Preparticipation Physical Exam - American College Health Association
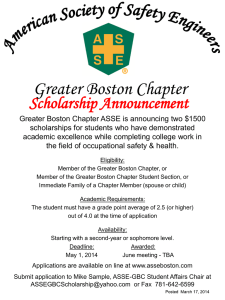
advertisement

Sudden Cardiac Death causes and screening in college athletics Matthew Pecci, MD Assistant Professor in Family Medicine Director of Sports Medicine Boston University Objectives Boston University Slideshow Title Goes Here • Scope of the problem • Review the most common causes of SCD in the US • Review current consensus on preparticipation(PPE) screening • Review the pros and cons of the addition of ECG screening to the PPE exam SUDDEN DEATH Boston University Slideshow Title Goes Here • Sudden death in athletics can occur from direct or indirect causes • direct - traumatic • indirect - atraumatic SUDDEN DEATH Boston University Slideshow Title Goes Here • Most indirect causes are cardiac in origin. • A very small number of indirect causes of sudden death are noncardiac • • • • heat stroke CVA pulmonary embolus drug abuse SUDDEN DEATH Boston University Slideshow Title Goes Here • From 1931 to 1986 direct causes of sudden death outnumbered indirect cause by 2 to 1. • From 1982 to the present this has reversed with indirect causes now outnumbering direct causes by 2 to 1. SUDDEN CARDIAC DEATH Boston University Slideshow Title Goes Here • Sudden cardiac death (SCD) in athletes: • nontraumatic, nonviolent, unexpected death due to cardiac causes within one hour after the onset of symptoms, and occurring within one hour of sports participation SCD EPIDEMIOLOGY Boston University Slideshow Title Goes Here How prevalent a problem is SCD? SCD Incidence Boston University Slideshow Title Goes Here • Incidence of SCD in US is unknown • Studies to date have relied on surveys, and nonmandatory reporting systems that may underestimate the true incidence • There has been some push from the sports medicine community for a national registry • National Center for Catastrophic Sports Injury • US National Registry of Sudden Death in Athletes SCD Incidence Boston University Slideshow Title Goes Here • Van Camp et al • • • • SCD in HS and college athletes 1983-1993 Identified by media reports and newspaper clippings 100 cases of SCD Estimated number of athletes based on HS and college participation rates • SCD rate 1:300,000 annually 1. Van Camp SP, Bloor CM, Mueller FO, Cantu RC, Olson HG. Nontraumatic sports death in high school and college athletes. Med Sci Sports Exerc. 1995;27:641– 647. SCD Incidence Boston University Slideshow Title Goes Here • Maron et al • • • • • 1. Minnesota HS athletes Mandatory insurance for catastrophic death in HS athletes 12 year period, grades 10-12 3 cases of SCD occurred during study period Rate of SCD was 1:200,000 participants annually Maron BJ, Gohman TE, Aeppli D. Prevalence of sudden cardiac death during competitive sports activities in Minnesota high school athletes. J Am Coll Cardiol. 1998;32:1881–1884. SCD Incidence Boston University Slideshow Title Goes Here • Maron et al • SCD over 27 year period in athletes up to age 39 • Identified cases of SCD through various sources – news media, internet, direct reports, etc • 1866 cases identified, in 1353 cause of death determined • Rate of SCD 1:164,000 participants annually 1. Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980–2006. Circulation. 2009;119:1085–1092. SCD Incidence Boston University Slideshow Title Goes Here • Eckart et al • • • • • 1. SCD in military recruits over 25 year period Ages 18-35 Mandatory reporting of all deaths Autopsy confirmation of cause Rate of SCD 1:9,000 recruit-years Eckart RE, Scoville SL, et al. Sudden death in young adults: a 25-year review of autopsies in military recruits. Ann Intern Med. 2004;141(11):829–834 SCD Incidence Boston University Slideshow Title Goes Here • Harmon et al • • • • • • 1. SCD in NCAA student-athletes over 5 year period Identified by NCAA database, media reports, and insurance claims 273 death with 45 SCD Incidence SCD 1:43,770 participants per year Breakdown by sport, sex, and race Div 1 men’s basketball SCD rate 1:3100 per year Harmon KG, Asif IM, Klossner D, Drezner JA. Incidence of Sudden Cardiac Death in National Collegiate Athletic Association Athletes. Circulation. 