here
advertisement

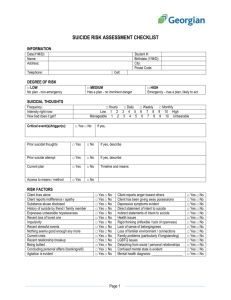
Keynote Presentation DR LEONARD LAMBETH Chief Psychiatrist, Dept. Health & Human Services Tasmania Suicide Prevention– It’s Everyone’s Business An Approach to Understanding & Prevention Assoc Prof. Len Lambeth BSc(Med), MBBS, FRANZCP, DAvMed ,Cert Forens Behav Science, AFRACMA Chief Psychiatrist, Mental Health, Alcohol and Drug Directorate The Problem • • • • Every year in Australia, suicide takes the lives of around 2000 Australians It is ahead of road traffic accidents and skin cancer as a cause of death For those aged 15-24, it is the NUMBER ONE cause of death. Suicide accounts for around 20% of all deaths in this age group and 25% for males in this group. National Context • Suicide Prevention Australia is the national peak body for the suicide prevention sector in Australia. • Plays a role in providing policy advice to governments, community awareness and public education, increased involvement in research and a future role in leading Australia’s engagement internationally. • LIFE Communications is a National Suicide Prevention Strategy project that aims to improve access to suicide and self-harm prevention activities in Australia through the promotion of the LIFE resources and website. • Also aims to improve communication and networks between suicide prevention stakeholders in Australia. Starting Points • • • • Suicide is a rare event overall Suicide and self-harm is not rare among psychiatric patients Suicide is hard to predict with any specificity It is very difficult to know and understand the thinking behind a suicidal act What Drives People to Suicide? • Understanding the person in the context of their unique environment is essential if we are to have any understanding of the drivers behind suicide. Some of the drivers include: – Mental health problems – Social disadvantage – Adverse childhood experiences – Physical health problems – Adverse life events – Legal problems – Loneliness A Personal Response • “I believe that each case of suicide has its own unique constellation of factors including, at its centre, the vital role of idiosyncratically defined psychological pain, which itself is pushed by a pattern of thwarted psychological needs that is special for that particular person”. • Schneidman, E., (2005) Suicide & Life-Threatening Behaviour. Vol 32 (1) An Ancient View “ Whensoever any affliction assails me, methinks I have the keys of my prison in my own hand and no remedy presents itself so soon to my heart as mine own sword.” Biathanatos – a treatise about the moral implications of suicide. (John Donne – 1602) Understanding Suicide • • • • Is understanding suicide achievable? Is it always associated with mental illness or disorder? Can we understand the underpinning emotions? Can we delineate the diverse and multifaceted underpinnings? Understanding Suicide • Biological - decreased serotonin, excess noradrenaline • Sociological – society’s influence on the individual (Durkheim); social dependency/gender role/ marital status (Hassan) • Psychological-psychodynamic (emotional states); cognitive (learned behaviour); family systems (family conflict). Psychache (Schneidman) • Schneidman (1985) developed the concept of “Psychache” – losses that can lead to intense emotional pain – – – – – – – – – – – – Rejection Worthlessness Hopelessness Helplessness Grief Anger Frustration Shame Isolation Loneliness Despair failure Suicide and Alcohol 35-80% of all suicidal behaviour is said to be alcohol related. Experiences of Suicide • • • • • • • • • Increased tension Unpleasant affect Disorganised behaviour Cognitive confusion Inability to resolve conflict Maladaptive problem solving Perceptual distortion Confusion and disorganisation Agitation. Anger, worthlessness Risk Factors • Predisposing – historic, static • Acute – current and dynamic • Protective Predisposing Risk factors • Demographic - male, older age, ethnicity, marital status, economic, employment • • • • Diagnosis of mental disorder Previous suicidal behaviour History of aversive life events Dispositional –maladaptive personality characteristics, emotional instability, poor resilience/coping skills Acute Risk Factors • Precipitant social stressors – loss of resources or status, interpersonal discord, legal or financial difficulties • Current mental state – hopelessness • Current engagement/compliance with professional support and treatment Protective Factors • Only a few have been identified • Many are inversions of risk factors • Those identified include: – – – – Positive coping strategies Effective problem solving skills General life satisfaction Resilience Suicide Prevention– areas of focus • • • • • Assessment and treatment of psychiatric disorders Detection and treatment in primary care Reducing access to lethal means Reducing inequalities in disadvantaged groups Increasing availability of psychological therapies Suicide and Mental Disorder While there is no doubt that the causes of suicide are multiple and complex, we must be aware of the increased risk of suicide associated with mental disorders: • Borderline Personality Disorder – 45 times increased risk • Depression - 20 times increased risk • Bipolar Affective Disorder – 17 times increased risk • Opioid use – 14 times increased risk • Anorexia Nervosa – 31 times increased risk • Alcohol misuse or dependence – 16 times increased risk The conclusion?? – We MUST assess for underlying psychiatric disorder Identifying Psychiatric Disorder – Benefits • By identifying psychiatric disorders we can: – Target evidence-based therapies aimed at preventing suicide and self-harm and wellbeing – Examples include: • DBT for BPD reduces self-harm and hospitalisation • Clozapine and other second generation anti-psychotics reduce suicide in Schizophrenia • Lithium reduces suicide in Bipolar Affective Disorder Suicide Prevention in Populations • Population based programs aimed at suicide prevention must include: – Public education – Means prevention – Improved assessment – Improved treatment – Targeted programs for specific populations Suicide Prevention – A Three Tiered Approach • Reducing suicide in any population requires a focus in the following three areas: 1. Capacity in communities 2. Recognition of those at risk 3. Post discharge and community-based care Tasmanian Context • Tasmanian Suicide Prevention Strategy 2010-2014 was launched in December 2010. • The Minister recently approved an extension of the Strategy until December 2015. • The Tasmanian Suicide Prevention Committee provides high level strategic advice and