fact sheet
advertisement

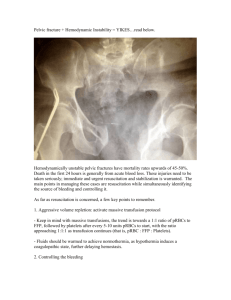
Pelvic Trauma Epidemiology Complications Classification Others Assessment Ix Mng Account for 3% of #’s; present in 30% multitrauma; 50% require blood transfusion; mostly MVA / falls; 5-20% mortality; 50% mortality if decr BP OA; 30% mortality if open Vascular: common iliac artery divides at SIJ int iliac (intrapelvic); if post ring involvement 2-3x blood requirement; can lose up to 4-6L blood; 15iu for APC, 9iu for VS, 3.5iu for LC; major cause of death; trt with pelvic sling (may decr pelvic vol by up to 10%) or mechanical fixation; bleeding from multiple sources in 60%, bilateral in 50%; most bleeding is low p venous bleeding and bleeding from bone edges; 10-15% are arterial (usually from int iliac; esp sup gluteal and obturator); shock and death usually due to arterial; if bleeding is refractory to resus, likely arterial and hence angiography should be persued Neural: lumbar and sacral plexus; S1-2 nerve roots commonly involved in post element #’s, assoc with sacral inj; impotence in 1/6th sacral #’s; lumbar root assoc with SIJ dislocation or # GU: bladder or urethral in 16%; urethral in 5%; usually in ant bulbous urethra; vaginal lac in 4% (techinically open if present); high fetal death rate; possible obstetric probs; if suspect, do retrograde urethrography before placing IDC GI: rectal inj uncommon (usually assoc with urinary inj and ischial #) Other: ruptured diaphragm See below; usually pubic symphysis breaks 1st sacrospinous lig and sacrotuberous lig ant SI lig Single break = stable inj; 2 breaks = unstable with risk of displacement Suggestive of LC: Horizontal #’s; SIJ diastasis and crush # of sacrum; central hip dislocation Suggestive of AP: vertical #’s; posterior hip dislocation Suggestive of VS: vertical #’s with vertical displacement Avulsion #: ASIS (sartorius; pain on flexion + abduction) Ischial tuberosity (hamstrings; non-union common; OT needed) AIIS (rectus femoris; can’t flex hip) Post spine (erector spinae) Iliac crest (direct violence) Acetabular #: 20%; transmission of force through femoral head via post / central / ant dislocation; usually due to MVA CT better than XR Usually treated with traction, but may need OT esp if displaced assoc with sciatic and femoral nerve inj, femoral #, knee inj Pelvic ring #: post # have higher incidence of vascular and neuro complications History: bladder, bowels Haematuria (blood at meatus, high riding prostate, boggy mass on PR), rectal, PV bleeding; abnormal bony prominence on PR; altered tone on PR Destot’s sign: haematoma above inguinal lig or in scrotum Roux’s sign: distance betweem gt trochanter and pubic symphysis unequal Earle’s sign: tender # line palpable on PR exam Grey-Turner’s sign: flank bruise due to retroperitoneal blood XR: 65-90% sens; pelvic inlet view for ant SIJ inj and AP displacement of ring #’s; pelvic outlet view for vertical displacement / transverse # through sacrum and arcuate lines; judet view for acetabular #; CT: needed for acetabular inj, pelvic ring disruption, post element #, single rami #, complex #; extravasation of contrast 80-90% sens, 98% spec for need for vessel embolisation Retrograde urethrogram: inject 200-300ml contrast Bladder poorly filled with extravasation to side: extraperitoneal rupture; conservative trt if small, OT if large Bladder doesn’t fill, extravasation to pelvic floor: membranous urethra rupture; needs cystoscopy Bladder doesn’t fill, extravasation beneath pelvic floor: bulbar urethra rupture Catheter: dry tap: intraperitoneal rupture Blood stained tap: extraperitoneal rupture ABC Stabilisation: doesn’t prevent arterial bleeding; may prevent dislodgement of existing clot; doesn’t support post pelvis; difficult if obese; assess for other causes of blood loss Pelvic sling: best if major disruption and opening of pelvic ring; CI IF LC / VS inj, isolated pubic rami #; don’t use >24hrs External fixation: quick and can be done in ED; use if pubic diastasis >2.5cm / involvement of post elements Pneumatic anti-shock garment: can be used pre-hospital; works in APC; may incr bleeding in