2011;123:1594-1600. SCD Incidence Boston University Slideshow Title Goes Here • Incidence likely somewhere in between • Based on available data experts estimate the true incidence of SCD in the US is 1 in 75,000 SCD Boston University Slideshow Title Goes Here What is the most common cause of SCD in athletes? SCD Boston University Slideshow Title Goes Here • Over age 35 - 90% of SCD are due to coronary artery disease • In many cases the athlete has no known history of disease • Acute plaque rupture SCD Boston University Slideshow Title Goes Here • Cause of SCD in athletes less than 35yrs • • • • • 36-50% hypertrophic cardiomyopathy 10-19% coronary artery anomalies 6% myocarditis 5% ruptured aorta (Marfans syndrome) <5% aortic stenosis, right ventricular dysplasia, CAD, Ion channel disorders HCM Boston University Slideshow Title Goes Here • Hypertrophic cardiomyopathy • Clinically recognized in 1 in 500 in the general population (0.2%) • Genes mutations on at least 12 genes which code components of the heart muscle fibers • Autosomal dominant with variable expression • Myocardial disarray, myocardial scarring HCM Boston University Slideshow Title Goes Here • Classic findings: • • • • LV wall thickness of 16mm or more (nl < 12mm) vast disarray of the walls affected and extent of hypertrophy septum to free wall ratio >1.3 Small LV cavity size < 45mm with impaired diastolic function Boston University Slideshow Title Goes Here HCM Boston University Slideshow Title Goes Here • Functional findings: • impaired filling of the LV during diastole due to small cavity size • abnormal flow across the mitral valve • pressure gradient to blood flowing into the aorta due to thickened septum HCM Boston University Slideshow Title Goes Here • Incidence of SCD in HCM • 2-4% / year in adults • 4-6% / year in children and adolescents HCM Boston University Slideshow Title Goes Here • Causes of SCD in HCM - speculative • Arrythmia - ventricular tachyarrythmias • hypotension from diastolic dysfunction and outflow tract obstruction • myocardial ischemia Screening for HCM Boston University Slideshow Title Goes Here • Can we identify HCM in an athlete before it causes SCD? • Family history – autosomal dominant • symptoms - syncope, CP, fatigue, dyspnea • physical exam findings HCM Boston University Slideshow Title Goes Here • Most athletes are asymptomatic and their sentinel event is SCD • Estimated that only 21% of athletes with HCM have signs or symptoms1 1. Maron BJ, Shirani J, et al. Sudden death in young competitive athletes. Clinical, demographic, and pathological profiles. JAMA. 1996;276(3):199–204 HCM Boston University Slideshow Title Goes Here • Physical exam - murmur from outflow obs. • Harsh, mid systolic • heard best at right upper sternal border • decreases in intensity with increased blood flow to the heart i.e. squatting, lying down • increase in intensity with decreased blood flow to the heart i.e. Valsalva, standing • Estimated that only 25% of HCM patients have a murmur Is an ECG helpful? Boston University Slideshow Title Goes Here • An ECG will be abnormal in 75-95% of patients with HCM • • • • wide array of abnormalities prominent Q waves deep negative T waves increased QRS voltage associated with ST depression or T-wave inversion. Is an echocardiogram helpful? Boston University Slideshow Title Goes Here • Echocardiography remains the standard to confirm the diagnosis of HCM • • • • identifying pathologic LV wall thickness (>16 mm) a non-dilated LV with impaired diastolic function Septum to free wall ratio > 1.3 Changes may not be apparent until physical maturity Boston University Slideshow Title Goes Here HCM diagnosis uncertainty Boston University Slideshow Title Goes Here • In cases where the diagnosis of HCM is uncertain (ie, borderline LV wall thickness) • Cardiac magnetic resonance imaging (MRI) • Genetic testing • Repeat echocardiogram after 4 to 6 weeks deconditioning • deconditioning should resolve the hypertrophy in an athletic heart and may help in distinguishing from HCM. HCM and participation Boston University Slideshow Title Goes Here • No single clinical, morphologic, or electrophysiologic feature has been found to be a reliable predictor of SCD in patients with HCM • 36th Bethesda Conference: • “present recommendations for sports eligibility remain conservative and homogeneous for those athletes within the diverse HCM clinical spectrum” • “Broad recommendation to exclude such individuals from competitive sports will, by definition, deny participation to some unnecessarily” Maron BJ, Zipes DP, et al. 36th Bethesda conference. Journal of the American College of Cardiology. 