complications of packing • • • • • Anosmia Pack falling out and continued bleeding Breathing difficulties and aspiration of clots Posterior migration of the pack causing airway obstruction and asphyxia Perforation of the nasal septum or pressure necrosis of cartilage Summary • If sever get specialist help • For recurrent cases consider underlying causes • Can be managed quickly and easily in most cases Template Provided By www.animationfactory.com 500,000 Downloadable PowerPoint Templates, Animated Clip Art, Backgrounds and Videos