leadership in suicide prevention activities in Tasmania, with a focus on implementing the strategy. • The Tasmanian Suicide Prevention Community Network is hosted by Relationships Australia (Tasmania) and funded by the Directorate to enable key stakeholders and service provides to work collaboratively across the state to address suicide prevention. Suicide in Tasmania - 2012 • Tasmanian age-standardised suicide death rate – 14.1/100,000 • NT – 18.1; WA – 13.5; QLD - 13.0 • 70 deaths by suicide in Tasmania in 2012 (33 from transport accidents) • 56 male deaths and 14 female deaths • The female suicide rate is the highest among all states and territories and higher than the national average of 5.1/100,000 • The male suicide rate is the second highest in Australia. • Most suicides occur in the areas of greater population, but males have a higher rate of suicide in rural areas. Approaches to Prevention The elements of the approach to suicide prevention in Tasmania include a range of initiatives under the current strategy. The following are some new initiatives aimed at further developing and enhancing our approach: 1. Assisting communities with the implementation of community action plans to prevent suicide. 2. Establishing early intervention referral pathways following suicidal behaviour or self-harm 3. Delivering suicide prevention awareness training to persons in key occupations. Approaches to Prevention cont. 4. Ensuring Tasmanian researchers can access in-depth analysis of Tasmanian suicides to better target prevention strategies. 5. Developing a targeted Youth Suicide Prevention Strategy for Tasmania with the Youth network of Tasmania 6. Analysis of suicide “hotspots” to mitigate risk at places of repeated suicides. 7. Ensuring that clinical risk categorisation processes are developed to aid in the early identification of those at high risk and to inform plans for the management of those at high risk. Community Action Plans • • • • In line with current directions Working through organisations such as Relationships Australia Aimed at enhancing social connectedness of community members Enabling communities to respond appropriately to people showing signs of distress, mental ill health or suicidal intent • Providing access to available support services Early Intervention Referral • Establishing referral pathways for early intervention is vital to both prevent the behaviour and to deal with the underlying causes. • Not everyone who attempts or considers suicide requires hospitalisation, but all require professional assessment, support and follow up. • Models aimed at ensuring effective follow-up for patients following an episode of self-harm or a suicide attempt to support discharge to early intervention and other support services need to be developed and implemented in DEMs and public mental health in-patient settings. Suicide Prevention Awareness Training • We wish to identify the suicide prevention training needs within Tasmania and commission training providers to deliver suicide prevention training to key occupations and sectors. • This training will target a number of important “gatekeepers” – people in positions to become aware of those in distress including: • GPs, Sporting bodies (coaches etc), churches, hairdressers, refuges, any services directed at those suffering with problems, OH&S representatives. Research • More research is needed to allow in-depth analysis of Tasmanian suicides to better target prevention strategies. • The Directorate is working closely with the Tasmanian Coroner to establish a new Tasmanian Suicide Register which will provide researchers with vital data upon which to base recommendations for prevention strategies.This would be a valuable tool in prevention giving us niche data in an accurate and timely manner. • Such a register will attempt to capture an individual’s story prior to suicide including the factors unique to their environment and gather information such as service contacts in the time leading up to the person’s death. Youth Suicide Prevention Strategy • A youth suicide prevention strategy will aim at building resilience in youth and encouraging and developing help seeking behaviours. • The strategy is being developed in partnership with the Youth Network of Tasmania (YNoT). • Success in this endeavour is very strongly aligned to the ability to consider and include the views of the youths themselves. • Throughout Australia, suicide remains the leading cause of death within the 15-24 year old age bracket. • A statewide forum to discuss youth suicide will be held in Launceston on 20 March 2015. Youth Suicide Prevention Strategy cont. • Youth suicide prevention strategies include: • • • • • • Developing internal positive coping strategies Assistive social supports Assisting in the development of self esteem Social support and connectedness Accessing professional support for assistance Removing access to means of suicide Suicide “Hotspots” • Research has demonstrated that there are a number of specific, accessible and usually public sites that are frequently used as a location for suicide – these become known as so called “hot-spots”. • Hot-spots include tall structures (bridges, cliffs), railway tracks and isolated locations (rural car parks) which offer direct means for suicide or seclusion that prevents intervention. • Establishing a cross-agency group including representatives from Health, Police, Ambulance, the Coroner and the Department of Infrastructure will enable any “hotspots” in Tasmania to be identified and options for mitigating suicide at such places developed. Clinical Risk Categorisation • This provides clinicians with a formulation that a person is at high, moderate, low or no foreseeable risk of an outcome – in this context – suicide. • The risk judgement is based upon a structured, transparent clinical process. • It leads to the development of a management plan based upon the formulation and enables monitoring of the risk and the effects of the management plan. Clinical Risk Categorisation • All clinicians involved in the care of people with mental health problems should be aware that assessment of risk is a required skill. • While suicide prevention is the concern of the whole community, clinicians have an ongoing role in the management and monitoring of identified risk. • Risk assessment involves an examination of both static and dynamic factors including gender, age, previous history, current mental state, social situation, impulsivity, treatment availability – all in the context of the person and their environment. Questions