2005;45(8):1317-75. HCM and participation Boston University Slideshow Title Goes Here • 36th Bethesda recommendations: “Athletes with a probable or unequivocal clinical diagnosis of HCM should be excluded from most competitive sports, with the possible exception of those of low intensity (class IA). This recommendation is independent of age, gender, and phenotypic appearance, and does not differ for those athletes with or without symptoms, LV outflow obstruction, or prior treatment with drugs or major interventions with surgery, alcohol septal ablation, pacemaker, or implantable defibrillator.” Boston University Slideshow Title Goes Here Coronary Artery Anomalies Boston University Slideshow Title Goes Here • The right and left coronary arteries arise from the aortic sinuses and are responsible for blood supply to the heart • a small percentage of people have arteries which originate in atypical locations • certain of these atypical arterial originations may affect blood flow to the heart Coronary Artery Anomalies Boston University Slideshow Title Goes Here • Most common anomaly leading to SCD: • left coronary from the right sinus of valsalva - causes a severe angle in the artery which disrupts blood flow • Others: • hypoplastic coronary arteries • tunneled epicardial arteries Boston University Slideshow Title Goes Here Coronary Artery Anomalies Boston University Slideshow Title Goes Here • • • • • Cause of death is from myocardial ischemia Very difficult to detect with screening No genetic component No exam findings Small percentage may have symptoms - review of 78 cases - 62% asymptomatic Boston University Slideshow Title Goes Here Questions? SCREENING for SCD Boston University Slideshow Title Goes Here • No outcome based study exists on the effectiveness of the PPE • The American Heart Association recommends a detailed history and exam consisting of 12 items1 • The 4th edition PPE monograph endorses the AHA recommendations2 1. Maron BJ, Thompson PD, et al. Recommendations and considerations related to preparticipation examination screening for cardiovascular abnormalities in competitive athletes: a 2007 update. Circulation. 2007;115(12):1643-55. 2. American Academy of Family Physicians , American Academy of Pediatrics , American College of Sports Medicine , et al. Preparticipation Physical Evaluation. In: Roberts W, Bernhardt D editor. 4th edition. Elk Grove (IL): American Academy of Pediatrics; 2010; SCREENING for SCD Boston University Slideshow Title Goes Here • Personal History: • Exertional chest pain • Unexplained syncope or near syncope • Excessive exertional and unexplained dyspnea/fatigue associated with exercise • Prior recognition of a heart murmur • Elevated systolic blood pressure SCREENING for SCD Boston University Slideshow Title Goes Here • Family History: • Premature death(sudden and unexpected, or otherwise) before age 50 years due to heart disease, in 1 or more relatives • Disability from heart disease in a close relative <50 years of age • Specific knowledge of certain cardiac conditions in family members: hypertrophic or dilated cardiomyopathy, long QT syndrome or other ion channelopathies, Marfan syndrome, or clinically important arrhythmias SCREENING for SCD Boston University Slideshow Title Goes Here • Additional questions in PPE monograph: • • • • Does your heart ever race or skip beats? Has your doctor ever ordered tests for your heart? Have you ever had an unexplained seizure? Do you get more tired or short of breath more quickly than your friends during exercise? • Family history of unexplained or unexpected death prior to age 50 