LC; decr BP if sudden removal, compartment syndrome, decr access to legs Conservative: # bilateral pubic ramus with min displacement LC I / AP I non-displaced # ilium Traction: acetabular and VS #, using femoral pins LC I + II – bed rest and delayed ORIF External fixation within 4hrs if: APC II, III + VS, ?LC III, esp if opened >2.5cm anteriorly; effective for controlling venous bleeding (maybe pre-angio) OT vs angio: controversy exists about best practice; depends on facilities available but most unstable pelvic trauma should have angio over OT if there is no abdo injury causing bleeding OT: Internal fixation if: major visceral / vascular inj, ongoing blood loss, open Open surgery if: haemodynamically unstable + positive FAST; may need extraperitoneal packing as part of damage contro; can used as bridge for patients too unstable to survive angiography Angiography and embolisation if: continuing blood loss and other sources excluded (ie. Intra abdominal exlcuded; need for ongoing blood transfusion, haemodynamic status, certain amount of iu blood needed, positive helical CT) even if haemodynamically unstable; only CI’ed if needs laparotomy; takes 1-2hrs; bleeding successfully control in >90%; 7-10% #’s require embolisation; only useful if branches of int and ex iliac system involved (more likely if VS / APC injury as 20% have arterial haem; only 2% lat compression #’s have arterial haem) Pros: avoids retroperitoneal probs assoc with OT, preserves tamponade effect, avoids entering haematoma, more effective than OT for major arterial bleeding Cons: source of arterial bleeding only identified in 20-30% pts with severe pelvic disruption; when failure occurs, usually assoc with severe 2Y coagulopathy; complications = impotence, bladder / gluteal necrosis, sciatic / femoral nerve paralysis, emboli to normal vessels; not available in some hospitals; operator dependent; time consuming; doesn’t address venous blood loss; diagnostic and therapeutic; must not perform cystourethrography pre-angiography Usually assoc with pelvic ring #; can cause sacral nerve damage (weak legs, saddle anaesthesia, incontinence); CT more sens than XR Sacral # Key+Cornwell / Kane 0 I II III IV 30% 1x # (eg. Avulsion ASIS, # ramus, iliac wing) No break in pelvic ring Stable 1x break in pelvic ring (eg. 2x rami, SIJ #, pubic symphysis #) Stable 25% have major STI / visceral inj 2x break in pelvic ring Unstable Often STI / visceral inj Acetabular # Young LC #’s (Lat compression and int rotation) 50% I II MVA III APC # (antpost compression) 25% I MVA III II Bucholz 1x # pubic ramus Mortality 10% Pubic rami # + SI # No SI widening Mortality 25% Pubic symphysis diastasis with SI hinging Mortality 35% SIJ displacement Mortality 40% (if open) Most common (50%) Stable (4% bladder rupture) # sacrum on side of impact + pubic rami # 7% Unstable to int rotation (stability depends on degree of involvement of SIJ; 36% severe haem, 7% bladder rupture)) # iliac wing near SIJ (may enter SIJ) + pubic rami # 10% Unstable (60% severe haem, 20% bladder rupture, 20% urethral inj) Contralat AP compression inj (open book # ie. Ex rotation), ipsilat lat compression inj (ie. LC I/II) Symphysis diastasis slight widening of SIJ; ligs stretched but intact 8% bladder rupture, 12% urethral inj 10% Disruption of sacrotuberous and sacrospinous and ant SI ligs, intact post SI ligs widening of ant SIJ’s open book inj Lumbosacral plexus and vessels often injured (28% severe haem, 10% bladder rupture, 23% urethral inj) 4% VS # (vertical shear) 5% Axial load Mixed Complete disruption of hemipelvis with lateral displacement but without vertical displacement; all ligs disrupted Significant blood loss (53% severe haem, 15% bladder rupture, 36% urethral rupture) 5% Hemipelvis displacement superiorly (usually through SIJ) Need ant and post SI lig disruption for vertical instability: usually SIJ, vertical sacral # or ilial wing #, or complete lig disruption through PS/PR, interosseous + post SI ligs; may have L5 transverse process # Significant blood loss (75% severe haem, 15% bladder rupture, 25% urethral rupture) 20-25% Notes from: