Overview of Coding and Documentation

Overview of Coding and Documentation
Initial Steps
Evaluate and monitor the patient
Treat the patient
Document the service
Code the service
Document the Service
Document all services/procedures rendered to a patient in the EMR
Remember: if you did not document it, you did not do it and it cannot be paid
Documentation Guidelines
Your documentation must support your services
Teaching Physician guidelines – government payors have strict guidelines regulating when a physician bills with a Resident’s involvement
Florence is rewriting
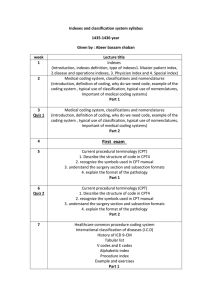
The HCPCS coding system consists of two levels
Level I – Current Procedural Terminology (CPT)
Codes
Developed and maintained by the AMA
Consist of five-digit codes and two-digit modifiers
Level II – HCPCS National Codes
Developed by CMS and maintained by a national panel
Consist of one alpha character followed by four-digits
Also have modifiers
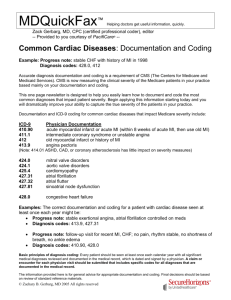
ICD-9-CM: International Classification of Diseases, Ninth Revision, Clinical
Modification
ICD-9 coding is a classification system that arranges diseases and injuries into groups according to established criteria
ICD-9 is based on the World Health Organization’s Ninth
Revision, International Classification of Diseases
Code changes are made annually by the government and are effective October 1 – September 30
All CPT codes submitted to payors must have an accompanying ICD-9 code(s)
Effective October 2014 ICD-10 replaces ICD-9 – THE
WORLD CHANGES DRAMATICALLY!!!!!
General Principles of Documenting -
Florence
The medical record should be complete and legible
The documentation of EACH patient encounter should include:
Date;
Reason for the encounter;
Appropriate history and physical exam;
Review of lab, x-ray data, and other ancillary services (where appropriate);
Assessment; and
Plan of care (including discharge plan, if appropriate)
General Principles of Documenting -
Florence
Patient’s progress, including response to treatment, change in diagnosis, and patient noncompliance;
Relevant health risk factors;
Written plan of care should include (when appropriate):
Treatments and medications, specifying frequency and dosage;
Any referrals and consultations; and
Patient/family education
General Principles of Documenting
Documentation should support the intensity of the evaluation and/or treatment, including thought processes and complexity of medical decision making;
All entries should be dated and authenticated by physician signature; and
The CPT/ICD-9-CM codes reported on the CMS-
1500 should reflect the documentation in the medical record.
CPT Coding and Documentation
E&M Services – (Evaluation and Management Services)
Levels of Care
E&M Documentation
CMS/AMA Guidelines
E&M Coding
Key Components
History
Exam
Decision Making
Contributory Factors
Counseling
Coordination of care
Presenting problem
Time
Key Components
History
Exam
Decision Making
History
Chief Complaint (CC)
History of Present Illness (HPI)
Review of Systems (ROS)
Past, Family & Social History (PFSH)
Exam
Organ Systems
For a General Multi-System Exam
Body Areas
Medical Decision Making
Complexity of establishing a diagnosis
The number of diagnoses or management options;
The amount and complexity of data ordered or reviewed; and
The risk of complications and morbidity/mortality.
Why Focus on Documentation
Physician documentation is the basis for the hospital coding.
Accurate and complete medical record documentation is critical to reflect the high quality of care provided by the medical staff.
The documentation in the medical record is the key driver of the quality outcome scores for the hospital.
Inadequate documentation can lead to a misrepresentation of the quality of care provided by the facility.
Documentation Basics
All diagnoses and conditions that are monitored, evaluated and/or treated during the hospital stay should be documented
Diagnosis must be stated in codeable terminology ( ICD 9 codes) to be included in the coding process .
Importance of Documentation
Capturing the appropriate diagnosis and condition is critical for:
Accurate severity of illness and risk of mortality reporting.
Compliance with CMS rules and regulations.
Appropriate reimbursement for the care provided.
Supporting length of stay and resources utilized.
Preparation for bundled payments and value based purchasing (VPB).
Support of physician billing.
Examples of Unable vs Acceptable
Low Hgb, transfuse
Hypertensive emergency, urgency, crisis
Urosepsis, change foley
COPD, home O2
CHF
Air space disease
Thin, low prealbumin
Unresponsive
Skin breakdown
Replete lytes, low Na, K+
Specify type of anemia
Malignant or accelerated hypertension.
Sepsis secondary to UTI
Chronic respiratory failure
Type of pneumonia
(organism), CAP, HCAP
Type of malnutrition
Coma
Pressure ulcer
Hyponatremia, Hypokalemia
Specificity of Diagnosis
Anemia – low
Acute blood loss anemia - moderate
Pancytopenia secondary to chemo - high
CHF – low
Chronic systolic or diastolic heart failure - moderate
Acute systolic or diastolic heart failure – high
Respiratory insufficiency – low
Chronic respiratory failure – moderate
Acute respiratory failure - high
Specificity of Diagnosis
Poor nutritional status – low
Mild or moderate malnutrition – moderate
Severe malnutrition – high
Renal insufficiency – low
Acute renal failure or injury – moderate
Acute renal failure secondary to ATN – high
GCS, unresponsive – low
Coma - high