including drowning, unexplained car accidents, SIDs • Family member with a pacemaker or implantable defibrillator • Family member with unexplained seizures, fainting or near drowning SCREENING for SCD Boston University Slideshow Title Goes Here • Physical exam: • • • • Auscultation for a murmur (sitting and standing) Femoral pulses to exclude aortic coarctation Stigmata of Marfans syndrome Brachial artery BP (sitting) SCREENING for SCD Boston University Slideshow Title Goes Here • AHA recommendation compliance: • In 2000 only 26% of NCAA schools had forms containing at least 9 of the 12 items • In 2005 48 states had approved forms for high schools and 39 of these forms had at least 9 items • In 2010 a survey to the Washington chapter of AAP, AAFP, and high school ADs only 6% of providers and 0% of schools were compliant. Only 47% of physicians and 6% of ADs reported awareness of the guidelines.1 Madsen NL, Drezner JA, Salerno JC. Sudden death screening in adolescent athletes: an evaluation of compliance with national guidelines. Br J Sports Med 2013; 47:172-77 SCREENING for SCD Boston University Slideshow Title Goes Here • What should colleges do? • Make sure forms contain recommended history and exam items • If you are performing your own PPEs make sure you have qualified examiners who are aware of the guidelines • If you are not performing your own PPEs make sure forms are adequately reviewed and if there are any questions athletes reexamined ECG Screening in the USA Boston University Slideshow Title Goes Here • 2007 consensus statement by the American Heart Association recommended not to screen athletes with an ECG • “Admirable proposal deserving serious consideration”, “many epidemiologic, social, economic, and other issues” which impact this screening proposal in the US • The 4th edition Pre-participation examination monograph does not recommend for or against ECG screening ECG and the Italian Data Boston University Slideshow Title Goes Here • Mandatory screening of competitive athletes with history, physical and ECG begun in 1982 • Population-based observational study • Incidence of SCD in athletes in prescreening (197981), early screening (1982-92), and late screening (1993-2004); causes of SCD • Incidence of SCD in athletes decreased by 89%, 10 fold decrease in deaths from cardiomyopathies Corrado D, Basso C, Pavei A, et al. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA. 2006; 296:1593– 1601. ECG and the Italian Data Boston University Slideshow Title Goes Here • Based on the Corrado study the European Society of Cardiology and the International Olympic Committee now recommend ECG screening as part of the Preparticipation exam Pelliccia A, Fagard R. Bjørnstad HH, et al. A European Society of Cardiology consensus document: recommendations for competitive sports participation in athletes with cardiovascular disease. Eur Heart J. 2005;26:1422–1445. No ECG Rationale Boston University Slideshow Title Goes Here • • • • • • Italian data Scope of problem in US ECG Specificity Cost Challenge of mass screening Ethical considerations for testing Italian Data Boston University Slideshow Title Goes Here • Not controlled • Mandatory H+P, and ECG all implemented in 1982 • High prescreening annual death rate in athletes of 3.6/100,000 person years somewhat accounts for the large change with screening • Lowest death rate 0.4 death/100,000 person years is similar to reported death rates of HS and college athletes in US without the use of ECG screening Italian Data Boston University Slideshow Title Goes Here • 44% of the disqualifications were from high blood pressure and valvular heart disease which presumably can be identified without an ECG • Unclear from data how many of the cardiomyopathies were diagnosed from history vs exam vs ECG • Decreased in death rate from cardiomyopathies during the study period was mainly due to ARVC not HCM • 24 of the 55 athletes who died during the study period had 1 or more positive findings (FH, palpitations, syncope, chest pain, murmur, or ECG findings) Scope of problem in US Boston University Slideshow Title Goes Here • Unknown • No national reporting system – we don’t know the numbers of cases of SCD or how many competitive athletes in US at any given time • Presumed low incidence Specificity of ECG Boston University Slideshow Title Goes Here • 7% false positive rate in Italian study with ECG analyzed by sports cardiologists • Studies in US using ECG at PPEs report 10%-25% abnormal ECGs requiring further evaluation • Study at Harvard over 3 years adding ECGs to screening had 16.9% false positive rate1 1.Baggish AL, Hutter AM, et al. Cardiovascular screening in college athletes with and without electrocardiogram. Ann Intern Med 2010;152:269-75 Cost of ECG Screening Boston University Slideshow Title Goes Here • Cost projection model in US based on the Italian data: • Annual cost of $2.5 to $3.4 billion dollars • Estimates 4,813 lives saved over a 20 year period • $10.4 to $14.4 million per life saved Halkin A, Steinvil A, et al. Preventing sudden death of athletes with electrocardiographic screening:what is the absolute benefit and how much will it cost? J Am Coll Cardiol. 2012;60(22):2271-76 Cost of ECG Screening Boston University Slideshow Title Goes Here • 5 year ECG screening program at the University of Virginia: • • • • • Screened 1,473 athletes over 5 years 5 significant cardiac abnormalities found(one long QT, no HCM) ECG abnormal in 275 resulting in 359 additional tests Cost of history and physical screening $343,725 Adding ECG cost and testing cost additional $551,145 Malhotra R, West JJ, et al. Cost and yield of adding electrocardiography to history and physical screening Division I intercollegiate athletes: a 5-year experience. Heart Rhythm. 2011;8(5):721-7. Cost of ECG Screening Boston University Slideshow Title Goes Here • 10 million middle and high school athletes would be eligible for screening annually • $25 H+P, $50 for ECG then assume 15% need further evaluation including cardiologist visit $100, echo $400 • Minimum annual cost of 2 billion dollars which does not factor into the administrative costs of such a large scale program Large scale US screening Boston University Slideshow Title Goes Here • Difficult to make consensus recommendations if there is no consistent infrastructure for implementation • Lack of widespread sports medicine infrastructure in both high schools and colleges in US: • Untrained examiners more false positives • Selective or unequal implementation based on socioeconomic status or profile of college/sport • Social and medico legal consequences Large scale US screening Boston University Slideshow Title Goes Here • Survey study of NCAA Div. I Football programs: • 35 of 74 schools or 47% use non-invasive screening • Most use ECG but 17 also use echocardiograms • 30% utilize a cardiologist for these screenings • Would the response be the same for non-revenue sports or other division schools? Coris EE, Sahebzamani F, et al. Preparticipation cardiovascular screening among National Collegiate Athletic Association Division I Institutions. Br J Sports Med. 2013;47:182-4. Ethical Consideration Boston University Slideshow Title Goes Here • 879 athletes(30 cases of HCM) disqualified in the Italian study, none died of SCD at end of study period. • Did they assume a sedentary lifestyle or were they low risk for SCD anyway? • At least 3 cases were reported to have committed suicide • We do not know what characteristics of HCM make SCD more likely – “deny participation unnecessarily” • Do we want to commit athletes who may not be at risk for SCD to Class IA activities for the rest of their lives? Conclusions for No ECG in US Boston University Slideshow Title Goes Here • Incidence of SCD is low overall • Informed decision requires more information: • Need a national SCD registry – athletes, symptoms, screened • Data on specificity of revised criteria in untrained • Cost control measures • More info on the natural history of HCM • Controlled trials prior to widespread recommendation Bottom Line: ECG use at your school Boston University Slideshow Title Goes Here • Will pick up more asymptomatic and potentially lethal cardiac conditions • Need infrastructure to obtain ECGs, and trained interpreters • Need to accept consequences of more false positives: • • • • Cost of further work up Time for further work up Potential disqualification of equivocal cases Legal consequences of disqualification Conclusions Boston University Slideshow Title Goes Here • Difficult to identify the scope of the problem in the US • The most common causes of SCD in college aged athletes in the US specifically HCM • AHA and PPE monograph recommendations for history and physical screening – is your school compliant? • ECG controversy • Know how to respond to non traumatic syncope in the Boston University Slideshow Title Goes Here athlete - ABCs with initiation of CPR, immediate call for help, be familiar with the use of an AED Boston University Slideshow Title Goes Here Thank You! Myocarditis Boston University Slideshow Title Goes Here • Acute inflammation of the myocardium which can cause arrythmia and SCD • Coxsackie virus B believed to cause 50% of cases • Others viruses echovirus, adenovirus, influenza, Chlamydia • Present as typical viral illness followed by progressive exercise intolerance and congestive symptoms Myocarditis Boston University Slideshow Title Goes Here • ECG may show diffuse low voltage, ST-T wave changes, heart block, or ventricular arrhythmias. • Serologic testing may show leukocytosis, eosinophilia, an elevated sedimentation rate or C-reactive protein, and increased myocardial enzymes. • Echocardiography will confirm the diagnosis within the right clinical context showing a dilated LV, global hypokinesis or segmental wall abnormalities, and decreased LV ejection fraction. Myocarditis Boston University Slideshow Title Goes Here • Athletes may return to training and competition after a period of about 6 months if: • LV function, wall motion, and cardiac dimensions return to normal (based on echocardiographic and/or radionuclide studies at rest and with exercise) • clinically relevant arrhythmias such as frequent and/or complex repetitive forms of ventricular or supraventricular ectopic activity are absent on ambulatory Holter monitoring and graded exercise testing • serum markers of inflammation and heart failure have normalized • the 12-lead ECG has normalized. Persistence of relatively minor ECG alterations such as some ST-T changes are not, per se, the basis for restriction from competition. Marfans Syndrome Boston University Slideshow Title Goes Here • • • • • Disorder of connective tissue prevalence of 1 in 5,000 Genetic mutation in the gene coding fibrillin Individuals with Marfans are tall with long limbs i.e. basketball and volleyball athletes Marfans Syndrome Boston University Slideshow Title Goes Here • Body systems affected: • Skeletal - tall, arachnodactyly, high arched palate, hyperextensable joints, scoliosis, chest deformity • Skin - stria • Ocular - retinal detachment, myopia, lens subluxation (60% of cases) • Pulmonary - spontaneous pneumothorax Marfans Syndrome Boston University Slideshow Title Goes Here • CV - ascending aorta dilatation, aortic dissection, aortic valve insufficiency, mitral valve prolapse or insufficiency, arrythmias • CV complications are the major cause of morbidity and mortality Marfans Syndrome Boston University Slideshow Title Goes Here • Exam findings: • • • • • • Arm span > height Reduced upper to lower body ratio pectus deformity hyperextensable joints murmurs - AI, MI, MVP skin - stria Marfans Syndrome Boston University Slideshow Title Goes Here • Ghent criteria – clinical features highly suspicious for Marfans • Diagnosis: • With + family history - positive features in at least 1 major systems • With - family history - positive features in at least 2 major systems Marfans Syndrome Boston University Slideshow Title Goes Here • All athletes highly suspicious for Marfans syndrome should have an echocardiogram which shows some abnormality 95% of the time, and a slit lamp which demonstrates lens subluxation 60% of the time. Marfans Syndrome Boston University Slideshow Title Goes Here • Class IA, or IIA activities if no aortic dilatation, no moderate aortic regurgitation, and no family history of dissection or SCD • Only class IA activities if any of these signs exist